Evaluation of Simulation-based Training in Airway Management among Maiden Workshop Participants in Enugu, Nigeria: A Mixed-method Study
Anthony T. Eduviere,A Lily O. Otomewo,B,* Emuesiri G. Moke,A Joshua OnohwosafeA
Abstract
Context: Simulation-based training is a growing format in healthcare education in Nigeria. So far, most evaluation of the outcome have been limited to the usual pre- and post- tests of knowledge acquisition.
Objective: To evaluate our simulation-based airway training, identify the challenges and their potential solutions.
Materials and Methods: This study was conducted in the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu in April, 2024; seven months after the maiden simulation-based airway workshop. We applied the 4-level Kirkpatrick model of training evaluation to assess the outcome of the workshop. The attendees of the aforementioned simulation-based airway management workshop were invited as participants for the workshop evaluation. A mixed-method research design encompassing focus-group discussions and questionnaire-based survey was used for data collection.
Results: Twenty-nine respondents completed the questionnaire-based survey (six anaesthesia fellows, fifteen residents, eight anaesthetic technicians). Only seventeen respondents (58.6%) have had previous exposure to manikin-based training. The overall satisfaction rating with the SBT was 82.3±11.0 [0-100 scale]. The perceived learning from the SBT was adjudged to be greater in technical skills and knowledge than communication skills. Following the training, the trainees’ behaviour improved with the regular provision and use of gum-elastic bougies during endotracheal intubation. While most participants expressed the desire for more frequent training, some recommended the use of manikins with difficult airway as the means to enhance the SBT.
Conclusion: The training positively impacted on the trainees’ learning and behaviour. Most respondents requested more frequent training sessions as the means of enhancing the training.
Keywords: Airway, anaesthesia, education, simulation, skills.
Introduction
Airway management is a critical skill required for resuscitation and promotion of patient safety. Both basic and advanced airway management require training of medical and allied health professionals to acquire the relevant skills and competence in securing the patients airway. Simulation-based training (SBT) provides an artificial representation of a clinical scenario using simulation aids to achieve experiential learning. The adoption of SBT in healthcare enables the trainees to learn from mistakes without consequences for real patients and the trainees. Moreover, it offers unlimited opportunities for repetitive learning until mastery is achieved. Some technical skills such as fibreoptic bronchoscope for difficult airway management and cricothyrotomy for emergency airway access in “can't intubate and can't ventilate” scenario are considered very critical and lifesaving in advanced airway management. The superiority and desirability of SBT over didactic training for these two skills have been demonstrated in previous studies.1,2 On a wider scale, meta-analysis of airway management and anaesthesiology training studies gives credence to SBT over other training formats not only in technical skills learning but also in non-technical (soft) skills, behaviours and trainee satisfaction.3,4 These other non-technical skills and performance behaviors are known to be determinants and predictors of patient outcomes.5,6
Several types of simulators have been adapted for the wide variety of processes encountered in healthcare including; human cadavers, task trainers, simple manikin simulators, high-fidelity patient simulators, standardized/simulated patients, virtual reality, in-situ simulation techniques and hybrid simulation. For some procedures such as cricothyrotomy, human cadaver simulation could provide a superior learning experience compared to manikins.7 However, none of these modalities is universally superior to the others.8-10 Despite the greater degree of realism that high-fidelity simulators offer, they do not guarantee better trainees' outcomes. Indeed, for novice trainees, high-fidelity simulation offers little or no advantage over low-fidelity simulation, but may potentially impair learning.11
Learning experience is considered a crucial element in the acquisition of knowledge and skills among trainees. Studies of the relationships between learner satisfaction and performance outcome reveal significant positive correlation between satisfaction and engagement, and these in turn correlate positively with their overall performance.12,13
The recent incorporation of simulation in the educational curriculum of various anesthesiology boards is indicative of a new paradigm that features simulation as essential component of medical education, training, certification and recertification.14,15 However, the global evolution of SBT in anaesthesiology and critical care medicine is still work-in-progress, with limited application even in developed countries.16 Nonetheless, SBT programmes have been successfully adopted by anaesthesia providers in low-resource settings, with remarkable impact.17
By far, the commonest methodology described for most of the studies that evaluate simulation-based airway training has been the pre- and post-training outcome comparison.18 With these, it could be posited that the overwhelming evidence supporting SBT should inspire the conceptualization of new research questions. In effect, the relentless research effort at investigating ‘if it works’ could be considered trite and of less significance. Instead, interrogation of ‘how it works’ and ‘how can it be most effective’ may be the preferred research questions that would unlock optimal benefits from SBT.19,20 Hence, this study was designed to evaluate the workshop from the perspective of the trainees, identify the challenges and their potential solutions.
Materials and methods
Research ethics
The study was conducted in strict compliance with the Helsinki declaration on research in human subjects. The institutional research ethics committee of the University Of Nigeria Teaching Hospital (UNTH) granted approval for the study with protocol number; NHREC/05/01/2008B-FWA00002458-IRB00002323. The participants were provided written information about the study’s aims and procedures. Participation was voluntary and the participant’s right to decline participation and their right to withdraw at any time they may chose were guaranteed. Confidentiality was maintained regarding the participant’s identity. Written informed consent was obtained from each participant.
Study design
A cross-sectional study design using a mixed-method of data collection was adopted.
Training evaluation framework
One of the validated methods commonly used to assess training programmmes is the 4-level Kirkpatrick model.21 The purpose of the framework is to increase training effectiveness through a systematic evaluation process. The model evaluates the training outcomes of a programme at the four (4) levels. Level 1 evaluates trainees’ satisfaction toward the instructors and the training programmme. Level 2 assesses trainees’ learning of professional knowledge or skills. Level 3 measures the changes in trainees’ behavior or performance as adapted in real-life settings, while level 4 quantifies the improvement in the ultimate outcomes which are associated with the training programme.
Nationwide Collaboration in Airway Simulation in Nigeria
The collaboration between the Society of Specialists in Airway Management (SSAM) Nigeria and Airway Development Incorporated, USA has facilitated the establishment of dozens of airway simulation centres in Nigeria in the past one year. The respective centres have conducted decentralized airway workshops providing opportunity and capacity for both basic and advanced airway management training. One of the airway simulation centres is located in UNTH, Ituku-Ozalla, Enugu. Hitherto, there was no clinical simulation laboratory in UNTH, Enugu. The maiden airway management workshop at the Enugu simulation centre held for two days at the temporary space hosting the airway simulation centre in October, 2023. The workshop was preceded a day earlier by virtual lectures on the aims of the workshop and aspects of basic and advanced airway management. The hardware deployed for the workshop included manikins (adult airway task trainers), videolaryngoscopes (VDL), different models of laryngeal mask airway, gum-elastic bougies, intubating stylets, self-inflating bags, oropharyngeal airways, nasopharyngeal airways, fibreoptic laryngoscopes, lubricating gel, syringes and intubating pillows.
Inclusion criteria
All airway management personnel in the Department of Anaesthesia and Intensive Care of UNTH, Ituku- Ozalla, Enugu who attended the maiden simulation-based airway workshop that held in October, 2023 at the University of Nigeria Teaching Hospital, Ituku-Ozalla, Enugu.
Study setting and participants
This study was conducted in the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu in April, 2024; seven months after the simulation-based airway workshop. We invited all the attendees of the aforementioned simulation-based airway management workshop as the participants for this workshop evaluation. These included anaesthetic technicians, resident anaesthetists and anaesthesiology fellows. Other attendees to the workshop were perioperative nurses, intensive care nurses, ear-nose-throat surgeons, emergency physicians and medical students on anaesthesiology rotation. These medical and allied health professionals are members of the multidisciplinary team that require airway management training to acquire the relevant skills in securing the patients airway. Owing to logistic challenges attendees in the latter group, and others who were externally sourced were excluded from this study.
Procedure
The eligible participants were briefed on the purpose and methods of the study. Thereafter, the questionnaire-based survey which was in pen-and-paper format was self-administered to all the eligible participants in their respective clinical areas, delivered in sealed envelopes. In addition to question items that were used to evaluate the outcome measures the questionnaire also sought information from the participants regarding their gender, professional status and history of prior experience with manikin-based training. On completion, the filled questionnaires were retrieved same day in the sealed envelope. This was intended to conceal the respondent’s identity and their responses in order to enhance confidentiality. Next, were the focus-group discussions which were conducted in-person with the purposively-sampled discussants. There were two focus groups comprising of six members each. Group A was made up of anaesthetic technicians (6), while group B consisted of junior anaesthesiology residents (3), senior anaesthesiology resident (2) and anaesthesiology fellow (1). The principal researcher served as the facilitator and the discussions were recorded digitally. The focus group discussions were conducted separately and sequentially for the two groups, with each session lasting about an hour.
Outcome measures
The outcome measures evaluated in the survey were (a) Trainee satisfaction with the simulation-based airway training (b) Perceived learning by the participants (c) Trainee suggestions for improving the airway management training and learning experience.
The outcomes were measured by self-reported assessments by the participants. A structured format was used to assess the seven items in the trainee satisfaction evaluation. The items are; (1) Satisfaction with the number of training sessions (2) Satisfaction with the content and format of training sessions (3) Satisfaction with the equipment used for the training sessions (4) Satisfaction with instructor/trainer support during skills learning (5) Satisfaction with the environment or setting of the training programme (6) Satisfaction with the scheduling of the training programme (7) Overall satisfaction with the simulation-based training. Responses to items (1) - (6) were scored as; very dissatisfied (1), somewhat dissatisfied (2), neither satisfied nor dissatisfied (3), somewhat satisfied (4), and very satisfied (5). Consequently, higher scores indicated higher levels of satisfaction. Response to item (7) of satisfaction evaluation was scored on a scale of 0 - 100 to indicate the least and the greatest overall satisfaction with the simulation-based airway training, respectively. In a similar manner, a structured format was used to assess the three components of perceived learning (knowledge, technical skills, team communication skills) by the participants. A five-point likert-type score was used for the evaluations; Strongly agree (5), Somewhat agree (4), Undecided (3), Somewhat disagree (2), Strongly disagree (1). The questionnaire also incorporates a semi-structured, open-ended request for the participants to suggest one (1) way of enhancing airway management learning experience. The evaluation of the SBT was conducted along the Kirkpatrick’s model of training outcome assessment.
Data analysis
The collected data was checked for completeness and accuracy, prior to entry into the Statistical Product and Service Solutions, (IBM-SPSS Corp., Armonk, NY, USA) statistical package for windows version 25.0 for analysis. Categorical variables were presented using frequencies and proportions while continuous variables were summarized using mean and standard deviation. The mean overall satisfaction score with simulation-based training between any two groups of participants was compared using the Student t test. The level of statistical significance was determined by a p value of <0.05.
The recorded discussions of focus group discussions were transcribed verbatim following each session. For quality assurance purposes, the scripts were compared with the written notes for completeness and accuracy. Then each script was checked against the audiotape by an independent reviewer. As a way of verifying the quality of translations, tapes were doubly transcribed after which both scripts were checked for similarity and where differences existed, these were reconciled by the transcribers. Coding of transcripts was done based on themes as they emerged during the coding process. The themes from each interview were reviewed by the researcher and grouped under wider themes. QDA Miner Lite v2.0.6 was used in the analysis of qualitative data. Three themes emerged from the study. They included opinion about simulation-based training, impact of stimulation-based training on practice and suggestions on how to improve the trainings.
Results
All the returned questionnaires were correctly filled, with only one indicating no response to the open-ended questionnaire item seeking suggestion on ways of improving the simulation-based airway training. Twenty-nine respondents completed the questionnaire-based survey (six anaesthesiology fellows, fifteen resident anaesthetists, eight anaesthetic technicians). Nineteen (65.5%) of the respondents were males and 17 (58.6%) have had previous exposure to manikin-based training (Table1)
Table 1: Characteristics of the respondents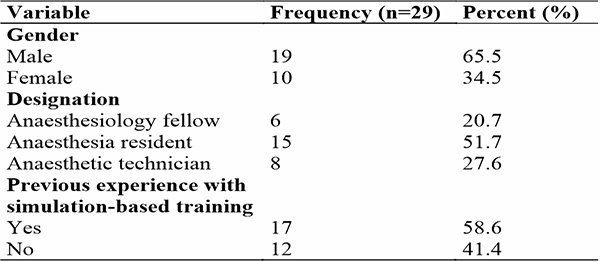
Table 2: Satisfaction with domains of the simulation-based training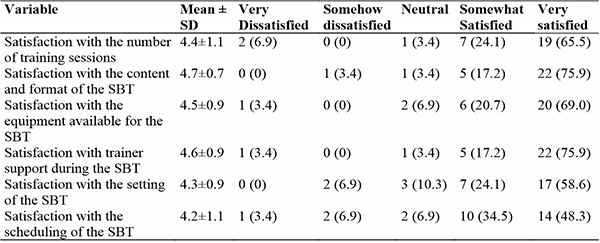
Table 2 indicates the satisfaction grading for the different domains of the simulation-based training. Among the six domains of the SBT the content and format domain was accorded the highest mean score of satisfaction, 4.7±0.7. This was closely followed by the satisfaction rating of the trainer support domain, 4.6±0.9. Conversely, the satisfaction with scheduling of the SBT recorded the least mean score of 4.2±1.1, followed by satisfaction with the setting of the SBT session, 4.3±0.9.
Table 3: Overall satisfaction with the simulation-based training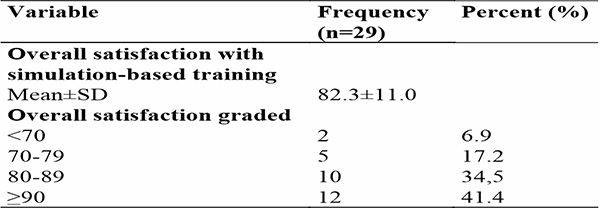
Table 3 shows overall satisfaction with the simulation-based training as rated by the trainees. The mean overall satisfaction score was 82.3±11.0. The highest proportion of the respondents, 41.4% had a satisfaction score =90 while the least, 6.9% had overall satisfaction at less than 70.
Table 4: Comparison of overall satisfaction score of different categories of participants with stimulation-based training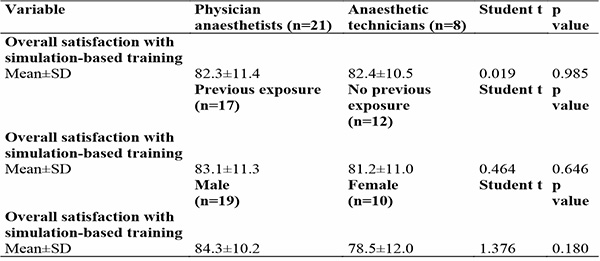
Table 4 shows comparison of overall satisfaction score with stimulation-based training among different categories of participants. The mean overall satisfaction score for those with previous exposure to manikin-based training, 83.1±11.3 was comparable to those with no previous exposure, 81.2±11.0, (Student t=0.464, p=0.646). There was no significant difference in the satisfaction scores on account of gender (Student t=1.376, p=0.180), or professional status (Student t=0.019, p= 0.985).
Table 5: Perceived learning during the SBT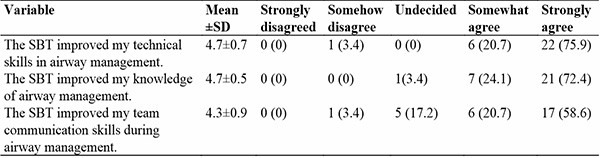
Table 5 shows the improvement in the various aspects of learning that the participants acquired during the training programme. The mean score for the improvement in team communication skills was least; 4.3±0.9, with remarkably greater improvement in knowledge and technical skills.
Table 6: Suggestions for improving the simulation-based airway training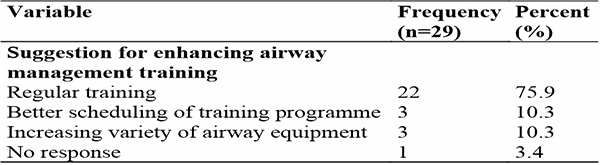
Table 6 shows suggestions on ways of enhancing airway management training. The highest proportion of the respondents, 75.9% suggested the need for regular training.
Result of Focus-group discussion (FGD)
Three themes emerged from the FGDs including the participants impression regarding the SBT, its impact on current practice of airway management and suggestions on how to improve future training sessions.
1. Impression regarding the stimulation-based training
The participants had varied impression regarding the training. However, they expressed a high level of satisfaction and were unanimous that the training improved their skills. One of the participants gave an impression of the training generally;
‘Training helps one to try his/her hands on some equipment that have not been in use on the real patients on the manikins and that gives one an idea of what to expect when one is working on a patient, and that also improves one’s skills’. (Participant 06).
The enthusiasm with the SBT was overwhelming. One discussant expressed her impression thus: “The workshop was very impactful. As registrars we didn’t really have the opportunity for hands-on learning on endotracheal intubation. With the manikins made available at the workshop and subsequently, we’ve been having continuous practice on improving our skills using both the VDL and Magill laryngoscope. The training session has actually improved my skills and that of my colleagues”. (Participant 01). For another discussant; “Particularly, it offered me the opportunity to master the use of the VDL. Prior to the workshop I had attempted to use the VDL once but it wasn’t successful and I was of the impression that it was easier to use the regular direct laryngoscopy with Magill laryngoscope than the VDL. During the SBT I tried my hands a couple of times but wasn’t successful but the trainers guided me through and since then I have been using the VDL successfully for difficult intubations and in pediatrics. Now, I’m no longer of the opinion that it is easier to use the normal Magill laryngoscope. My initial failed attempt at using the VDL was in a live patient. The success at the SBT using the manikin boosted my confidence a lot and since then I have been using the VDL on live patients. (Participant 07)
Another participant shared his own personal experience:
I had seen a lot of difficult intubations that I am now finding so easy. The devices have greatly aided airway management especially regarding difficult airways. This is especially so with the gum-elastic bougies. There is however limited access to some of the devices that were used during the workshop. But those bougies that were shared to us have been very useful. I still have my own’. (Participant 03).
2. Impact of the stimulation-based training on current practice
All the participants paid attention to the approach to practice since after the training in emphasizing its impact. These were how the participants exemplified their thoughts:
‘Most resident doctors prefer the rigid stylet to the regular malleable stylet that was hitherto in use in our centre. One thing I’ve observed is that immediately after the training when you give them the usual malleable stylet they’ll ask you to go and get the rigid stylet. Unfortunately, these stylets have gradually disappeared. Bougies are now routine practice devices in the operating rooms unlike before when their use was limited to the intensive care units (ICUs). We also use the bougies as tube exchanger’. (Participant 05).
‘One thing I can really mention is the use of bougie. It is becoming more frequent than what it used to be, and I always have it whenever I want to do an intubation. Then of course, whenever I’m anticipating difficult airway to gather other equipment like the VDL’. (Participant 02).
Despite the increasing preference for the rigid stylet following the SBT, some of the practitioners still opt for the malleable stylet. One of the participants had this to say:
‘They (referring to Resident doctors) don’t like using the rigid stylet. Most of them would say that we should get the usual ones that we were using, those ones that they can bend. And that’s what I always bring for them’. (Participant 11).
Another limitation to the impact of the SBT on current practice was revealed to be the unavalaibility of some of the advanced airway equipment that featured during the workshop. One discussant expressed her frustration: “We’ve not had a lot of practice with other advanced airway devices that we were exposed to during the workshop, I mean things like the intubating LMA which we don’t have in our centre. It was only at that workshop that I saw it and used it. So, for me, I don’t think I still have good skills with it, because i’ve not tried it again since after the workshop. It’s not just available”. (Participant 01).
3. Suggestions on improving stimulation-based training
Most participants expressed the desire for more frequent training, with one suggesting how this could be institutionalized: “More frequent training is required, especially if there could be a permanent airway simulation room, like a lab. with an instructor or something. We are gradually losing some of the knowledge and skills acquired during the training”. (Participant 09)
One of the participants was specific on the training session that is most essential to her and the reason for that. These were his words:
‘I will like more ultrasound sessions, because I think for one it reduces ‘poking’ of the patients’. (Participant 8).
Another participant was concerned that he was yet to have an intubation experience on a live patient and wished for that:
‘I don’t have any intubation experience on a live patient. Perhaps, we could be allowed to have the live intubation training’. (Participant 04).
One participant wished for the provision of manikins that have difficult airways in the training programme. This was based on his observation during the period of training.
‘Is it possible that in subsequent trainings we could get manikins that have difficult airways so that we can also use that to practice? The manikins provided once you open you will see everything’. (Participant 12).
The participants also expressed the need for more equipment. One participant made an explanation of what having more instruments could mean. He had this to say:
‘The only challenge might be like the VDL, which might not have all the blades for the patients you want to use it to work with. …..You know that for the paediatric patients you have newborn, then you have the infants ….. That is what I mean by not having all the blades. Generally, when you have the older patients, the blades are all available’. (Participant 08).
One of the participants expressed her reservation with the scheduling of the training programme thus:
“I can’t think of any other thing that can be added really to the programme except may be the scheduling. And of course, there’s no time that you’ll fix that will be suitable for everybody”. (Participant 10).
Discussion
Simulation-based education has only recently gained prominence in Nigeria and only 58.6% of the participants in our study have had a previous exposure to manikin-based education. A national survey of Nigerian paediatric healthcare professionals mirrored such low penetration with 23% of the physicians and 34% of the nurses admitting to having a simulation laboratory in their institution. The professionals further disclosed that manikin-based simulation was the norm, mostly for basic life support training.22
The overall satisfaction with the SBT was remarkably high with a mean of 82.3±11.0 %. The high satisfaction level recorded in the various individual domains corroborate with the overall satisfaction as declared in the single-item measure. In a study conducted in Ethiopia, Jamie and Mohammed reported a satisfaction level of 70.95% regarding SBT, among trainee undergraduate midwifery students.23 Similarly, in another study conducted in Saudi Arabia, Agha et al. reported an overall satisfaction score of 85% with SBT, among the trainee medical students.24 Whereas the level of satisfaction in our study compares well with the 70.95% and 85% reported in these two referenced studies, the methodological differences in their derivation should not be ignored. Our study derived the overall satisfaction of the sample by obtaining the mean of the individual responses to the single-item satisfaction scale of ‘0-100’. However, Agha et al. dichotomized the likert-type satisfaction responses to individual items, deriving the satisfaction level as the fraction of the total responses that is satisfied (satisfied and very satisfied), for each item in the questionnaire. Trainer support during skills demonstration has since been identified as a critical factor in trainee satisfaction during simulation-based learning.23,25 In the study by Jamie and Mohammed, the trainees who were assisted by their teachers during skills demonstration were about 6-fold more satisfied than those who were not assisted.23 Also the students who had more skills practicing sessions per semester were twice as likely to be satisfied with the SBT, than those who experienced fewer sessions.23 Among the trainees studied by Agha et al., most had observed the high fidelity simulators (69%), and 71% recommended for more training sessions with simulators.24 Both studies were cross-sectional surveys which utilized structured questionnaires to evaluate midwifery and medical students’ satisfaction with SBT, respectively. The trainees in both studies also had much greater exposure to simulation-based education (including high-fidelity simulators) than our participants. Our study compared the satisfaction scores with gender, trainee professional status and prior exposure to manikin-based training. We found no significant difference in satisfaction on account of these trainee characteristics. However, among medical school undergraduates studied by Agha et al. in Saudi Arabia their satisfaction with SBT showed a higher score for the females than males in third year.24
In our study, satisfaction with trainer support during the SBT was very high, second only to the satisfaction rating ascribed to the domain of content and format of the SBT. This finding suggests its influential contribution to the overall satisfaction scores recorded by our respondents. Expectedly too, the satisfaction with the number of training sessions received only modest rating. Our study design incorporated qualitative survey in the semi-structured questionnaire and the focus-group discussions in order to better explore the trainees perspective. In the suggestions proffered for enhancing the SBT majority of the questionnaire respondents, 75.9% (22/29) opted for more frequent and regular SBT sessions. This recommendation was corroborated by most discussants in the focus-group discussions while expressing a high level of satisfaction with the SBT. On further exploration of the themes of the focus-group discussions the participants confirmed that the training has improved airway management skills and attitudes, especially with the regular use of gum-elastic bougies during tracheal intubation. They also disclosed that despite the availability of the VDL its regular use is still hampered by administrative challenges. Other suggestions offered by the discussants towards enhancing the SBT were the provision of difficult airway manikins and establishment of permanent simulation laboratory staffed with instructor.
Regarding learning during the SBT session, our participants indicated that they acquired more technical skills and knowledge compared to communication skills. The improvement in communication skill attributed to SBT has generally not been as unequivocal as the technical skill acquisition.26 Rather unfortunately, much of surgical complications in the literature are traceable to deficiencies in non-technical skills, such as team communication rather than from technical errors of the surgery.27 The impact of communication skills in improving patient outcome has been mentioned earlier.5,6
In considering our training evaluation framework we reported outcomes related to three (level 1, level 2, level 3) of the four-level Kirkpatrick model for training evaluation. We evaluated the learner reaction (trainee satisfaction) using both the questionnaire survey and the focus-group discussions (Kirkpatrick level 1). The questionnaire survey evaluated the perceived acquisition of technical and non-technical skills, while the focus-group discussions gave deep insight regarding the technical skills acquired during the SBT (Kirkpatrick level 2). One of the themes explored in the focus-group discussions was the impact of the SBT on the current practice of the trainees. Following the SBT the regular provision and use of gum-elastic bougies during endotracheal intubation has become a routine (Participant 5). Along with this is the change in practice regarding the use of videolaryngoscopes, judging from the comment of a participant. (Participant 02). These represent improvement in the trainees’ behaviours and practice performance attributed to the SBT (Kirkpatrick level 3). We did not evaluate patient-centred outcomes (Kirkpatrick level 4) as these were not within the objectives of our study. Nielsen et al. undertook a systematic review on the impact of SBT in airway management.18 Out of the 22 studies analysed,19 conducted level 2 evaluation, four conducted level 4 evaluation, three conducted level 3 evaluation while none performed level 1 evaluation.18 None of the studies assessed all four Kirkpatrick levels, one study assessed three levels, two studies assessed two levels, while 19 studies assessed only one level (eighteen; level 2, one; level 4). The number of participants in each study considered in the systematic review ranged from 16 to 266, whereas 29 participants took part in our study. The Kirkpatrick model has been widely applied for the evaluation of other healthcare training programmes worldwide, including in low- and middle-income countries (LMICs).28,29 Surprisingly, despite the increasing popularity of simulation-based education in Nigeria, minimal effort has been devoted to evaluating their outcome. The shortcoming in comprehensive evaluation of training programmes with standard validated tools such as the Kirkpatrick model apparently besets other healthcare training programmes in the country.30,31,32
In actual fact, the evidence supporting the effectiveness of SBT is not lacking in the literature3,4. In evaluating the SBT we had also stated our aim to identify the challenges and proffer potential solutions. The preponderant recommendation for improving the simulation-based education was the implementation of frequent training workshops. There was resounding concordance in this proposition in both the questionnaire and focus-group discussion arms of the study. Thus, in a way this study provides the answer to ‘how SBT in airway management can be most effective’ rather than the endless interrogation and proof of its effectiveness.19,20 The participants also recommended the provision of manikins with difficult airway during future SBT, and the establishment of a permanent airway simulation laboratory for regular training.
Limitations
Perceived learning which is the trainee’s self-report of skill or knowledge acquisition is not equivalent to actual learning, the latter being a measurement of learning as determined by the trainer/educator. Whereas perceived learning is a frequently used indirect measure of learning in research its construct and validity are distinct from those of direct measure of learning which actual learning represents.33 Nevertheless, there is substantial corroboration between the perceived learning reported in the questionnaire arm and the focus-group discussions, providing justification for the mixed-methodology of the study design. Another limitation of this study is the relatively small sample size. This would not permit a more detailed analysis of the data to determine the participant’s factors that may affect satisfaction, learning or change in behavior.
Strengths
In addition to the knowledge and technical skill acquisition during the SBT our study also evaluated the trainees improvement in non-technical skills (team communication), being important determinants of clinical outcome.5
Conclusion
Overall, the participants reported high satisfaction with the simulation-based airway training. The respondents also perceived that it enhanced their technical skill, knowledge and team communication. The trainees’ behaviours and practice performance improved following the SBT. The respondents expressed desire for more frequent training sessions and the provision of manikins with difficult airway as means of enhancing the simulation-based training.
Conflict of interest: The authors declare that no conflict of interest exists.
Funding support: Nil.
References
- Shetty K, Nayyar V, Stachowski E, Byth K. Training for cricothyroidotomy. Anaesth Intensive Care. 2013;41(5):623-30.
- Nilsson PM, Russell L, Ringsted C, Hertz P, Konge L. Simulation-based training in flexible fibreoptic intubation: A randomised study. Eur J Anaesthesiol. 2015;32(9):609-14.
- Sun Y, Pan C, Li T, Gan TJ. Airway management education: simulation based training versus non-simulation based training-A systematic review and meta-analyses. BMC Anesthesiol. 2017 ;17(1):17.
- Su Y, Zeng Y. Simulation based training versus non-simulation based training in anesthesiology: A meta-analysis of randomized controlled trials. Heliyon. 2023;9(8):e18249.
- Stahel PF, Cobianchi L, Dal Mas F, Paterson-Brown S, Sakakushev BE, Nguyen C, et al. The role of teamwork and non-technical skills for improving emergency surgical outcomes: an international perspective. Patient Saf Surg. 2022;16(1):8.
- Merry AF, Weller JM. Communication and team function affect patient outcomes in anaesthesia: getting the message across. Br J Anaesth. 2021;127(3):349-52.
- Takayesu JK, Peak D, Stearns D. Cadaver-based training is superior to simulation training for cricothyrotomy and tube thoracostomy. Intern Emerg Med. 2017;12(1):99-102.
- Abulfaraj MM, Jeffers JM, Tackett S, Chang T. Virtual Reality vs. High-Fidelity Mannequin-Based Simulation: A Pilot Randomized Trial Evaluating Learner Performance. Cureus. 2021;13(8):e17091.
- Chernikova O, Heitzmann N, Stadler M, Holzberger D, Seidel T, Fischer F. Simulation-based learning in higher education: A meta-analysis. Rev Educ Res. 2020;90(4):499–541.
- Arnold JJ, Johnson LM, Tucker SJ, Chesak SS, Dierkhising RA. Comparison of Three Simulation-Based Teaching Methodologies for Emergency Response. Clin Simul Nurs. 2013;9 (3): e85-e93.
- Jones M. Effects of Simulation Fidelity on Learning Transfer. Journal of Educational Informatics. 2021;2(1):24–34.
- Li N, Marsh V, Rienties B. Modelling and managing learner satisfaction: Use of learner feedback to enhance blended and online learning experience. Decis. Sci. J. Innov. Educ.2016;14(2), 216–42.
- Rajabalee YB, Santally MI. Learner satisfaction, engagement and performances in an online module: Implications for institutional e-learning policy. Educ Inf Technol. 2021;26: 2623–56.
- Tayeb BO, Shubbak FA, Doais KS, Yamani AN, Dhaifallah DG, Alsayed EF, et al. Uses of simulation-based education for anesthesiology training, certification and recertification: A scoping review. J Taibah Univ Med Sci. 2023;18(5):1118-23.
- Shorten GD, De Robartis E, GoldikZ, kietaibi S, Niemi-Murola L. European section/Board of Anaesthesiology/European Society of Anaesthesiology consensus statement on competency-based education and training in anaesthesiology. Eur J Anaesthesiol. 2020;37(6):421-34.
- Savoldelli GL, Ostergaard D. Simulation-based education and training in anaesthesia during residency in Europe: where are we now? A survey conducted by the European Society of Anaesthesiology and Intensive Care Simulation Committee. Eur J Anaesthesiol. 2022;39(6):558-61.
- Mossenson AI, Tuyishime E, Rawson D, Mukwesi C, Whynot S. Promoting anaesthesia providers non-technical skills through the vital Anaesthesia Simulation Training (VAST) course in a low-resource setting.Br J Anaesth. 2020;124(2):206-13.
- Nielsen RP, Nikolajsen L, Paltved C, Aagaard R. Effect of simulation-based team training in airway management: a systematic review. Anaesthesia. 2021;76(10):1404-15.
- Eppich W, Reedy G. Advancing healthcare simulation research: innovations in theory, methodology, and method. Adv Simul (Lond). 2022;7(1):23.
- Henriksen K, Rodrick D, Grace EN, Brady PJ. Challenges in Health Care Simulation: Are We Learning Anything New? Acad Med. 2018;93(5):705-8.
- Paull M, Craig Whitsed C, Girardi A. Applying the Kirkpatrick model: Evaluating an Interaction for Learning Framework curriculum intervention. Issues Educ. Res. 2016; 26(3):490-507.
- Umoren R, Ezeaka VC, Fajolu IB, Ezenwa BN, Akintan P, Chukwu E, et al. Perspectives on simulation-based training from paediatric healthcare providers in Nigeria: a national survey.BMJ Open 2020;10:e034029.
- Jamie AH, Mohammed AA. Satisfaction with simulation-based education among Bachelor of Midwifery students in public universities and colleges in Harar and Dire Dawa cities, Ethiopia. Eur J Midwifery. 2019;3:19.
- Agha S, Alhamrani AY, Khan MA. Satisfaction of medical students with simulation based learning. Saudi Med J. 2015;36(6):731-6.
- Gudayu TW, Badi MB, Asaye MM. Self-efficacy, learner satisfaction, and associated factors of simulation-based education among midwifery students: a cross-sectional study. Educ. Res. Int. 2015, Article ID 346182, 7 pages.
- Blackmore A, Kasfiki EV, Purva M. Simulation-based education to improve communication skills: a systematic review and identification of current best practice. BMJ Simul Technol Enhanc Learn. 2018;4(4):159-64.
- Greenberg CC, Regenbogen SE, Studdert DM, Lipsitz SR, Rogers SO, Zinner MJ, et al. Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg. 2007;204(4):533–40.
- Nguyen BT, Nguyen VA, Blizzard CL, Palmer A, Nguyen HT, Quyet TC, et al. Using the Kirkpatrick Model to Evaluate the Effect of a Primary Trauma Care Course on Health Care Workers' Knowledge, Attitude, and Practice in Two Vietnamese Local Hospitals: Prospective Intervention Study. JMIR Med Educ. 2024;10:e47127.
- Brown HA, Tidwell C, Prest P. Trauma training in low- and middle-income countries: A scoping review of ATLS alternatives. Afr J Emerg Med. 2022;12(1):53-60.
- Shehu NY, Okwor T, Dooga J, Wele AM, Cihambanya L, Okonkon II, et al. Train-the-trainers intervention for national capacity building in infection prevention and control for COVID-19 in Nigeria. Heliyon. 2023;9(11):e21978.
- Eguzo K, Okwuosa C, Ekanem U, Akwaowo C, Mkpang E. Use of Simulation-Based Training for Cancer Education among Nigerian Clinicians. J Clin Res Oncol 2018;1(2):1-6.
- Akiode A, Fetters T, Daroda R, Okeke B, Oji E. An evaluation of a national intervention to improve the postabortion care content of midwifery education in Nigeria. Int J Gynaecol Obstet. 2010;110(2):186-90.
- Bacon DR. Reporting Actual and Perceived Student Learning in Education Research. J. Mark. Educ. 2016; 38(1) 3–6.