Infant and young child feeding practices associated with nutritional status among children attending child welfare clinic in Kericho County, Kenya
Daniel Kipngeno Cheruiyot*1,2, David Kamau2, Willy Kiboi Kahanya3
Abstract
Background: Breastfeeding is widely recognized as the gold standard for infant feeding in the first six months of life, providing essential nutrients and antibodies for optimal growth and development. However, suboptimal breastfeeding practices and inadequate complementary feeding can contribute to malnutrition. This study assessed complementary feeding practices associated with nutritional status in breastfed children.
Materials and methods: The study population were children aged 6 to 59 months in Kericho County. The study was designed as an institutional based cross-sectional survey of children seen in Kericho County Referral Hospital and Kakaptet Sub- County Hospital. Simple random sampling was used to select 172 study participants across these hospitals. Descriptive statistics, chi square and Fischer’s exact tests were carried out. Additionally, both unadjusted and adjusted odds ratio were obtained using multinomial regression analysis. Ethical standards were strictly adhered to throughout the study.
Results: Findings revealed that 75 (43.6%) children were aged between 24 and 59 months, 55 (32%) were aged 9 to 23 months and 42 (24.4%) were aged 6 to 8 months. Approximately two-thirds of caregivers had attained secondary education (n=77, 44.8%). Stunting was prevalent in 25% of the children, while both wasting and underweight affected 23.8%. Approximately 39% of caregivers introduced their children to complementary feeds before six months of age. Only 39.2% of children aged 6 to 23 months consumed five or more food groups for minimum dietary diversity (MDD). In the study, 95.9% of the children met the recommended minimum meal frequency (MMF), but only 39.2% had the minimum acceptable diet (MAD).
Conclusion: Introduction of complementary food after 6 months reduced the likelihood of wasting and stunting. Implementing targeted nutrition interventions for children aged 6 to 59 months in Kericho County is imperative.
Key words: nutritional status, stunting, wasting, underweight
Introduction
Malnutrition remains a significant public health problem in many developing countries, including Kenya. Despite significant advancements in child health, stunting, underweight, and wasting continue to affect a substantial proportion of children, particularly in rural areas. Indeed, the global statistics on child malnutrition are truly alarming. An estimated 149 million children under five-year-olds had chronic malnutrition as reported by World Health Organization (WHO) and United Nations Children Development Fund.1 Additionally, the prevalence of wasting and stunting in Africa was 6.8% and 34.8% respectively.1,2 Similar trends were observed in Kenya with a prevalence of stunting, wasting and underweight of 18%, 5% and 10% respectively2. With up to 45% of child deaths globally being linked to malnutrition, these statistics shows an undesired state of child malnutrition which demand immediate action.1
Breastfeeding is widely recognized as the gold standard for infant feeding in the first six months of life, providing essential nutrients and antibodies for optimal growth and development. Recent data reported that 823,000 deaths of the under-five-year-old children were preventable by optimal breastfeeding.3 Additionally, WHO observed that mortalities, especially in developing countries, could be reduced by 20% in the first two years of life with appropriate breastfeeding and complementary feeding practice.4 However, suboptimal breastfeeding practices and inadequate complementary feeding can contribute to malnutrition.5
Previous studies have reported various factors associated with child malnutrition, including maternal education, socioeconomic status, breastfeeding and complementary feeding practices. In Kenya, studies have investigated the prevalence of malnutrition and its determinants in different regions.6 However, there is lack of studies examining the specific complementary feeding practices associated with nutritional status in breastfed children in Kericho County. Additionally, given that Kericho County is predominantly a rural area with people of diverse socioeconomic status, there is need to understand the complementary feeding practices that are associated with nutritional status in this county. By examining complementary feeding practices associated with nutritional status in breastfed children the study aimed to contribute to a better understanding of the challenges faced by children in this cohort in Kericho County.
Methodology
Study design and area
The study was carried out in Kericho County, Kenya. It was carried out as an institutional based cross-sectional study to investigate the association between nutritional status with breastfeeding and complementary feeding practices of children aged 6 to 59 months. Two institutions used as the study site were Kapkatet Sub-County Hospital which is located at latitude and longitude coordinates of -0.629716 and 35.197243 respectively and Kericho County Referral Hospital located at latitude and longitude coordinates of 0.3713° S, 35.2801° E respectively. The two institutions are major referral hospitals within Kericho County, especially for children with severely acute malnutrition and those with moderate acute malnutrition that occurs with complications.
Study population and sampling procedure
The study population consisted of children aged 6 to 59 months attending the child welfare clinic. Children who were critically ill and required intensive medical care were excluded from the study to minimize the risk of additional stress and potential harm. A sample size of 172 children was determined, using Fischer formula and adjusted to account for attrition.7,8 The simple random sampling method was used to select the study participants from the child welfare clinic book. All caregiver-child pair listed in the child welfare clinic book whose next date of visitation was within the study period had an equal chance of being included in the study. To ensure equal chance, at the onset each caregiver-child pair was assigned a unique identification number. A random number was thereafter generated and it was used to select numbers within the range of assigned identifications. The caregiver-child pairs that corresponded to the randomly generated numbers formed the study sample. The distribution of the study participants across the two hospitals was done using probability proportionate to size.
Data collection
Data were collected from the months of April to July, 2023 through a number of methods and tools. Previously validated standardized questionnaires adopted from the infant and young child feeding practices guideline – 2021 were used to collect data during the face-to-face interviews with the caregivers7. Anthropometric measurements were carried out using standard procedures described by Centre for Disease control as described by earlier studies8,9.
Measures
The independent variable was nutritional status which was assessed using z scores generated from anthropometric measurements. They included weight for-age z-score (WAZ), weight for-height z-score (WHZ) and height for-age z-score (HAZ). The dependent variables were the socio-demographic characteristics of the child and the mother. Socio-demographics assessed which were specific to the child included age of the child, sex of the child, place of child birth and mode of delivery. Age of the caregiver, marital status, religion, household head, caregiver use alcohol and household size were the socio-demographic factors assessed that were specific to the caregiver. Breastfeeding practices were assessed based on initiation, and duration. On the other hand, complementary feeding was assessed based on the timing of introduction, frequency measured as minimum meal frequency, and type of foods measured as minimum meal diversity and minimum acceptable diet.
Data analysis
The characteristics of the study population were summarized by descriptive statistics using both ENA for SMART and statistical package for social sciences (SPSS). Chi square tests and Fischer’s exact tests were used to compare categorical variables between groups with different nutritional statuses. Variables that were significantly associated at bivariate analysis were further subjected to multinomial logistic regression analysis. Adjusted regression analysis was also carried out by controlling for socio-demographic characteristics.
Ethical consideration
Ethical clearance was obtained from the Ethical Scientific Review Committee of Mount Kenya University. Both verbal and written informed consent was sought from all the participants (caregivers) before inclusion of their children in the study. Additionally, the investigators ensured data confidentiality and privacy throughout the study. This was done by ensuring that unique codes were used to identify the participants and storage of the consent forms in a lockable cabinet which was accessible only to the investigators.
Result
Child specific socio-demographics
As shown in table 1, 75 (43.6%) of the children were aged 24-59 years, followed by 55 (32%) who were aged 9 to 23 months and 42 (24.4%) who had age range of 6 to 8 months. Additionally, 88 (51.2%) of the children were males and 84 (48.8%) were females. Majority of the children (n=163, 94.8%) were delivered at the health facility. The mode of delivery for about three quarters of the children (n=131, 76.2%) was vagnally.
Table 1: Child specific socio-demographic characteristics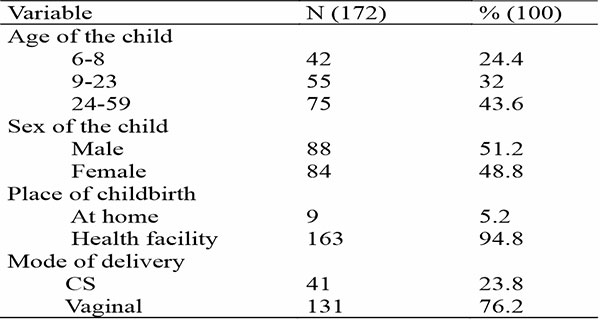
Caregiver-specific socio-demographic characteristics
As shown in table 2 the age range of the respondents was 14 to 47 years with 163 (92.4%) of them aged 20 to 47 years. Majority of the caregivers practiced Christianity (n=169, 98.3%) and were either married or cohabiting (63.4%). Households were majorly headed by males (102, 59.3%), and about equal proportion of the households had 1 to 3 members (n=80, 46.5%) and 4 to 6 members (n=79, 45.9%). Additionally, 47 (27.3%) of the caregivers used alcohol.
Table 2: Caregiver-specific socio-demographic characteristics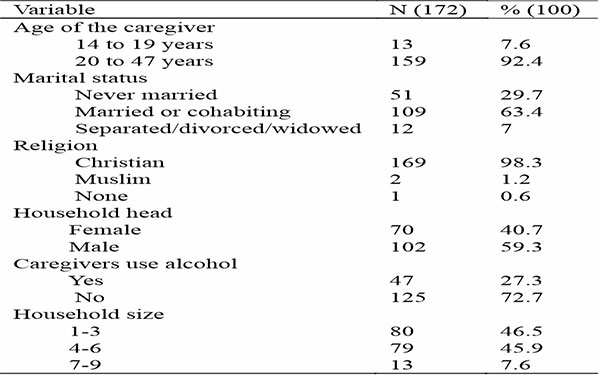
Nutritional status of children aged 6 to 59 months
The nutritional status of children aged 6 to 59 months in Kericho County are as shown in figure 1. The prevalence of stunting was higher than both underweight and wasting with a score of 25%. Equal proportion (23.8%) of the children studied were underweight and wasted.
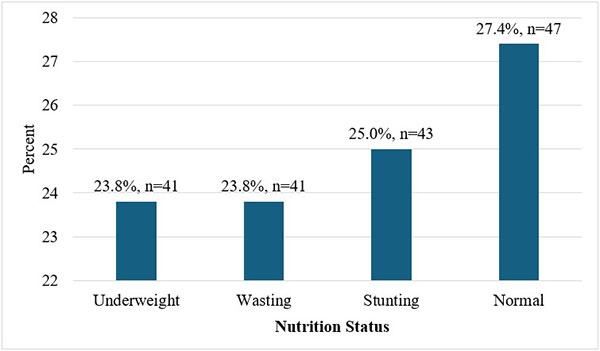
Figure 1: Nutritional status of children aged 6 to 59 months
Breastfeeding and complementary feeding practices
The results on breastfeeding and complementary feeding practices are reported in table 3. Majority of the children, with a proportion of 167 (97.1%) had been breastfed, and 139 (80.8%) were breastfed within 1 hour after birth. Additionally, 158 (91.9%) of the caregivers received breastfeeding support and education from healthcare provider, followed by 9 (5.2%) from the CHVs and 5 (2.9%) from an elderly mother. Additionally, 71 (41.3%) of the children were currently being breastfed. About 67 (39%) had their caregivers introduce complementary food before the age of 6 months. With regards to minimum dietary diversity, 38 (39.2%) of the children aged 6 to 23 months were fed on five or more food groups while the rest were not. A similar proportion of the children fed on the minimum acceptable diet (MAD), and 93 (95.9%) of the children aged 6 to 23 months were fed on the recommended minimum meal frequency.
Table 3: Breastfeeding and complementary feeding practices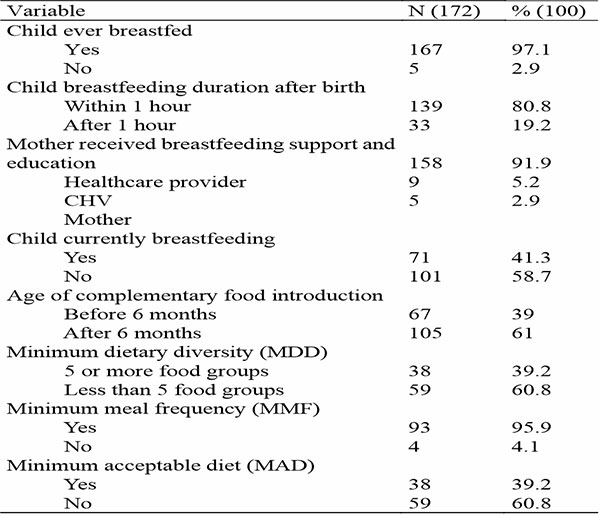
Food groups for complementary feeding
Figure 2. shows food groups and proportions the caregivers fed their children. The findings presented in this figure shows that 169 (98.3%) of the children were fed with grains - white/pale starchy roots, tubers and plantains. About 123 (71.5%) of the children were fed other fruits and vegetables while 110 (64%) of them were fed dairy products. Additionally, 88 (51.2%) of the children were fed legumes and pulses and a similar number given vitamin A rich fruits and vegetables. The children were also fed fleshy foods like meat, fish, poultry and organ meat with 61 (35.5%) of them given food from this food group. Eggs was the least consumed with 55 (32%) of children feeding from it.
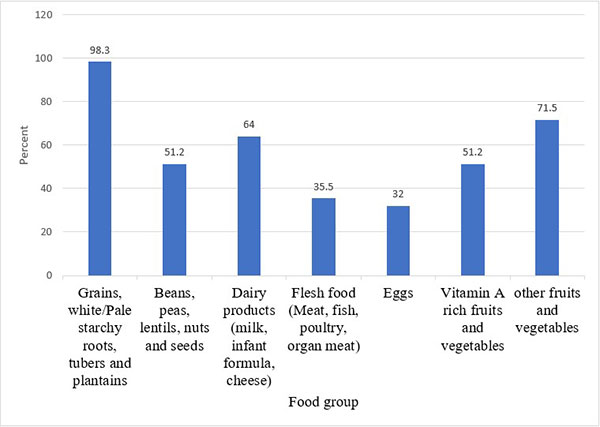
Figure 2. Types of food given to children aged 6 to 59 months
Association between infant and young child feeding practices and nutritional status
The results of unadjusted logistic regression analysis on the association between breastfeeding and complementary feeding with nutritional status are presented in table 4. The findings revealed that children who were introduced to complementary feeds after 6 months had significantly lower chances of being wasted (OR = 0.49, 95% CI: 0.29-0.83, p = 0.04) and stunted (OR = 0.71, 95% CI: 0.25-0.99, p = 0.02) compared to those who were introduced to complementary feeds before 6 months. The findings further showed that children introduced to complementary feeds before 6 months were associated with increased likelihood of underweight (OR = 1.33, 95% CI: 1.12-1.47, p = 0.01). Breastfeeding support from health workers was not likely to prevent underweight while initiation of breastfeeding within 1 hour after birth was associated with reduced chances for stunting (OR = 0.05, 95% CI: 0.03-0.07, p = 0.04).
Table 4: Logistic regression analysis of nutritional status and dietary practices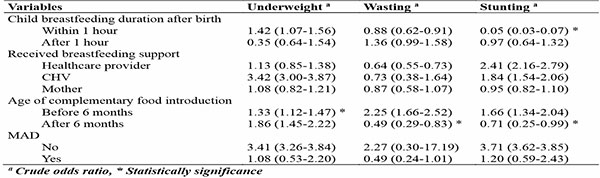
Association between infant and young child feeding practices and nutritional status
The results of unadjusted logistic regression analysis on the association between breastfeeding and complementary feeding with nutritional status are presented in table 4. The findings revealed that children who were introduced to complementary feeds after 6 months had significantly lower chances of being wasted (OR = 0.49, 95% CI: 0.29-0.83, p = 0.04) and stunted (OR = 0.71, 95% CI: 0.25-0.99, p = 0.02) compared to those who were introduced to complementary feeds before 6 months. The findings further showed that children introduced to complementary feeds before 6 months were associated with increased likelihood of underweight (OR = 1.33, 95% CI: 1.12-1.47, p = 0.01). Breastfeeding support from health workers was not likely to prevent underweight while initiation of breastfeeding within 1 hour after birth was associated with reduced chances for stunting (OR = 0.05, 95% CI: 0.03-0.07, p = 0.04).
In the adjusted model presented in table 5, the analysis revealed that only one practice, specifically the age at introduction of complementary feeds, showed a significant association with nutritional status. Introducing complementary foods after 6 months of birth was linked to decreased chances for both wasting and stunting. The adjusted odds ratio (aOR) for wasting was found to be aOR = 0.25 (95% CI: 0.05-0.91, p = 0.03), indicating a statistically significant reduction in the likelihood of wasting. Similarly, the aOR for stunting was aOR = 0.44 (95% CI: 0.16-1.08, p = 0.04), suggesting a statistically significant decrease in the chances of stunting.
Table 5: Multiple logistic regression analysis for dietary practices associated with nutritional status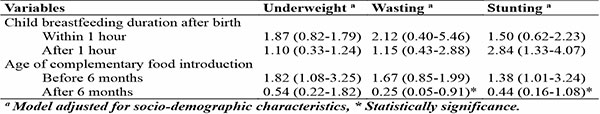
Discussion
The results showed that underweight, wasting, and stunting were rather common. Conflicting findings were reported in earlier research.9 A greater rate of stunting (27%), as well as underweight (26.3%). However, they reported lower frequency of wasting - 23%.10 Similarly, Ethiopian Demographic and Health Survey conducted in 2016 revealed that the underweight in the Tigran region was 23%).11 However, a study in Ghana reported lower prevalence scores for all the three forms of nutritional status compared to our study, that is stunting, underweight and wasting scores of 20.5%, 21.1% and 11.5%, respectively. Furthermore, according to 2022 Kenya Demographic Health Survey, the prevalence in the current study is significantly higher compared to the national prevalence of 19% and 18% in 2022, respectively.2 The observed differences between our findings and those from previous studies may reflect a range of underlying factors. For instance, the higher rates of stunting and underweight in our study could be indicative of localized nutritional deficiencies or inadequate access to healthcare services compared to regions with lower prevalence rates. Additionally, the discrepancies may also stem from differences in methodologies employed across studies, such as variations in sample size, demographic characteristics, and data collection techniques. Furthermore, socio-economic conditions, including food security and maternal education levels, play a crucial role in shaping nutritional outcomes; areas with better community-based nutrition programs and timely introduction of complementary foods tend to report improved nutritional status among children.12 The implications of this high stunting prevalence cannot be understated, as it heralds potentially lasting consequences for both the immediate and long-term health of these children such as delayed cognitive development and high risks of chronic diseases later on in their life.13 Stunting among the children remain one of significant challenges that impacts various parts of the nation and region, that call for implementation of effective approach to address the pressing issue.14
Almost all respondents (97.3%) had breastfed their children at some point. Previous studies reported mixed results. However, majority of the studies reported high breastfeeding frequencies.10-13 In order to ensure a child's development and overall health and nutritional condition, breastfeeding is essential.15 Over three quarters of the mothers surveyed said they had started breastfeeding their infants within the first hour after delivery. Earlier studies reported mixed findings, with most reporting fewer initiations of breastfeeding within an hour of childbirth.12,13 Distinct cultural customs and traditions may impact the timing of beginning breastfeeding. The disparities observed in our study compared to previous research could be an indication that several factors influence breastfeeding practices. While our findings show a high initiation rate of breastfeeding within the first hour, other studies, such as those conducted in Ghana and Ethiopia, report significantly lower rates, with only 39.4% and 58.3% initiating breastfeeding within this timeframe, respectively.10,11 These differences may be attributed to varying cultural beliefs surrounding colostrum and traditional feeding practices that discourage immediate breastfeeding, as seen in some communities where colostrum is perceived negatively. Additionally, factors such as maternal education and access to antenatal care have been shown to play a significant role in timely initiation; mothers with higher education levels or who received adequate prenatal counseling were more likely to initiate breastfeeding promptly.15 Furthermore, the impact of delivery conditions, such as cesarean sections or complications during birth, can also lead to delays in initiating breastfeeding, as evidenced by studies indicating longer times to initiation among those who underwent surgical deliveries.14-16
There was a considerable decrease in stunting and wasting in children whose complementary food introduction occurred after 6 months as opposed to those whose introduction occurred before 6 months. Findings from this research corroborated with those from Ghana that found a 0.75 lower risk of chronic malnutrition in children who started receiving complementary foods at six months of age.17 Another study carried out in India found that children were 1.24 times more likely to have stunting and 1.21 times more likely to suffer from severe stunting if complementary meals were introduced later in life.18 In addition, delayed complementary meal delivery increased the risk of wasting by 5.15 times. In our study, grains, white or pale starchy roots, tubers, and plantains made up the vast bulk of the complementary meals (97%). Carbohydrate foods such as grains and tuber foods were often given as complementary foods (75%) due to their availability, ease of access, and the ease of tolerance by the infant.19 The differences between our findings and those from previous studies shows that timing and composition of complementary feeding are influenced by a number of factors. For instance, while our study emphasizes the benefits of introducing complementary foods after six months other studies have reported that earlier introductions are often driven by cultural beliefs or misconceptions about infant readiness for solid foods.18 In particular, research from Sub Saharan Africa indicates that approximately 31.9% of infants are introduced to complementary foods before the recommended age of four months, which may lead to adverse health outcomes such as increased risks of gastrointestinal infections and slower growth velocity.17 Furthermore, differences in dietary practices across regions can affect the types of complementary foods introduced. For example, studies have shown that infants in some populations receive less diverse diets, lacking essential nutrients from protein sources like meat and dairy during the critical period of complementary feeding.18,19
We reported higher MMF but lower MAD and MDD. These crucial markers have been the subject of conflicting findings in different research.20 These results were in line with another research that found that over half of the infants (49.7%) had reached the MDD, almost 40% had reached the MAD, and over three quarters of the children (74.4%) had reached the recommended MMF.20 A study in Ethiopia found a somewhat greater MDD (59.9%) than what we reported, but a very low MAD percentage of approximately 10%. In contrast to the present study another study found lower proportions: only 17.8% of the youngsters had met MDD, 12% had satisfied MAD, and 40% had gotten meals twice daily.21 Disparities in food security due to variances in healthcare systems, cultural variety, and geographical location may have explained the variation. All three have significant impacts on people's eating patterns. Based on these findings, there is a need to intensify the promotion and support of early initiation of breastfeeding, followed by the introduction of safe complementary foods while continuing breastfeeding up to two years of age or beyond.22
Conclusion
Findings from the study revealed the importance of early commencement of breastfeeding within an hour of childbirth and the timely introduction of complementary feeds to ensure good nutritional results. In particular, the research found that children who were given complementary meals at the recommended intervals had a lower risk of wasting and stunting. The nutritional status of the participants was also affected by the frequency and diversity of the diet they consumed.
Conflict of interest
The author declares no conflict of interest.
References
- United Nations Children’s Fund (UNICEF), World Health Organization (WHO), International Bank for Reconstruction and Development/The World Bank Group. Levels and trends in child malnutrition: UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates. Key findings of the 2023 edition. 2023.
- Kenya National Bureau of Statistics and ICF. Kenya Demographic and Health Survey 2022. Key Indicators Report. Nairobi, Kenya, and Rockville, Maryland, USA: KNBS and ICF. [Internet]. 2023. Available from: www.DHSprogram.com.
- Ayub F, Anjum M, Bibi S, Khan A, Soomro S, Sardar A. Nutritional Status and its Association with Breastfeeding and Complementary Feeding Practices Among Children visiting Tertiary Care Health Centre. Pakistan Armed Forces Medical Journal. 2023 Aug 1;73(4):1028–32.
- Noh JW, Kim YM, Akram N, Yoo KB, Cheon J, Lee LJ, et al. Factors affecting breastfeeding practices in Sindh province, Pakistan: A secondary analysis of cross-sectional survey data. Int J Environ Res Public Health. 2019 May 2;16(10).
- Khaliq A, Wraith D, Miller Y, Nambiar S. Association of Infant Feeding Indicators and Infant Feeding Practices with Coexisting Forms of Malnutrition in Children under Six Months of Age. Nutrients. 2022 Oct 12;14(20):4242.
- Muluneh MW. Determinants of exclusive breastfeeding practices among mothers in Ethiopia. PLoS One. 2023 Feb 1;18(2 February).
- World Health Organization. (2021). Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF). Licence: CC BYNC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0
- Anino CO, Were GM, Khamasi J W. Positive Deviant Intervention Prevents Acute Malnutrition in Younger Siblings of Undernourished Children in Migori County, Kenya. Dedan Kimathi university repository. 2018;
- Anino, O. C., Were, G. M., & Khamasi, J. W. (2015). Impact evaluation of positive deviance hearth in Migori County, Kenya. African Journal of Food, Agriculture, Nutrition and Development, 15(5), 10578-10596.
- Dagnew GW, Asresie MB. Factors associated with chronic energy malnutrition among reproductive-age women in Ethiopia: An analysis of the 2016 Ethiopia demographic and health survey data. PLoS One. 2020 Dec 11;15(12):e0243148.
- Woldeamanuel BT, Tesfaye TT. Risk Factors Associated with Under-Five Stunting, Wasting, and Underweight Based on Ethiopian Demographic Health Survey Datasets in Tigray Region, Ethiopia. 2019.
- Akinyi MP, Achieng MFC. Influence of Complementary Feeding Practices on Nutritional Status of Children Between 6 to 24 Months in Kisumu County, Kenya. Journal of Research in Social Science and Humanities. 2023 Feb;2(2):1–6.
- Ali Z, Saaka M, Adams AG, Kamwininaang SK, Abizari AR. The effect of maternal and child factors on stunting, wasting and underweight among preschool children in Northern Ghana. BMC Nutr. 2024 Dec 4;3(1):31.
- Akanbonga S, Hasan T, Chowdhury U, Kaiser A, Akter Bonny F, Lim IE, et al. Infant and young child feeding practices and associated socioeconomic and demographic factors among children aged 6–23 months in Ghana: Findings from Ghana Multiple Indicator Cluster Survey, 2017–2018. PLoS One. 2023 Jun 9;18(6):e0286055.
- Jebena DD, Tenagashaw MW. Breastfeeding practice and factors associated with exclusive breastfeeding among mothers in Horro District, Ethiopia: A community-based cross-sectional study. PLoS One. 2022 Apr 1;17(4 April).
- Faraj K, Bouchefra S, El Ghouddany S, Elbaraka Y, Bour A. Early breastfeeding initiation: Exploring rates and determinants among postpartum women in Eastern Morocco. Sci Afr. 2023 Sep;21:e01883.
- Mekonen EG, Zegeye AF, Workneh BS. Complementary feeding practices and associated factors among mothers of children aged 6 to 23 months in Sub-saharan African countries: a multilevel analysis of the recent demographic and health survey. BMC Public Health. 2024 Jan 8;24(1):115.
- Toma TM, Andargie KT, Alula RA, Kebede BM, Gujo MM. Factors associated with wasting and stunting among children aged 06–59 months in South Ari District, Southern Ethiopia: a community-based cross-sectional study. BMC Nutr. 2023 Dec 1;9(1).
- Kenyatta J. Potential and safety of complementary foods developed from selected cereals and legumes cultivated in Gondar province, Ethiopia to alleviate protein-energy malnutrition Tsehayneh Geremew Yohannes doctor of philosophy (Food Science and Nutrition). 2022.
- Nurokhmah S, Middleton L, Hendarto A. Prevalence and Predictors of Complementary Feeding Practices Among Children Aged 6-23 Months in Indonesia. Journal of Preventive Medicine and Public Health. 2022 Nov 1;55(6):549–58.
- Ministry of Health. Turkana Smart Nutrition Survey June 2023 Report. Division of Family Wellness, Nutrition & Dietetics. June 2023.
- Mphasha MH, Makwela MS, Muleka N, Maanaso B, Phoku MM. Breastfeeding and Complementary Feeding Practices among Caregivers at Seshego Zone 4 Clinic in Limpopo Province, South Africa. Children. 2023 Jun 1;10(6).
- Anino CO., Mugalavai, V., & Kamau, E. H. (2013). A study on impact of climate change on the food and nutrition security in children of small-scale farmer households of Migori area. Glob. J. Biol. Agric. Heal. Sci, 2, 67-71