Spontaneous bilateral chronic subdural haematoma in an 8-month-old male with osteogenesis imperfecta: A case report
Ubong U. Ekpene1, Enono E. Uduehe1, Imoh Isobara2, Ned Ndafia1
Abstract
Osteogenesis imperfecta is a rare inherited collagen disease that presents most commonly with increased bone fragility. We present an 8-month-old male child with a 5-month history of progressive abnormal increase in the size of the head and a history of multiple long bone fractures not preceded by trauma and blue sclerae.
Cranial CT scan showed bilateral frontoparietal chronic subdural haematoma. X-rays of the limbs showed healed left humeral and right femoral fractures.
He underwent bilateral burrhole and drainage of haematoma with a good postoperative outcome.
Osteogenesis imperfecta with spontaneous bilateral chronic subdural haematoma is rare, thus informs this case report.
Key words: Osteogenesis imperfecta, Bilateral Chronic Subdural haematoma, genetic collagen disorder, case report.
Introduction
Osteogenesis imperfecta (OI) is a rare inherited collagen disease characterized by a group of disorders that is most commonly associated with increased bone fragility, with resultant multiple fractures, amongst other clinical manifestations. It is caused mainly by mutations affecting 2 genes, COL1A1 and COL1A2 that code for collagen type 1,1 thus, its clinical manifestations affect the bones, ligaments, tendons, skin and sclera, which are composed of these collagens. In its mild form it can present with blue sclerae, but severe types can present with growth retardation, cardiovascular anomaly, spine and limb deformities.
Vrolik coined the term osteogenesis imperfecta in 1849.2 Lobstein had first described it in 1833 and called it osteopsathyrosis idiopathica and was one of the first to correctly understand the etiology of the condition.2 Osteogenesis imperfecta has been known by other names in the past namely: fragilitus osseum, Lobstein disease, brittle-bone disease, blue-sclera syndrome, and fragile-bone disease.
This condition affects 1 in 10,000 - 20,000 birth.3,4 It can be classified based on clinical course into 5 types, namely: nondeforming with persistently blue sclerae (OI type 1), perinatal lethal form (OI type 2), progressively deforming type (OI type 3), moderate form (OI type 4), and Osteogenesis imperfecta with calcification of the interosseous membranes and/or hypertrophic callus (OI type 5), and genetically into 30 classes.5 Its mode of inheritance is mostly autosomal dominant and to a lesser extent, autosomal recessive.5
In the more easily recognized type, affected individuals present with blue sclera, and a predisposition to tubular bone fractures following relatively minor trauma, with bowing of the legs. Other presentations include: dental abnormalities, joint hypermobility, and neurological manifestations like hearing loss and seizures.6 Neurosurgical conditions may also occur and include: intracranial haematomas, hydrocephalus, macrocephaly, basilar invagination, and spinal fracture.7
Spontaneous bilateral chronic subdural haematoma in an infant with osteogenesis imperfecta is an extremely rare condition. It is shown to be caused by a genetic mutation in collagen formation with resultant bone fragility from abnormal bone calcification, vascular fragility and permanent friction between multiple bone fragments of the skull.6 The increased risk of intracranial haematoma in OI patients also have been attributed to platelet dysfunction8 and weakness of the skull.9
Spontaneous Subdural haematoma was first reported in an infant with osteogenesis imperfecta by Tokoro et al in 19889. Since then, a few more cases have been reported by several authors.6,7,9-14 Most of the reported cases occurred in children,6,7,9-11 while 3 cases were reported in adults, all of whom had additional predisposing conditions (alcohol abuse, uraemia and spontaneous intracranial hypotension).12-14 Treatments for the subdural haematoma included non-operative treatment, burr hole and drainage, or craniotomy and evacuation of haematoma depending on the age of the haematoma. Considering how rare the condition is, and with only few case reports and case series published in the English literature, this report aims at adding to the existing body of literature. To the best of our knowledge, this is the first report of this condition in our sub region and possibly in Africa.
Case Report
This is the case of an 8-month-old male infant with 5 months history of progressive abnormal increase in the size of the head and delayed developmental milestones. There was no history of head trauma, neither fever nor use of anticoagulants. Pregnancy history, perinatal and neonatal history were unremarkable. He was seen 3 months earlier by the paediatrician and orthopaedic surgeon on account of fractured left humerus and right femur while being bathed by the mother. The diagnosis of Osteogenesis imperfecta was first made based on clinical and radiological findings. There was no clear family history of similar condition.

Fig. 1: Triangular shaped face with frontal bossing

Fig. 2: Blue Sclera
Physical examination revealed macrocephaly with an Occipitofrontal circumference of 46.5cm, triangular shaped face with frontal bossing (Fig. 1). He had blue sclerae (Fig. 2).
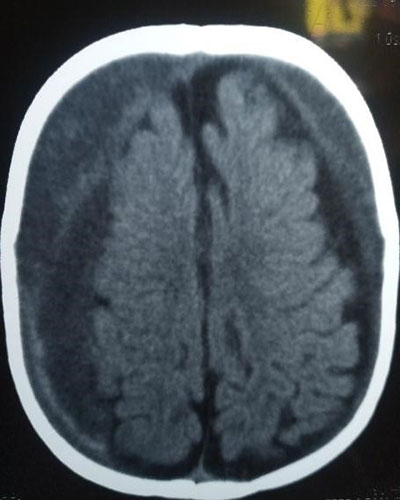
Fig. 3: bilateral frontoparietal fracture chronic subdural haematoma

Fig. 4: Left healed Humeral fracture
Cranial CT scan showed features in keeping with bilateral frontoparietal chronic subdural haematoma (Fig. 3). X-rays of the limbs showed healed left humeral fracture (Fig. 4) and right femoral fracture with bilateral bowing of the tibia (Fig. 5). Echocardiography showed a small membranous ventricular septal defect. Full blood count, clotting profile and Liver function test results were normal.

Fig. 5: Right healed femoral and bilateral bowing of the tibia
He had bilateral burr hole and drainage of the haematoma with a good postoperative recovery, and was subsequently discharged home. Follow up in clinic was uneventful for up to two months before patient was lost to follow up without carrying out the requested post operative cranial CT scan.
Discussion
Several case reports,6,9,11-14 and case series7,10 on subdural haematomas associated with osteogenesis imperfecta have been published. However, Spontaneous bilateral chronic subdural in an OI patient is very rare. A literature search only revealed five of such reported cases.6,7,10,13 Four were in children,6,7,10 and one in an adult.13 There were also reported cases of unilateral subdural haematoma: four in children,7,9,10,11 and two in adults.12,14
The increased tendency for intracranial bleed is shown to be due to bone fragility from abnormal bone calcification, vascular fragility and permanent friction between multiple bone fragments of the skull.6,15 Haematological derangements like decreased platelet retention and reduced factor VIII R:Ag were major contributors to intracranial bleed, while reduced ristocetin cofactor, deficient platelet aggregation induced by collagen and prolonged bleeding time were less common findings.16
Although OI has a genetic basis with both autosomal dominant and recessive mode of inheritance, some cases may be sporadic without any traceable family history as in the index case. In most cases in the paediatric population, as in the index case, there is usually no clear history of head trauma, but in some there may be a history of minor trauma to the head.7,10 Adults who present with subdural haematoma tend to have other associated risk factors like alcohol abuse and Aspirin use, uraemia and spontaneous intracranial hypotension.11-13
Faqeih et all noted a prevalence of intracranial bleeding of 1% among a cohort of 400 patients with OI, two of which were SDH and one each of epidural and intracerebral haematoma.9 In addition, the authors found that all 4 patients had glycine mutations in the C-terminal collagen type 1 alpha triple helix, leading the authors to conclude that there may be an association between the presence of this mutation , limb anomalies and increased tendency for intracranial bleeding among patients with OI.9
In a review of 10 children with OI by Sasaki-Adams et al,7 seen over a 19-year period at a single neurosurgical centre, the most common neurosurgical conditions encountered in this cohort included macrocephaly in 5 patients, subdural hematoma in 3 patients, epidural hematoma in 2 patients, and hydrocephalus in 3 patients. 20% of the cohort had Basilar invagination and spinal fractures. Some patients were treated nonoperatively, while several required craniotomies for clot evacuation, decompression, and spinal fixation for fracture or basilar invagination, and Ventriculoperitoneal shunt insertion for the hydrocephalus. The index case required bilateral burr hole and drainage with a good postoperative outcome. Sayre et al reported a mortality following surgery for drainage of the subdural haematoma in a 29-year-old with co-existing renal failure.12
Medical treatment with Bisphosphonate has been shown to be effective in reducing the risk of further fractures. This was not given to the child due to financial constraint in the family.
Conclusion
Bilateral chronic subdural haematoma is a rare neurosurgical condition that affects patients with Osteogenesis Imperfecta. There should be a high index of suspicion in any OI patient who presents with macrocephaly, delayed developmental milestone or any other neurologically related symptoms and signs earlier mentioned in the literature review. This subdural haematoma can easily be diagnosed with a cranial CT scan. Treatment with burr hole can be lifesaving with a good outcome.
References
- Marom R, Rabenhorst BM, Morello R. Osteogenesis imperfecta: an update on clinical features and therapies. Eur J Endocrinol. 2020; 183(4): R95-r106.
- Robichon J, Germain JP. Pathogenesis of osteogenesis imperfecta. Can Med Assoc J. 1968; 99: 975–979.
-
Martin E, Shapiro JR. Osteogenesis imperfecta: epidemiology and pathophysiology. Current osteoporosis reports. 2007; 5(3): 91-7.
-
Forlino A, Cabral WA, Barnes AM, Marini JC. New perspectives on osteogenesis imperfecta. Nat Rev Endocrinol. 2011; 7(9): 540-57.
-
Mortier GR, Cohn DH, Cormier-Daire V, Hall C, Krakow D, Mundlos S, et al. Nosology and classification of genetic skeletal disorders: 2019 revision. Am J Med Genet A. 2019; 179(12): 2393-419.
-
Anja G, Jörg S, Martina M, Ertan M, Thorsten R. Subdural hematoma as clinical presentation of osteogenesis imperfecta. Pediatr Neurol. 2005 Feb; 32(2): 140-2. doi: 10.1016/j.pediatrneurol.2004.07.011.
-
Sasaki-Adams D, Kulkarni A, Rutka J, Dirks P, Taylor M, Drake JM. Neurosurgical implications of osteogenesis imperfecta in children. Report of 4 cases. J Neurosurg Pediatr. 2008; 1(3): 229-36.
-
Hathaway WE, Solomons CC, Ott JE. Platelet Function and Pyrophosphates in Osteogenesis Imperfecta. Blood. April 1972; 39(4): 500-509.
-
Tokoro K, Nakajima F, Yamataki A. Infantile chronic subdural hematoma with local protrusion of the skull in a case of osteogenesis imperfecta. Neurosurgery. 1988; 22(3): 595-8.
- Faqeih E, Roughley P, Glorieux FH, Rauch F. Osteogenesis imperfecta type III with intracranial hemorrhage and brachydactyly associated with mutations in exon 49 of COL1A2. American journal of medical genetics Part A. 2009; 149A(3): 461-5.
- Dinca EB, Carron R. Beware of Osteogenesis Imperfecta: Subdural Hematoma in a 10-Year-Old Child With Minor Head Trauma. The journal of nervous and mental disease. 2019; 207(7): 575-6.
- Sayre MR, Roberge RJ, Evans TC. Nontraumatic subdural hematoma in a patient with osteogenesis imperfecta and renal failure. The American journal of emergency medicine. 1987; 5(4): 298-301.
- Eddeine HSMD, Dafer RMMDMPH, Schneck MJMDFF, Biller JMDFFF. Bilateral Subdural Hematomas in an Adult with Osteogenesis Imperfecta. Journal of stroke and cerebrovascular diseases. 2009; 18(4): 313-5.
- Rezazadeh A, Hollensead SC, Laber DA, Kloecker GH. Intracranial Hemorrhage in a Patient with Osteogenesis Imperfecta Due to Inherited and Acquired Platelet Dysfunction. Blood. 2006; 108(11): 3960.
- Albayram S, Kizilkilic O, Yilmaz H, Tuysuz B, Kocer N, Islak C. Abnormalities in the cerebral arterial system in osteogenesis imperfecta. Am J Neuroradiol. 2003; 24(4): 748–750.
- Evensen S A, Myhre L, Stormorken H. Haemostatic studies in osteogenesis imperfecta. Scand J Haematol. 1984; 33(2): 177–179.