Evaluation of cosmetic outcome and patient satisfaction following adhesive strips and staples wound closure in primary total knee arthroplasty
Ubong E Essien1, Chukwuemeka M Obi2, Udoinyang Inyang3, Aniebiet Ubaha4
Abstract
Background: Most surgical wound closure techniques include using materials that may require removal after surgery. Surgical skin sutures and staples are popular skin closure materials that require removal after surgery and are usually associated with patient discomfort and crosshatching of the skin.
Adhesive strips are a newer, non-invasive technique for skin closure in orthopaedic procedures, and they have been documented to have fewer wound-related complications.
The cosmetic scores of surgical scars can be assessed by the Hollander Wound Evaluation Score (HWES), the visual analogue scale (VAS), and the numeric rating scale (NRS).
Objective: Patient satisfaction with surgical scars between adhesive strips and skin staples was compared via the Hollander wound evaluation score, visual analogue scale score, and Numeric rating scale score. To compare wound cosmesis between adhesive strips and skin staples using the Hollander wound evaluation score and visual analogue score. To compare pain on removal of wound closure material using the numeric rating scale.
Method: Group A received skin closure with adhesive strips, whereas Group B received skin closure with staples. In week 2, the assessment of discomfort from removing coaptive material for patients in groups A and B was performed using the numeric rating scale score. At week 6, the surgical scar was assessed using the VAS score and the HWES. The outcome measures were scar cosmesis and pain score on the removal of skin closure material.
Results: There was a statistically significant difference in the NRS score with participants in the adhesive strip group having a lower score, with a P value of 0.000 (<0.05). The VAS score and HWES were higher in the adhesive strip group than in the skin staple group, with a P value of 0.000 (<0.05).
Conclusion: Patients in the adhesive strip group experienced less pain and discomfort at strip removal and were more satisfied with their scars. The cosmetic scores for scars in the adhesive strip group were significantly higher than those in the skin staple group.
Keywords: Adhesive strips, Staples, Hollander wound evaluation score, Numeric rating scale, Primary total knee arthroplasty
Introduction
Orthopaedic surgery utilizes different skin closure techniques, each selected to optimize healing, reduce infection risks, and achieve a cosmetically satisfactory scar.1 A scar is a distortion in the normal structure and function of the skin architecture resulting from a healed wound.2 The method of wound closure in total knee arthroplasty is a major aspect of the surgery, as it influences the overall outcome and patient satisfaction.1,3 While there is no ideal technique for skin closure, surgical sutures, and skin staples are popular skin closure techniques in total knee arthroplasty. These materials require removal after surgery and are usually associated with problems such as patient discomfort and crosshatching of the skin.
Adhesive strip application is a newer, non-invasive technique for skin closure in orthopaedic procedures.3 Adhesive strips consist of porous, non-woven rayon material reinforced with polyester filaments for strength and coated with a hypoallergenic adhesive.4 Adhesive strips have been documented to have fewer wound-related complications as the closure material does not breach the skin.5,6
Surgical scars can be assessed through objective or subjective tools. Objective assessment requires devices to measure features such as colour, thickness, relief, pliability, and surface area whereas subjective tools provide a qualitative measurement by a patient or clinician.7 These objective and subjective tools are useful in assessing scars at different intervals during the postoperative period and monitoring their progress.2 There is currently no gold standard in scar assessment tools.8,9
Several studies have assessed the cosmetic scores of surgical scars using different subjective scar assessment tools such as the Hollander Wound Evaluation Score (HWES), the visual analogue scale (VAS), and the numeric rating scale (NRS).10,11 Subjective scar assessment scales provide a rapid evaluation of multiple scar characteristics, they are usually free and easily accessible, and it also capture patient’s opinion of their scars.12,13
The visual analogue score is a subjective assessment done by the patient on a 10cm line drawn and divided into 10 equal parts with zero representing the worst scar and 10 the best scar possible. It is reported to be consistent and reliable in scar assessment.14 To improve the VAS scale as an outcome measure, it can be combined with descriptive tools such as HWES to improve the numerical results of VAS.15,16
The Hollander Wound Evaluation Score (HWES) is easy to use, fast to complete, and provides technical feedback to practitioners on the quality of wound repair2. It is easily reproducible because of the binary nature of its scoring system; scar width is predefined as >2 mm, and each parameter assessed is scored either 1 for absent or 0 for present. It is a scoring system with a minimum score of zero (worst) and a maximum score of six (best).17 These scores are designated based on the absence or presence of six criteria. These criteria are margin separation, soft tissue step-off at borders, contour irregularities, edge eversion, excessive distortion, and overall appearance.17
Pain may be assessed by either pain unidimensional or multidimensional measures. The unidimensional methods assess pain quantitatively in terms of intensity. The commonly used methods are the visual analogue scale (VAS) and the numerical rating scale (NRS).18
The VAS is a continuous 100-millimeter scale (0-100) based on verbal descriptions of the extremes of pain without graduations: no pain and worst imaginable pain.18 The NRS is an 11-point scale (0-10), marked off in a graduated horizontal line with severity increasing with numerical character.18 It is easier to administer, although there is a tendency to overestimate pain scores.
The technique of skin closure chosen often depends on the surgeon’s preference or institutional practices. There is a need to determine a skin closure method that will result in a cosmetically acceptable scar for the patient. Hence, this study aims to compare satisfaction with surgical scars between adhesive strips and skin staples using the Hollander wound evaluation score, visual analogue score, and numeric rating scale.
Methodology
This prospective interventional study was conducted at the National Orthopaedic Hospital Igbobi, Lagos from September 2018 to August 2019. All patients who underwent primary total knee replacement and consented to the study were recruited. Patients who had revision surgery, were immunocompromised or had allergies to adhesive strips were excluded from the study. Approval for this study was obtained from the hospital Ethics and Research Committee.
Fifty-six patients were recruited into this study from the outpatient clinic. A simple randomization technique was used for sample segregation, such that patients who picked odd number cards were placed in group A (adhesive strip skin closure), whereas those with an even number of cards were assigned to group B (staple skin closure). The primary outcome measure was scar cosmesis and pain score on removal of skin closure material.
Prophylactic antibiotics were administered to all patients before a tourniquet was applied to the thigh. All patients received standard skin preparation, and surgeries were performed through a midline skin incision followed by a medial parapatellar arthrotomy. Following completion of the procedure, capsule closure was achieved with polyglactin suture (Size 1), with the insertion of an active drain. Subcutaneous wound closure was achieved with continuous polyglactin sutures (size 0).
Wound closure was performed with the knee flexed to the 45-degree position. Patients in Group A received skin closure with adhesive strips applied perpendicular to the wound and at 0-2mm intervals.4 These adhesive strips were applied after thorough drying of the wound. Half of the 1st adhesive strip was applied across the mid portion of the wound and the opposite edge of the wound was firmly apposed to its counterpart using forceps before the remaining strip was applied. Subsequent adhesive strips were applied using the same technique.
Patients in Group B received skin closure with skin staples. The wound edges were everted with dissecting forceps as the staples were applied with the crossbar a few millimetres above the skin surface and with a minimum inter-staple distance of 6 mm.11
All patients received standard wound dressing and postoperative care.
In week 2, the assessment of discomfort from removing coaptive material for patients in groups A and B was performed using the numeric rating scale score with 0 indicating no pain and 10 indicating the worst level of imaginable pain. At week 6, the surgical scar was assessed using a combination of the visual analogue score and the Hollander wound evaluation scale. All the data obtained were entered into the questionnaires.
Data analysis
All documented data from the questionnaires were analysed through the Statistical Package for Social Sciences (SPSS) version 20.0 for Windows. The results are illustrated in tables and charts. The chi-square-test and t-test were used to determine any statistically significant differences between the two methods of skin closure in primary total knee arthroplasty. P values of these variables less than 0.05 were considered significant.
Results
Fifty-six patients who met the inclusion criteria were recruited into the study; however, four patients were lost to follow-up.
Sociodemographic data
There were 41 females (78.8%) and 11 males (18.8%) in the study, with a female-to-male ratio of 3.7:1. The participants’ ages ranged from 54-86 years, with a mean of 67.9 + 8.0 years.
The visual analogue scale (VAS) score and Hollander wound evaluation score (HWES) were greater for the adhesive strip group than for the skin staple group. This result was statistically significant, with a P value of 0.000.
There was a statistically significant difference in the NRS score with the staple group recording a greater score at removal than the adhesive strip group. The VAS score and HWES were greater for the adhesive group.
Table 1: Sociodemographic Characteristics of Study Participants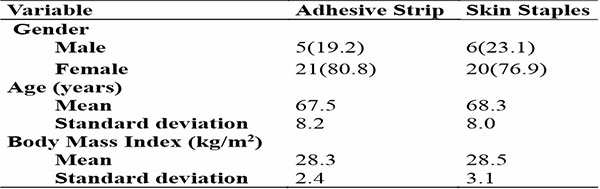
Table 2: The NRS, VAS, and HWES Scores of both treatment group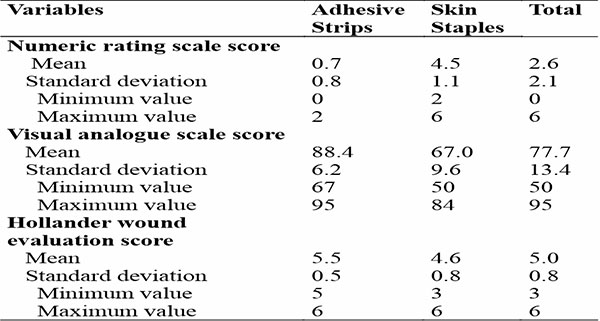
Table 3: Comparison of both treatment groups NRS scores, VAS scores, and HWES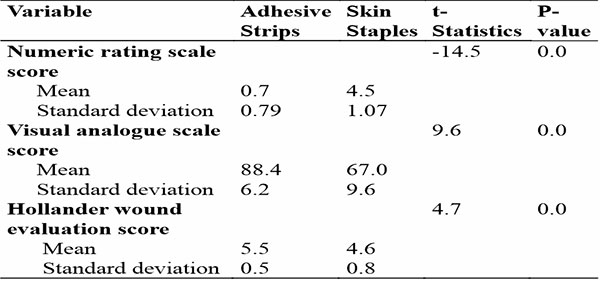
Discussion
Subjective scar assessment was used for this study because it is easy to apply, fast to complete, and provides technical feedback on the quality of the wound repair.2,7,8,12,13 Assessment of the wound was done at week 6 using HWES and VAS scores. Studies have shown there is no significant difference between HWES and the VAS score at 6 weeks or 3 months and 1 year.19,20
The mean VAS scores at week 6 for adhesive strips and staples were 88.4 and 67.0 respectively. The mean HWES for the adhesive strips group was also higher than the mean score for the staple group (5.5 and 4.6 respectively). These differences were statistically significant and may be explained by the absence of the puncture site scar with adhesive strip use, a feature frequently observed after skin-stapled closures.21
Takayama et al. reported similar findings in their study, however, this was based mainly on the absence of cross-hatching in the scar.4 Anuar et al reported better cosmesis with adhesive strips compared to sutures in their study of wound closure after long bone fracture fixation, this was due to adhesive strips not having suture marks and cross-hatching as opposed to sutures.22
Skin closure material removal constitutes a source of significant post-operative discomfort which may affect overall patient satisfaction. This was assessed using the numeric rating scale, it correlates well with the visual analogue scale score.23 Patients in the adhesive group reported less discomfort at coaptive device removal than those in the skin staple group. The NRS score was higher for the staple group on day 14 post-surgery when staples were removed compared to the removal of adhesive strips. This is due to the everting and lifting of the staples from the dermis and epidermis by the staple remover. The mean NRS score in the adhesive strips group was 0.7 whereas that in the staple group was 4. This difference was statistically significant. This higher level of satisfaction with adhesive strips was noted by Takayama et al. they attributed the increased patient satisfaction to the absence of pain or discomfort during adhesive strip removal and earlier showering time for patients.4
Conclusion
Optimal skin closure methods that yield an aesthetically pleasing scar are highly desirable, as they significantly enhance patient satisfaction and overall well-being. Furthermore, acceptable scars can reduce the emotional and psychological distress associated with visible reminders of surgery, leading to a better overall quality of life. Using adhesive strips for wound closure after knee arthroplasty provides a more cosmetically acceptable surgical scar and is associated with less discomfort or pain on removal than staples. A major limitation was the inability to blind surgeon/ patient to the method of skin closure which created some bias in assessment of outcome variables. This could not have been avoided since patient would see the wound during wound inspection and the skin closure method chosen would have to be executed by the researcher assistants and assessment of outcomes assessed by the same. Another limitation of this study was the relatively small sample size making it subject to type 2 errors. A larger multicentre study is recommended.
References
- Krebs VE, Elmallah RK, Khlopas A, et al. Wound closure techniques for total knee arthroplasty: An evidence-based review of the literature. J Arthroplasty.2017; 33(2):633638.
- Abelleyra Lastoria DA, Benny CK, Hing CB. Subjective scar assessment scales in orthopaedic surgery and determinants of patient satisfaction: A systematic review of the literature. Chin J Traumatol. 2023;26(5):276-283. doi: 10.1016/j.cjtee.2023.02.001
- Gaine WJ, Ramamohan NA, Hussein NA, et al. Wound infection in hip and knee arthroplasty..J Bone Surg Br 2000; 82-B: 561-5.
- Takayama S, Yamamoto T, Tsuchiya C, et al. Comparing Steri-Strip and Surgical staple wound closures after primary total knee arthroplasties. EurJ OrthopSurgTraumatol.2017;27(1):113-118.
- Carli AV, Spiro S, Barlow BT, et al. Using a non-invasive secure skin closure following total knee arthroplasty leads to fewer wound complications and no patient home care visits compared to surgical staples. Knee.2017; 24(5):1221-1226.
- Katchy AU, Katchy SC, Ekwedigwe HC, et al. Total knee replacement in Nigeria: An assessment of early functional outcome of 68 consecutive knees. Niger J Clin Pract 2018; 21:1202-8.
- Fearmonti R, Bond J, Erdmann D, Levinson H. A review of scar scales and scar measuring devices. Eplasty. 2010 Jun 21;10:e43. PMID: 20596233; PMCID: PMC2890387.
- Park JW, Koh YG, Shin SH, Choi Y, Kim W, Yoo HH, Lee JO, Jang YN, Kim J, Li K, Kim BJ, Yoo KH. Review of Scar Assessment Scales. Medical Lasers 2022;11:1-7. https://doi.org/10.25289/ML.2022.11.1.1.
- Price, K., Moiemen, N., Nice, L., & Mathers, J. (2021). Patient experience of scar assessment and the use of scar assessment tools during burns rehabilitation: a qualitative study. Burns & Trauma, 9. doi:10.1093/burnst/tkab005 .
- Eggers MD, Fang L, Lionberger DR. A comparison of wound closure techniques in total knee arthroplasty. J Arthroplasty. 2011;26(8): 1251-8e1 -4.
- Yuenyongviwat V. A randomised controlled trial comparing skin closure in total knee arthroplasty in the same knee: nylon sutures versus skin staples.Bone Joint Res 2016;5: 185-190.
- Carrière, M.E., van de Kar, A.L., van Zuijlen, P.P.M. (2020). Scar Assessment Scales. In: Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G. (eds) Textbook on Scar Management. Springer, Cham. https://doi.org/10.1007/978-3-030-44766-3_14
- Lee, K.C., Dretzke, J., Grover, L. et al. A systematic review of objective burn scar measurements. Burn Trauma 4, 14 (2016). https://doi.org/10.1186/s41038-016-0036-x
- Duncan, J. A. L., Bond, J. S., Mason, T., Ludlow, A., Cridland, P., O???Kane, S., & Ferguson, M. W. J. (2006). Visual Analogue Scale Scoring and Ranking: A Suitable and Sensitive Method for Assessing Scar Quality? Plastic and Reconstructive Surgery, 118(4), 909–918. doi:10.1097/01.prs.0000232378.887.
- Kim KY, Anoushiravani AA, Long WJ, et al. A meta-analysis and systematic review evaluating skin closure after total knee arthroplasty – What is the best method? J Arthroplasty.2017; 32(9): 2920-2927.
- Quinn JV, Wells GA. An assessment of clinical wound evaluation scales. Acad Emerg Med. 1998;5(6):583-586. doi:10.1111/j.1553-2712.1998.tb02465.x
- Hollander JE, Singer AJ, Valentine S, et al. Wound registry: development and validation. Ann Emerg Med 1995.25(5): 675- 678.
- Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain. Arthritis care and research. 2011; 63(11):240-252.
- Nepal, S., Ruangsomboon, P., Udomkiat, P., & Unnanuntana, A. (2020). Cosmetic outcomes and patient satisfaction compared between staples and subcuticular suture technique for wound closure after primary total knee arthroplasty: a randomized controlled trial. Archives of Orthopaedic and Trauma Surgery. doi:10.1007/s00402-020-03479-3.
- Quinn J, Wells G, Sutclife T, Jarmuske M, Maw J, Stiell I (1998) Tissue adhesive versus suture wound repair at 1 year: randomized clinical trial correlating early, 3-month, and 1-year cosmetic outcome. Ann Emerg Med 32:645–649. https://doi.org/10.1016/ s0196-0644(98)70061-7.
- Clayer, M., & Southwood, R. T. (1991). COMPARATIVE STUDY OF SKIN CLOSURE IN HIP SURGERY. ANZ Journal of Surgery, 61(5), 363–365. doi:10.1111/j.1445-2197.1991.tb00235.x
- Anuar Ramdhan I, Zulmi W, Hidayah A, Kamel M, Fadhil M, Anwar Hau M (2013) Comparative study between coaptive film versus suture for wound closure after long bone fracture fixation. Malays Orthop J 7(1):52–55.
- Gusman, D. N. (2012). Suture materials and techniques. Lower Extremity Soft Tissue & Cutaneous Plastic Surgery, 77–100. doi:10.1016/b978-0-7020-3136-6.00009-6.