A histomorphological assessment of endoscopic biopsies in patients with upper gastrointestinal diseases in a tertiary hospital setting in Nigeria
Nwafor Chukwuemeka Charles,1 Owobu Clifford Ikhuoria,2 Keshinro Samuel Olalekan,3 Udofia Uduak Kufre,4 Essien Udobong McEinstein,5 Okafor Innocent Chibuike5
Abstract
This is a prospective, observational and descriptive study of all the upper gastrointestinal endoscopies (UGIE) that were performed between January 2020 and December 2022.
All UGIE and biopsies were performed by one endoscopist. Clinical information on age, sex, presenting complains, endoscopic findings and provisional diagnosis were retrieved from laboratory forms.
Results: A total of 273 biopsies were obtained from 181 patients, 6 (2.2%) from the upper and lower esophagus sphincter, 180 (65.9%) from different parts of the gastrum and 87 (31.9%) from the first and second parts of the duodenum.
The most common indication for upper endoscopy was dyspepsia. Of all the esophageal biopsies, 83.3% of them had no pathology. Only 3 (1.6%) cases of the gastric biopsies were histologically confirmed to be gastric adenocarcinoma. The vast majority of the gastric lesions were inflammatory. Chronic gastritis was seen in 92.7% of cases. Only one (1.1%) case of malignant duodenal lesion was seen (1.1%). Of the 273 UGIE biopsies, only 4 (1.5%) malignant lesions were seen.
Conclusion: A baseline data of the pattern of UGIE in Akwa Ibom State has been documented. Chronic gastritis is very common, while esophageal lesions and gastric malignancies are rare.
Key words: Gastric biopsies; Chronic gastritis; Gastric cancer; Dyspepsia; Uyo
Introduction
The upper gastrointestinal tract (UGIT) is the part of the gastrointestinal tract that includes the mouth, esophagus, stomach and the duodenum. Major pathologies that affect the UGIT include congenital and acquired diseases. Acquired diseases of the UGIT include inflammatory diseases, benign neoplastic and malignant neoplastic diseases. The common diseases of the UGIT are esophagitis, gastroesophageal reflux disease (GERD), gastritis, duodenitis, esophageal and gastric carcinomas.1
Upper gastrointestinal endoscopy (UGIE), is an effective and appropriate preliminary investigation that is useful in the management of patients with various UGIT diseases. UGIE in combination with tissue biopsy for histology is the gold standard for management of patients with UGIT pathologies. This combination is of great importance.2-6 UGIE is not only the most accurate tool for evaluating patients with gastrointestinal related symptoms, it is also the most cost effective. In addition, certain therapeutic interventions such as sclerotherapy, banding, stricture stretching, gastrostomy and polypectomy can be done.7
Globally the commonest non neoplastic and neoplastic esophageal lesions are esophagitis and esophageal adenocarcinoma respectively.8 Esophageal cancer is ranked as the 7th most common cancer globally and recent studies have shown that esophageal squamous cell carcinoma is no longer the most common malignant lesion, rather esophageal adenocarcinoma.8 Gastritis is the commonest non neoplastic gastric lesion, while gastric adenocarcinoma is the commonest gastric malignancy.1 Gastric carcinoma is the 5th most common malignancy and the 3rd most deadly cancer.9 Duodenal malignancies are very rare, while chronic duodenitis are the predominant lesion at this site.1
Though UGIE could be said to be a common medical procedure these days, however, studies have shown that in many African cities, it is not readily available and when available, it is unaffordable to many citizens, except for the urban middle class and above.10,11 A few UGIE studies from various parts of Nigeria and other African countries have been published. Unfortunately these UGIE studies from African countries are mostly of very short durations.3,12-18
The performance of UGIE with biopsy collection is dependent on the availability of qualified and experienced endoscopists in an area. Until three years ago, there was no endoscopist in Akwa Ibom State, Nigeria. UGIE is a relatively nascent procedure in our environment and there is no previous documentation of findings, hence the need for this study which aims to establish a baseline data, which will serve as basis for comparison in future.
Methodology
This is a prospective, observational and descriptive 3 years study of all the UGIE that were performed between January 2020 and December 2022.
Each patient was clinically evaluated and investigated before the procedure. All tests were carried out in the endoscopy suite using “a fibre optic gastroduodenoscopy Olympus, UK” and following standard techniques of instrument sterilization, patient premedication, positioning and follow up after the procedure. All UGIE and biopsies were performed by one endoscopist. Areas of the UGIT examined were the esophagus, stomach and upper parts of the duodenum. Mucosal biopsies were taken where necessary.
The biopsies were received in properly labeled and tightly closed specimen containers containing 10% neutral buffered formalin, which were then examined grossly for the number and appearance. Biopsy samples were fixed in 10% neutral buffered formalin, processed with an automated tissue processor, embedded in paraffin wax and 4-5 µm sections were obtained. The sections were stained with Haematoxylin & Eosin (H&E) and May Grünwald Giemsa for histopathologic examination. The histopathologic detection of Helicobacter pylori (H pylori) in gastric biopsy specimens was considered the gold standard for the diagnosis of H pylori infection. Immunohistochemistry (IHC) studies were done on few cases when indicated. The indications for IHC were for confirmation of diagnosis for suspected cases of gastric maltoma and undifferentiated carcinoma. In such cases, the most representative tissue block was sent to reference laboratories.
Clinical information on age, sex, presenting complains, endoscopic findings and provisional diagnosis were retrieved from laboratory request forms that were sent along with the biopsy samples. The extracted patient’s clinical information was entered into a special data form (pro-forma designed for the study) before being entered into a computer. Collected data was analyzed using SPSS version 25. Chi-square test (Pearson value) was used for categorical variables. Student’s t-test was used to compare means. A P-value of less than 0.05 was considered statistically significant.
Inclusion Criteria: All endoscopic mucosal biopsies of esophageal, gastric and duodenal (1st and 2nd parts) lesions were included.
Exclusion Criteria
Patients presenting with lesions in the oral cavity and beyond the second part of the duodenum were excluded. Also excluded were cases in which only fibrocollagenous tissues were seen on histology.
Results
Table 1, shows the age group, gender and site distribution of cases. A total of 273 biopsies were taken from 181 patients, (6 from the upper and lower esophageal sphincters, 180 from different parts of the gastrum and 87 from the first and second parts of the duodenum). The ages ranged from 14 years to 85 years, with a mean age of 50.78 ± 16.65. In all cases that had esophageal biopsies except one, biopsies were also taken from the gastrum. The 6 esophageal biopsy cases were between age groups 20-59 years, with a male to female sex ratio of 1:1. Gastric biopsies were taken from 180 cases (94 males and 86 females), with a male to female sex ratio of 1.1:1. All age groups were involved (as shown in table 1). There was an increase in cases with increasing age group, up to age group 60-69 years and a descent in number of cases was observed thereafter. All the 87 cases of duodenal biopsies also had gastric biopsies from at least 3 parts of the gastrum. All age groups were involved, although most duodenal biopsies were taken from age group 40-49 years, with a male to female sex ratio of 1.3: 1. The age range was between 14 years and 85 years, with a mean age of 50.78 years and a standard deviation of 16.65.
Table 1: Age, gender and site wise-distribution of upper endoscopic biopsies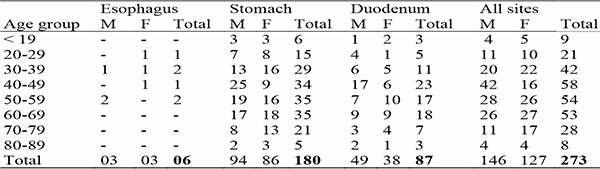
Table 2: Indications for upper endoscopy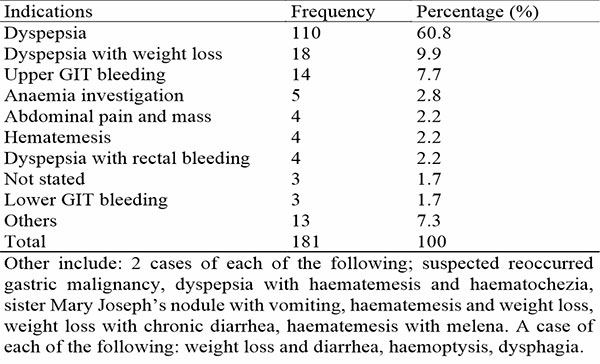
The most common indication for upper endoscopy was dyspepsia alone in 60.8% of cases as shown in table 2. This was distantly followed by dyspepsia with weight loss in 9.9% of cases. The third most common indication for upper endoscopy was upper GIT bleeding and this was seen in 7.7% of cases. Dyspepsia was also seen in combination with other complaints like weight loss, rectal bleeding, haematemesis and haematochezia. In all dyspepsia was seen in 74% of cases. Table 3, shows the various clinical diagnoses made at presentation and gross appearance on endoscopy. Localized gastritis was made in 34.8% of cases, whereas pangastritis was the clinical diagnosis in 26.5% of cases. In 16.6% of cases, the clinical diagnoses were not stated. Suspected peptic ulcer diseases accounted for 11.6% of cases, whereas GERD and suspected cancer cases accounted for 3.9% and 2.2% respectively. Erythema was the commonest gross appearance as it was seen in 49.7% of cases. The gastric mucosa was edematous in 23.8% of cases, while erosion, nodular appearance and ulceration were observed in 19.3%, 7.7% and 6.1% of cases respectively.
Table 3: Clinical diagnosis at presentation and gross appearance on endoscopy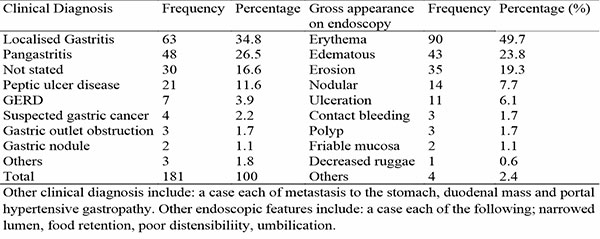
In this study, biopsies were predominantly obtained from 5 sites (fundus, corpus, incisura, antrum and D1) in each patient in 53.6% of cases, as shown in table 4. In 17.1% of cases biopsies were obtained from 3 sites corpus, incisura and antrum. The 3rd most common group were cases in which biopsies were obtained from 4 sites (fundus, corpus, incisura and antrum accounting for 11%. Biopsies taken from only 2 sites (corpus and D1), were seen in 2.2% of cases, whereas biopsy taken from only one gastric site (corpus) was seen in only 1.7% of cases.
Table 4: Specific sites of biopsy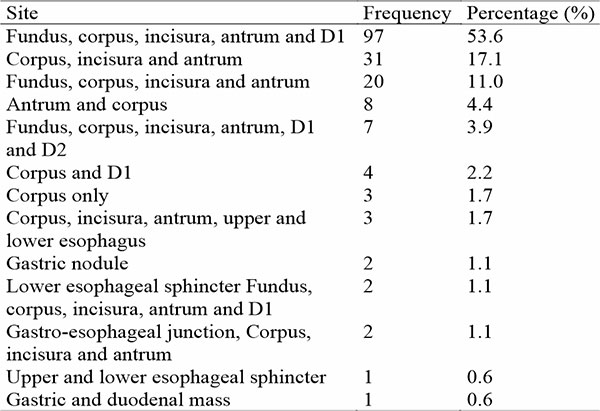
Of the 6 upper and lower esophageal sphincters biopsies, no pathology was seen in 83.3% of them, as shown in table 5. In only 1 (16.7%) was a diagnosis of esophageal hyperkeratosis made.
Table 5: Distribution of histopathologic diagnosis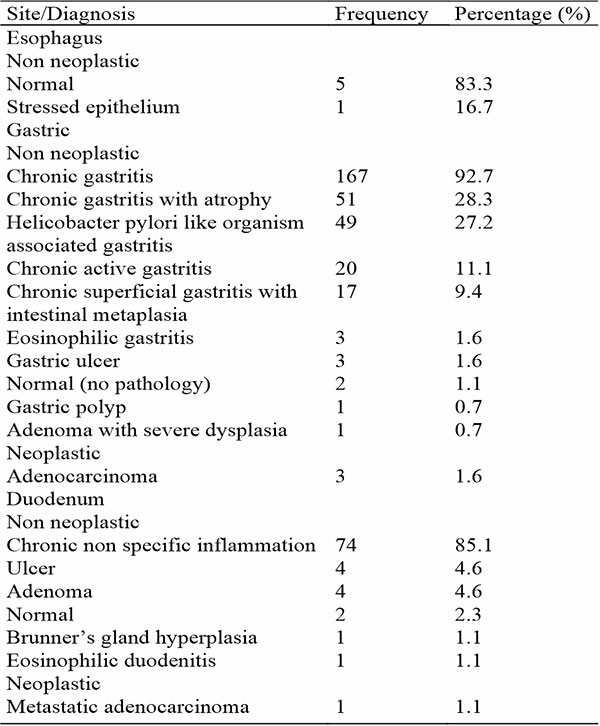
Only 3 (1.6%) cases of gastric biopsies were confirmed histologically to be gastric adenocarcinoma. Two of the gastric adenocarcinomas were seen in biopsies of males patients, aged 72 and 73 years, with the lesions predominantly involving the corpus. The third (33.3 %) gastric adenocarcinoma case was seen in the biopsy of a 64 - year - old female who presented with an antral nodule. The vast majority of lesions were non neoplastic, comprising various types of gastric inflammatory disorders. Chronic gastritis were seen in 92.7% of cases, while gastritis with atrophy accounted for 28.3% of cases, followed by Helicobacter pylori like organism associated gastritis (27.2%), chronic active gastritis (11.1%) and chronic superficial gastritis with intestinal metaplasia (9.4%). Gastric ulcer accounted for 1.6%, while normal gastric mucosa (no pathology seen), was observed in 2 (1.1%) cases.
Only one (1.1%) case of malignant duodenal lesion was seen (1.1%) and it was from a metastatic lesion from an elderly male with prostatic adenocarcinoma. Two (2.3%) cases of normal duodenum were seen, while in 85.1% of cases, the chronic non specific inflammation was the histologic diagnoses. Duodenal ulcer and adenoma each accounted for 4.6% of cases. A significant association was observed between the clinical diagnoses and the histopathologic diagnoses, with a P value of 0.000. Of the 273 UGIE biopsies, only 4 (1.5%) malignant lesions were seen.
Table 6: Comparison of index study with other studies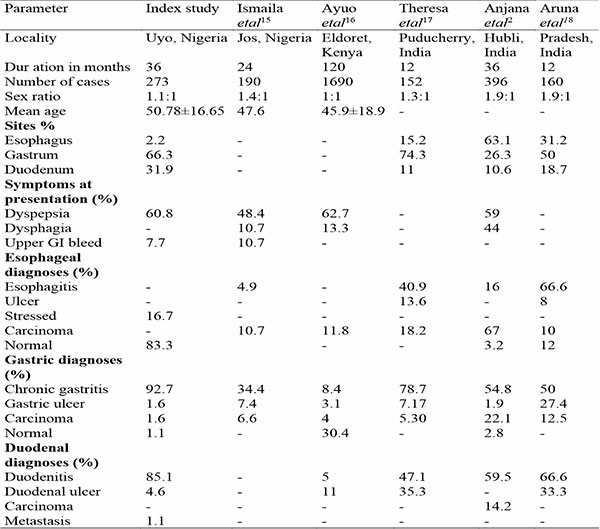
Table 6, shows a comparison of the index study with other studies that handled UGIE as a whole.
The various diagnoses made on the gastric biopsies seen in the index study are compared with findings from various Nigerian studies that concentrated on gastric endoscopic biopsies alone, as shown in table 7.
Table 7: Comparison index study with various gastric endoscopic biopsy studies done in Nigeria and other countries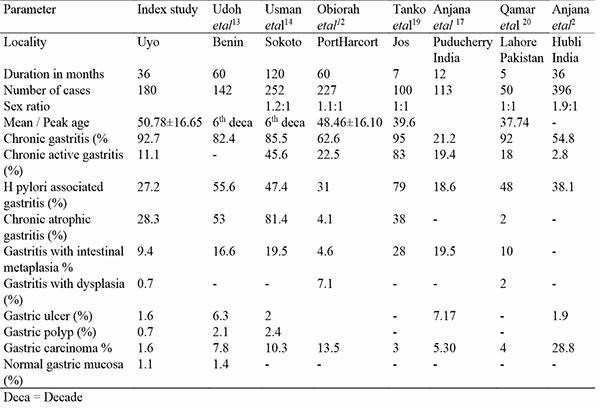
Discussion
Following an UGIE and biopsy, an excellent opportunity is provided for the clinician and histopathologist to correlate the clinical data, endoscopic and histopathological findings for an improved patient management. Endoscopic biopsy and histopathologic findings also aid in identifying the changing patterns in the spectrum of a disease, thereby identifying when medical interventions can be introduced to reduce disease progression and associated morbidity and mortality.
Based on site distribution of cases, only 2.2 % of UGIE biopsies were obtained from the oesophagus, which is less than 15.0 %, 31 % and 63.1 % reported in Puducherry, Pradesh and Hubli, respectively, all in India.2,17,18 Unfortunately there is scant information on UGIE studies done in Nigeria with focus on esophageal lesions. The few cases seen in this study were mainly reported as normal esophagus. This is in contrast to the studies done in Jos (Central Nigeria), Kenya and different parts of India, where various pathologies (including esophagitis, ulcer and carcinomas) were observed.2,15-18 The low number of esophageal biopsies in this study may be the reason, though it may also be a reflection of the number of patients presenting with complaints that warrant biopsies of the esophagus. The lower number of esophageal biopsies in the index study also corroborates with previous study in the same locality (though not on UGIE but on gastrointestinal lesions generally), where 2 (1.1%) cases of inflammatory lesions and 3 (7.3%) cases of malignant lesions were documented.21 The high rate of 67% documented by Anjana etal in Hubli India, was due to high rate of tobacco chewing in their study environment.2
An inverse relationship was observed between the number of gastric biopsies and esophageal biopsies. The higher the number of esophageal biopsies, the lower the gastric biopsies and this was observed in all the studies mentioned earlier.2,17,18 Though the reason for this observation was not stated, this may be related to the clinical condition of the patients and the part of the gastrointestinal tract with the major pathology. A lesion in the esophagus may be large enough to partly or completely occlude the esophagus and hence reduce access to the gastrum.
Duodenal biopsies constituted 31.9% of all the biopsies in this study. This is higher than the observed rate in previous studies (10.6%, 11% and 18.7%).2,17,18 The higher rate of biopsies from this site in the index study was not necessarily due to increase in the number of pathologies at this site, but rather due to attempts by the endoscopist to take biopsies widely enough not to miss pathologies in the adjacent areas. Majority of the histopathologic diagnoses were non specific duodenitis, distantly followed by duodenal ulcer. This is similar to observations in Kenya and different parts of India, though the cases of duodenal ulcerations in India were higher than the rate observed in the index study.2,16-18 Primary malignant lesion of the duodenum is rare and was not mentioned in any study reviewed except by Anjana etal in Hubli India.1,2
In study and some previous studies, non neoplastic diagnoses far out-number the neoplastic diagnoses for UGIE. This is in contrast to findings in Hubli India, where 67% of the esophageal biopsies were diagnosed to be malignant lesions.2,15-18
There is a slight male preponderance in the index and some previous studies. The mean age of cases in this study (50.74 years), is greater than that documented in Jos and Kenya.2,15-18 The male preponderance is believed to be due to the higher prevalence of habits like smoking, alcoholism and stressful lifestyle in males which are known risk factors for UGI diseases.5
Dyspepsia is a chronic or frequently recurring group of symptoms which include epigastric pain or discomfort (which could be intermittent or persistent), may or may not be associated with belching, bloating, heart burn, nausea, or vomiting, which is usually of gastroduodenal region.22 Similar to other studies, dyspepsia was the most common indication for UGIE.2-6,15-18 Other common indications were dysphagia and massive upper gastrointestinal bleeding, progressive weight loss, persistent vomiting, iron deficiency anemia, epigastric mass and suspicious barium meal results.
Following a gastric biopsy, the common diagnoses could be various types of gastritis, gastric ulcer, gastric cancer and normal gastric tissue. The standard protocol for reporting gastritis following UGIE is the use of the Sydney system of reporting, which focuses on topography, severity of H. Pylori density, inflammation, activity, atrophy and intestinal metaplasia.23 During UGIE, two tissue samples each should ideally be obtained from at least the corpus, antrum and incisura.23 This aims at reducing sampling errors.23 The endoscopist in our setting adhered to this, by obtaining adequate samples (specimens) from at least corpus, incisura and antrum in more than 70% of cases. This is in contrast to previous reviewed studies that were silent on topography.2-6,10-19
In studies done both within and outside Nigeria, chronic gastritis was the commonest diagnoses following a gastric biopsy.2-6,10-19 This is similar to observations in the index study though the rate of 94.3% documented in this study is higher than what were seen in previous studies. In this study, chronic gastritis (with or without specific features) was defined as the presence of a uniform infiltration of the superficial and or deep lamina propria by lymphocytes and plasma cells.1,24 Chronic active gastritis was defined as the additional presence of neutrophils. This was observed in 11.1% of the index study and is less than 19.4%, 22.5%, 45.6% and 83% observed in various Nigerian studies.12-14,19 It is also less than 18% in Lahore Pakistan and 19.4% in Puducherry India.17,20 In contrast, significantly less chronic active gastritis rates of 2.8 % and 5.0 % were reported in both Hubli and Mumbai, India, respectively.2,6
H pylori organism is a well known etiologic agent in gastritis and its complications of peptic ulcer disease (PUD) and gastric carcinoma and mucosa associated lymphoid tissue lymphoma (MALToma). Its eradication is necessary for the cure of gastritis, PUD and prevention of malignant lesion development.1,24 H. pylori - associated chronic gastritis was seen in 27.2 % of gastric biopsies in this study. This is less than the rates ranging from 31.0 to 79.0 % earlier reported in studies done in Nigerian and also less than 38.1 % and 48.0 % in studies documented elsewhere in Hubli, India and Lahore, Pakistan, respectively.12-14,19,20 The observation of H.Pylori in this study in contrast is higher than the 18.6 % reported in Puducherry, India.17 Several factors are known to determine the incidence of H pylori in patients on evaluation for chronic gastritis. These factors include: proper orientation of foveolae in tissue biopsy (as the organism are seen in gastric foveolae), making thin sections during tissue processing, with proper staining technique and the use of special stains such as Giemsa for the detection of these micro-organisms. H pylori prevalence and incidence is also known to vary depending on socio-economic conditions, poverty, overcrowding, poor sanitation and poor hygiene.25,26 The ease with which citizens in our environment can procure and self-medicate themselves with different types of antibiotics, before presenting may also be a reason to the low rate observed in our study.
Gastric mucosal atrophy is the loss of specialized gastric glands (parietal cells) in the mucosa, partly replaced by intestinal metaplastic epithelium. It is characterized by architectural changes manifested by variation in the volume and irregularity in the shape, branching, and spacing of the glands.2,24 Mucosal atrophy rate of 28.3% was observed in this study is greater than 2%, 3% and 4.1% documented in Lahore Pakistan, Mumbi India and Port Harcourt Nigeria, but less than 38%, 53% and 81.4% documented in Jos, Benin and Sokoto respectively.6,12-14,19,20 The general variation in the rates observed for chronic gastritis may be due to variation in personal, nutritional and environmental factors of the individuals.
Malignant gastric neoplasms include, adenocarcinomas, MALTomas, gastrointestinal stromal tumors, carcinoid tumors etc. of which gastric adenocarcinomas are the most common.1 Only 1.6% of UGIE biopsies in this study were malignant gastric lesions and all 3 were adenocarcinomas. This is far less than the reported rates from other previous Nigerian studies.12-15,19 Similarly the index rate of 1.6% is also less than all the rates reported in studies done outside Nigeria, except in Tamilnadu India, where a lower rate of 1% was documented.2-6,10,11,16-18,27 No reason was given by the authors for the significant low rate. We have no immediate explanation for the significant low rate of malignant gastric cases seen in these series. Future studies are required to confirm or invalidate this finding.
The five most common gross morphologic findings in our study following UGIE in order of appearance, were erythema, edema, erosion, nodularity and small ulcerations. These corroborate with previous findings by Qamar etal though these findings do not generally point to any definitive histopathologic diagnosis, grade of gastritis or presence of H pylori, however erosions, erythema and friability are related to inflammation and activity.20,28 This may also be the reason why many of the reviewed studies did not make mention of them.
Normal endoscopy was found in very low percentage of our patients (1.1%), compared to what was reported in other studies. The study by Udoh et al is the only Nigerian study that reported normal endoscopy, with a comparable rate of 1.4%.13 In contrast, higher rates ranging from 2.4 % to 48.0 % were reported in various international studies2,3,4,10,15,16,27. These patients might be suffering from functional dyspepsia, which is quite common, rather than obvious structural UGI abnormalities.10,18 The index lower rate of normal findings may likely be due to better/meticulous selection of patients for UGIE by the gastroenterologist. Due to high cost of UGIE and the fact that some studies have demonstrated that endoscopy does not change the outcome in patients with dyspepsia, some schools of thought have argued that endoscopy should be reserved for the high risk patients or those with alarming symptoms.29
The major limitation of this study, is that this analysis may suffer from a selection bias as only those who could afford the cost of UGIE (which is expensive in our environment) were scoped and hence included in this analysis. Thus our results may not stand the test of generalization, as only those who could pay underwent the procedure. The diagnostic accuracy of endoscopy is known to be dependent on the experience of the endoscopist, this may have also added some bias as all the UGIE procedure were performed by one endoscopist. A history of exposure to major risk factors for gastric cancers such as alcohol, spices and consumption of opiates were not obtained from our patients. Hence the effect of these factors in our local environment cannot be extracted from this study.
In conclusion, a baseline data of the pattern of UGIE in Akwa Ibom state has been documented in this study. Chronic gastritis and duodenitis are very common, while esophageal lesions and gastric malignancies are rare. Most of the patients were aged between 30-69 years.
References
- Kumar V, Abbas A K, Aster J C. The gastrointestinal tract. In: Kumar V, Abbas A K, Aster J C editors. Robbins and Cotran Pathologic Basis of Diseases. 10th ed. India: Elsevier; 2021. P. 753-822.
- Anjana M L, Kavitha Y. Histopathological Spectrum of Upper Gastrointestinal Endoscopic Biopsies in a Tertiary care centre. Annals of Pathology and Laboratory Medicine 2021; 8 (6): A-159 – A-163.
- Elhadi A A, Mirghani H O, Merghani T H, Mohammed O S, Eltoum H A. Pattern of Endoscopic Findings of Upper Gastrointestinal Tract in Omdurman Teaching Hospital, Sudan. Sudan JMS 2014; 9 (2): 71 – 74.
- Sulieman M A, Ahmed K M, Abdelhamid A A, Yahya A A. The Changing Pattern of Upper Gastro-Intestinal Lesions in Southern Saudi Arabia: An Endoscopic Study. The Saudi Journal of Gastroenterology 2010; 16 (1):35-7.
- Abhimanyu S, Kapil G. Clinicopathological correlation of upper gastrointestinal tract endoscopic biopsies in a tertiary care hospital in rural area of North India. Int. J. Adv. Res. 2020; 8 (03): 1155-1160.
- Neha S S, Purwa P. Histopathological Study of the upper gastrointestinal tract endoscopic biopsies. Annals of Pathology and Laboratory Medicine 2018; 5 (8): A-683 – A-688.
- Jones M P. Evaluation and treatment of dyspepsia. Postgrad Med J 2003; 79: 25 – 29.
- Huang J, Koulaouzidis A, Marlicz W, Lok V, Chu C, Ngai C H et al. Global burden, risk factors and trends of esophageal cancer: An analysis of cancer registries from 48 countries. Cancers 2021; 13 (141): 1-16.
- Bray F, Ferlay J, Soerjomataram I. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018; 68: 394-424.
- Kayamba V, Sinkala E, Mwanamakondo S, Soko R, Kawimbe B, Amadi B. Trends in upper gastrointestinal diagnosis over four decades in Lusaka, Zambia: a retrospective analysis of endoscopic findings BMC Gastroenterology 2015; 15:127: 2-9.
- Michael M, Hillary M T, Violet K, Gift M, Elly O, Mengistu E. Gastrointestinal endoscopy capacity in Eastern Africa. Endosc Int Open 2021; 09: E1827–E1836
- Obiorah C C, Nwafor C C. Clinicopathologic profile of gastric endoscopic biopsies in PortHarcourt Nigeria. Global Journal of Medical Research: Microbiology and Pathology 2020; 20 (1): 1-7.
- Udoh M O, Obaseki D E. Histopathological Evaluation Of H. Pylori Associated Gastric Lesions In Benin City, Nigeria. East African Medical Journal2012; 89 (12): 408-413.
- Usman B, Abubakar S M. Morphologic pattern of diseases in gastric biopsies and role of Helicobacter Pylori in chronic gastritis at a Nigerian Teaching Hospital. Saudi J Pathol Microbiol 2021, 6 (2): 71-75.
- Ismaila B O, Misauno M A. Gastrointestinal endoscopy in Nigeria - a prospective two year audit. Pan African Medical Journal 2013; 14:22. doi:10.11604/pamj.2013.14.22.1865.
- Ayuo P O, Some F F, Kiplagat J. Upper gastrointestinal endoscopy findings in patients referred with upper gastrointestinal symptoms in Eldoret, Kenya: A retrospective review. East African Medical Journal 2014; 91 (8): 267-273.
- Theresa M J, Lavanya M, Gerald R J, Sultan B K. Evaluating the spectrum of histomorphological patterns on endoscopic biopsy in patients with upper gastrointestinal tract disorders. Trop J Pathol Microbiol 2019; 6(1):1-8.
- Aruna E, Chakravarthy V K, Prospective Study on histopathological spectrum of upper gastrointestinal tract lesions in a Teaching Hospital of Southern India. Journal of Clinical and Diagnostic Research. 2020 Nov, Vol-14(11): EC37-EC41.
- Tanko M N, Echejoh G O, Mandong B M, Manasseh A N, Malu A O. Gastric histopathological findings in mucosal biopsies of symptomatic patients in Jos central Nigeria. Nig J Med 2007; 16(2): 113-118.
- Qamar S, Bukhari M, Asrar A, Sarwar S, Niazi S. Evaluation of antral gastric biopsies. A study of 50 patients at Mayo Hospital. Special edition annals 2010; 16 (1): 45-50.
- Nwafor C C, Nwafor N N, Etuk E B, Kanu O. Histopathological spectrum of gastrointestinal lesions seen in university of uyo teaching hospital, South–South Nigeria. Ann Trop Pathol 2019;10:27-33.
- Veldhuyzen van Zanten SJ, Flook N, Chiba N, Armstrong D, Barkun A, Bradette M, et al. An evidence-based approach to the management of patients with dyspepsia in the era of Helicobacter pylori. Can Med Assoc J 2000;162:S3-23.
- Dixon M F, Genta R M, Yardley J H, Correa P. Classification and grading of gastritis: the updated Sydney system. The American journal of surgical pathology 1996; 20(10), 1161-1181.
- Goldblum J R, Lamps L W, Mckenney J K. The Gastrointestinal tract. In: Goldblum J R, Lamps L W, Mckenney J K editors. Rosai and Ackerman’s surgical pathology. 11th ed. China: Elsevier Health Sciences 2017. 585 – 816.
- Farinha P, Gascoyne R D. Helicobacter pylori and MALT lymphoma. Gastroenterol 2005; 128: 1579-1605.
- Gonnzaga L, Coelho V, Barua R L, Emm Q. Latin American consensus conference on helicobacter pylori infection. Amer J Gastroenterl 2000; 95: 2688-2691.
- Padma S, Murugan R. Disease pattern by upper gastrointestinal endoscopy in rural areas of Tiruchirappalli district carried out at CMCH and RC Irungalur, retrospective study and comparative analysis with other contemporary studies in India. Int Surg J 2018;5:965-70.
- Ohkusa T, Kumagai J, Tanizawa T. Changes in endo-scopic features and histological findings of H.pylori related gastritis with a follow-up over a year after eradication of H.pylori. 1999 Jan; 57 (1): 173-8.
- Schmidt N, Peitz U, Lippert H, Malfertheiner P. Missing gastric cancer in dyspepsia. Aliment Pharmacol Ther 2005; 21: 813-820.