Impact of canalplasty on the surgical outcomes of type-1 tympanoplasty: experience in a tertiary care teaching hospital
Saumya Ranjan Das1, Prasenjit Baliarsingh1, Biplob Bhattacharyya1, Somadatta Das2, Rabindra Nath Padhy3
Abstract
Context: Canalplasty restores the normal width and shape of the external auditory canal (EAC) for passage of sound. It is required as a co-surgical procedure with tympanoplasty in some cases; where the entire tympanic membrane and anulus cannot be seen during surgery due to the bony overhang or narrowing.
Objective: The aim of the study was to determine the surgical outcome of canalplasty in patients with CSOM undergoing type-I tympanoplasty. Widening of the external auditory canal, called canalplasty helps in a better placement of the tympanic membrane graft with a better visualization and with a correct understanding of the effect of canalplasty on the outcome of type I tympanoplasty.
Methods: A total of 110 patients diagnosed with chronic otitis media mucosal disease with a central dry perforation involving the tympanic membrane were included. The group A included 55 cases that underwent tympanoplasty with canalplasty; while the group B with 55 cases underwent tympanoplasty without canalplasty.
Results: Analysis was done for graft uptake, hearing improvement and time taken for the postoperative recovery. In terms of graft uptake, both groups achieved a success rate of 98.2%. The improvement in postoperative hearing in cases with canalplasty was statistically significant p<0.05. Time taken for complete postoperative recovery in the two groups was statistically insignificant.
Conclusion: Anatomical and technical factors diversely affect the functional outcome of tympanoplasties. Canalplasty helped in a better visualization and placement of the graft. Time spent on drilling in canalplasty was compensated by the time gained in grafting of the neo-tympanum. The procedure prevented graft lateralization due to the accurate exposure of the annulus. Postoperative care was easier in cases of tympanoplasty with canalplasty.
Keywords: Canalplasty, Surgical outcomes, Tympanoplasty, Chronic suppurative otitis media
Introduction
The special anatomical features and the acoustic quality of tympanic membrane play a role in the hearing mechanism. The grafting of the perforated tympanic membrane and reconstruction of the ossicular chain are performed surgically in tympanoplasty, as any perforation causes hearing problems. Indeed, the tympanoplasty type-1 refers to a surgical procedure to seal a perforated tympanic membrane.1 Several graft materials are mainly used to close the tympanic membrane perforations, such as temporalis fascia, cartilage, perichondrium, periosteum, dura mater, vein, fat, and skin.2 It is a safe and effective procedure used to eradicate repeated inflammations of the middle ear and to restore hearing with the middle ear function. Moreover, preoperative assessment, desirable intraoperative hemostasis, and thoughtful surgical planning with the careful placement of the graft are the factors that affect the success of the surgery.3
Secondly, the external auditory canal (EAC) is restored to its natural width and form by the procedure known as canalplasty. It is necessary in conjunction with tympanoplasty in certain circumstances because the bony overhang or constriction prevents the surgeon from seeing the full tympanic membrane and annulus during surgery. Moreover, its role is beneficial for postoperative care. Indeed, other indications of canalplasty include congenital stenosis, exostosis, obliterative external otitis, and tumors of EAC and keratosis obturans.4
Methods
This comparative prospective study was conducted from November 2018 to October 2020 with patients having chronic suppurative otitis media (CSOM) presenting at the department of ear, nose, and throat. The study consisted of two groups: Group A: Tympanoplasty with canalplasty and Group B: Tympanoplasty without canalplasty. Group A consisted of patients with CSOM having perforated tympanic membrane and narrow-bony external auditory canal (Figure 1A); whereas Group B had CSOM patients having perforated tympanic membrane and wide bony external auditory canal (Figure 1B). Patients with inactive stage of CSOM in the age group 15-60 years and having pars tensa perforation of tympanic membrane for more than three weeks were included in this study; on the other hand, patients having CSOM with attico-antral disease, active stage of the disease, pars tensa perforation of less than 3-week duration, complications of CSOM, mixed or sensorineural hearing loss, systemic illness and pregnancy were excluded. Patients selected for type 1 tympanoplasty with or without canalplasty were admitted to the inpatient department. Pre-operative pure tone audiometry (PTA) was performed as baseline hearing assessment for all patients. The underlay method of tympanoplasty by post-auricular approach was followed. Cases of CSOM with circumferential or segmental narrowing of bony external auditory canal causing poor visibility of the tympanic membrane and/ or the tympanic annulus were selected for canalplasty. In these cases, canalplasty was performed by widening the bony external auditory canal with the help of a micro-drill, followed by grafting the tympanic membrane and repositioning the tympanomeatal flap (see Figure 1C,D).
At the first follow-up at the end of 6 weeks, along with the suction cleaning of the ear canal, the tympanic membrane was examined for graft uptake status; eventually, after three months, pure tone audiometry (PTA) was undertaken to assess the hearing improvement. After six months, both parameters were checked to see whether the improvement was retained in the long run.
Results
There were 72 female (65.45%) and 38 male (34.55%) subjects in the study who underwent either of the two procedures. Among them, more males underwent type 1 tympanoplasty with canalplasty (21 out of 38 males, 55.26 %), while more females (38 out of 72 females, 52.78%) underwent type 1 tympanoplasty alone. PTA of all patients showed that most subjects, and in each group, had a hearing loss of 26-40 dB (mild hearing loss). The mean hearing loss values of groups A and B were 39.78 ± 12.86 and 38.47 ± 9.37 dB, respectively. The distribution of pure tone audiometry was normal for group B (p=0.198, data not shown), but for group A, it was non-normal (p<0.001, data not shown). There was no statistically significant difference across the hearing loss groups by type of surgery (p=0.501) [Table 1].
Table 1: Baseline pure tone audiometry among study subjects by type of surgery (n=110, 55 in each group)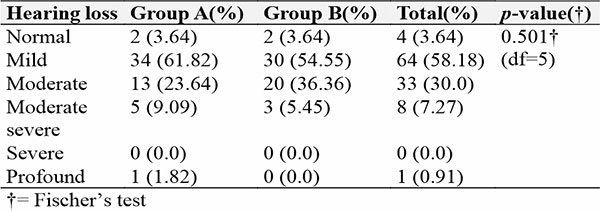
The graft uptake was seen in 108 (98.2%) cases (54 in each group, 98.2% each) at the first visit. There was no statistically significant difference in the proportion of subjects who had graft uptake (p=1.00). PTA at the third visit had a mean change of 21.27 ± 6.32 dB and 22.03 ± 5.77 dB in groups A and B, respectively [Table 2]. The distribution was non-normal for both Group A and B (p<0.05). A comparison of median changes in PTA between the groups showed that there was no statistically significant difference (p=0.204).
Table 2: Hearing improvements in pure tone audiometry at third visit compared to baseline among two study groups (n=110, 55 in each group)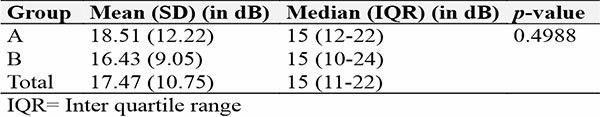
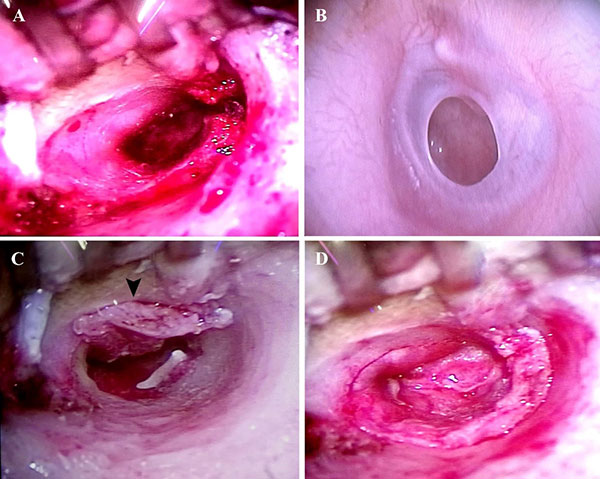
Figure 1. Intra-operative microscopic view of the left ear:
A. Narrow external auditory canal.
B. CSOM left ear with perforated tympanic membrane instead of the flap
C. Widened bony EAC with elevated tympanomeatal flap (arrowhead) after canalplasty.
D. EAC and neo-tympanic membrane (grafted) after type 1 tympanoplasy with canalplasty.
Discussion
A total of 110 subjects (55 in each group) were used for data analysis; having an equal number of study subjects in both groups ensured that both groups were comparable. The mean age of the study population was 31.85 ± 11.45 years (min 15 years, max 55 years). Both groups had subjects with median ages that were not significantly different from each other (p=0.528). It could be concluded that the matching for age of patients was ensured, and both groups were similar as per age of patients. Thus, the groups were similar in terms of gender distribution. PTA showed that most of the subjects in each group, had a hearing loss of 26-40 dB (mild hearing loss). The mean hearing loss for Groups A and B was 39.78 ± 12.86 and 38.47 ± 9.37 dB, respectively. There was no statistically significant difference across the hearing loss groups by type of surgery (p=0.501). Thus, the subjects undergoing tympanoplasty alone were no different from those undergoing tympanoplasty with canalplasty. At the first visit, graft uptakes were seen in 108 (98.2%) cases (54 in each group, 98.2% each). There was no statistically significant difference in the proportion of subjects who had graft uptake (p=1.00) by the type of surgery. PTA at the third visit had a mean change of 21.27 ± 6.32 dB and 22.03 ± 5.77 dB in groups A and B, respectively. Comparison of median changes in PTA at 3rd visit between the groups showed no statistically significant difference (p=0.204). Thus, both procedures produced equal results in terms of hearing improvement. Improvement beyond three months was negligible (p>0.05). Hence, an initial three-month assessment can conclude the degree of hearing improvement that the subjects finally had after surgery and might not be repeated at six months without any further complaints from the subjects. A comparison of median changes in PTA between the groups showed no statistically significant difference (p=0.4988). Thus, the hearing improvement is almost equal in both the groups of subjects undergoing either type 1 tympanoplasty alone or along with canalplasty. However, studies concluded that canalplasty gives 9 dB gain in hearing compared to those without canalplasty, which was not seen in this study.5 Similarly, a study showed a statistically significant improvement in hearing loss in cases where canalplasty was done in addition to tympanoplasty, which was not seen in this study.6 The present study was a matched comparative study. Similar to the studies by Chandra et al. 2009 and Salvador et al. 2020, the decisions for canalplasty in the present study were taken intraoperatively during microscopic surgery for cases of CSOM having narrowed of the bony external auditory canal with difficulty in the visualization of the whole tympanic membrane.7,8
Conclusions
Herein, Type 1 tympanoplasty done alone or combined with canalplasty produced hearing improvements of 21-22 dB. Thus, it could be at the discretion of the operating surgeon to decide if a canalplasty is needed in addition to the tympanoplasty since the outcomes of the surgery in terms of hearing improvement will not be altered by either procedure. Graft uptake at six months was found to be similar in both groups (98.2%), and there was statistically no significant difference between the groups. Thus, canal narrowing could mostly be a reason to undertake canalplasty in addition to tympanoplasty; it could be concluded that a decision by the surgeon to undertake type 1 tympanoplasty alone or in combination with canaloplasty could be taken without affecting the outcome of the surgery in terms of hearing improvement or graft uptake.
Conflicts of Interest
All the authors report no conflict of interest.
Funding
No funding was received for this study
References
- Zollner F. Panel on myringoplasty (2nd workshop on Reconstructive middle Ear Surgery). Arch Otolaryngot 1963;78:301-302.
- De Seta E, Covelli E, De Seta D, Mancini P, Filipo R. Cartilage tympanoplasty; how to reduce surgery time. J Laryngol Otol 2010;124:784-5. DOI: 10.1017/S0022215110000344
- Reilly B. Tympanoplasty: Background, Pathology, Indications. Medscape 2016; 1-6.
- Jung TTK. Canalplasty. Operative techniques in Otolaryngology-head and neck surgery 1996;7(1): 27-33. DOI: https://doi.org/10.1016/S1043-1810(96)80058-3
- Vijayendra H, Ittop CJ, Sangeetha R. Comparative study of hearing improvement in type 1 tympanoplasty with and without canalplasty. Indian J Otolaryngol Head Neck Surg 2008;60(4):341-4.DOI: 10.1007/s12070-008-0113-y
- Prakash MD, Badkar P. Effect of canalplasty in tympanoplasty. Int J Otorhinolaryngol Head Neck Surg 2018;4(4):1049. DOI: http://dx.doi.org/10.18203/issn.2454-5929.ijohns20182711
- Chandra TS, Murthy PSN, Sreenivasulu M, Jyothirmai ASL. A Study on Correlation of External Auditory Canal Dimensions and Endoscopic Tympanoplasty in a Tertiary Health Care Centre. Int J Contemp Med Res 2019;6(4):5-7. DOI: 10.21276/ijcmr.2019.6.4.48
- Salvador P, Gomes P, Silva F, Fonseca R. Type I Tympanoplasty: surgical success and prognostic factors. Acta Otorrinolaringol ESP 2020. https://doi.org/10.1016/j.otorri.2020.04.009