Ectopic Pregnancy: A Review of Prevalence, Clinical Presentation and Outcome in Gusau, Northwest, Nigeria
Shittu A. Muhammad,MBBS,FWACS,MSc, Stephen O. Olaoye,MBBS,FWACS, Tetunde B. Aremu-Kasumu MBBS, FWACS, Olaniyi T. Fasanu,MBChB,MWACS
Abstract
Background: The prevalence of ectopic pregnancy in Zamfara state is unknown and gynaecological emergency admissions for this condition are on the increase.
Aim: To determine the prevalence, risk factors, clinical presentation and outcome of patients managed for ectopic pregnancy at the Federal Medical Centre Gusau, Zamfara State, Nigeria, from January 2014 to December 2020.
Methodology: This was a retrospective study of ectopic pregnancies at Federal Medical Centre Gusau, Nigeria from January 2014 to December 2020. Participants’ medical records were retrieved to collate socio-demographic, clinical characteristics, management and outcome information. Data was analysed with SPSS software version 26. Means, frequency and percentages were used to present the significance of the results.
Result: A total of 64 women were managed for ectopic pregnancy between January 1st 2014 and December 31st 2020 in Federal Medical Centre, Gusau. During this period, there were 20,836 deliveries, giving an incidence of 0.31% (3.1 per thousand deliveries). The Mean age of the patients was 27.4 ± 5.5 years. Amenorrhea, abdominal pain and vaginal bleeding were the most common presentations (100%, 98.4% and 96.9% respectively). The commonest risk factor was a previous history of unsafe abortion in 18/64 (28.1%). The ectopic pregnancy was ruptured in 57 of 64 patients (89.1%), and 5 (8.8%) presented in hypovolaemic shock. Laparotomy was done for all the patients and salpingectomy was performed in 98.4%. Anaemia was the most common complication in 45 of 64 (70.3%) necessitating blood transfusion. There was no case fatality in the study.
Conclusion: The incidence of ectopic pregnancy in our centre was low, the most common risk factor was a previous history of unsafe abortion. The majority of the patients presented late with an already ruptured ectopic pregnancy. Early localisation of pregnancy with the aid of an ultrasound in women with a missed period would identify those with an ectopic pregnancy before it ruptures.
Keywords: Ectopic pregnancy, clinical presentation, tubal rupture, salpingectomy, Nigeria.
Introduction
The desire to procreate may end up with an unpleasant experience and severe acute life-threatening condition that may change such wish to melancholy. An ectopic pregnancy is a pregnancy that is implanted outside the endometrial lining of the uterine cavity1-5.
Most ectopic pregnancies are unilateral, sparing the contralateral fallopian tube. An ectopic pregnancy rarely occurs in the abdominal cavity. Other rare sites are ovaries, cervix, and uterine cornu.4
It is an important contributor to maternal morbidity and mortality in the first trimester of pregnancy6.
The global estimated prevalence of ectopic gestation is 1-2% of all pregnancies7, the case-fatality rates for ectopic pregnancy in most under-developed communities (low and middle income countries, LMICs) is 1-3% and this figure is ten-folds those of advanced countries.1,2,4
The majority of women with ectopic pregnancy have no known risk factors, however, evidence has shown that conditions associated with damage to the fallopian tubes are the major risk factors for the development of ectopic pregnancy.1,2,4,8 Among these factors are pelvic infections, previous abdominal and pelvic surgeries1,8 cigarette smoking, and previous ectopic pregnancy.7,9 Sexually transmitted infection with Chlamydia trachomatis has been associated with between 30 to 50% of all cases of ectopic gestations.3
There is a rising trend in the incidence of ectopic pregnancy worldwide as a result of many factors including the high prevalence of pelvic inflammatory diseases, puerperal and post-abortion sepsis, and in vitro fertilisation (IVF),3,8 but there has been a correspondingly marked reduction in the diagnosis of ruptured ectopic pregnancy.1 This decline is probably due to the use of the highly sensitive quantitative serum ßHCG assay, high-resolution transvaginal ultrasound scan and the availability of minimal access surgery for the early diagnosis of unruptured ectopic.9-11
The clinical presentation of ectopic pregnancy is variable, and is dependent on the location or whether it is ruptured or unruptured.8,9
Symptoms of ectopic pregnancy include sudden onset of severe lower abdominal pain followed by vaginal bleeding after a period of 6 to 10 weeks amenorrhea, nausea, vomiting and occasionally diarrhoea. Symptoms of hypovolaemia are not unusual in a patient with ruptured ectopic pregnancy. Abdominal tenderness, rigidity, guarding and rebound tenderness are features of haemoperitoneum.2 Sometimes ectopic pregnancy presents with uncommon symptoms and signs, then a high index of suspicion is required to make a diagnosis in such atypical presentations.8,12
Despite the diverse modes of clinical presentations of ectopic pregnancy, a tenth of cases will have no complaints2,7 and about a third will have no clinical sign on presentation.2
There has been a remarkable improvement in the treatment modalities for ectopic pregnancy over the decades, from the most invasive exploratory laparotomy approach to either the minimally invasive laparoscopic surgical approach or the medical management with methotrexate or expectant management.13,14
The minimally invasive surgical approach is rapid.6,10 All forms of interventions that are traditionally carried out at exploratory laparotomies, such as salpingectomy, salpingostomy, salpingotomy and tubal milking of the gestational sac are also possible at laparoscopy.10
The aim of this study is to determine the prevalence, risk factors, clinical presentation and outcome of patients managed for ectopic pregnancy at the Federal Medical Centre Gusau, Zamfara State, Nigeria, from January 2014 to December 2020
Methodology
This was a retrospective study of ectopic pregnancies at the Federal Medical Centre, Gusau, Zamfara State in North-Western Nigeria between January 2014 and December 2020. The medical records of all the patients who were managed for ectopic pregnancies in the hospital during the period under review were retrieved. The search included records from the theatre, labour ward and gynaecological emergency ward of the hospital. From the obstetrics and gynaecology operation registers, a list of patients who underwent surgeries for ectopic pregnancy was compiled and compared with the admission records in the wards. The case folders of the patients were retrieved from the medical records department.
Records of all deliveries for the same period were obtained from the maternity section of the hospital. Information on the socio-demographic characteristics, clinical symptoms and signs, sites and treatment options, risk factors for the disease and the associated morbidity were extracted and collated on a Microsoft Excel sheet.
Ethical Consideration
Ethical approval was obtained from the ethical committee of the hospital. Information obtained from the patients’ folders was kept confidential and the data was stored in the laptop of two of the authors and on the desktop of the departmental secretary.
Data Analysis
Data obtained was collated using a Microsoft Excel sheet and uploaded to SPSS IBM version 26 (IBM, Chicago, Illinois, USA) and analysed. Descriptive statistics was used for frequencies, percentages and means to present the significance of the result. The results are presented in tables and figures where appropriate.
Results
There were 20,836 deliveries between 1st January 2014 to 31st December 2020 in Federal Medical Centre, Gusau. During this period, 64 women were admitted and managed for ectopic pregnancy, giving a prevalence of 3.1 per thousand deliveries. The Mean age of the patients was 27.4 ± 5.5 years, though it ranged between 15 and 38 years with the majority (34.4%) of them being between 25 and 29 years. Thirteen patients (20.3%) were nulliparous and 15 (23.4%) had five or more deliveries. The mean gestational age was 7.0 ± 2.1 weeks. Most of the ectopic pregnancies (84.4%) were at a gestational age of less than 9 weeks, and almost all the patients presented in the first trimester (Table 1).
Table 1: Summary of demographic characteristics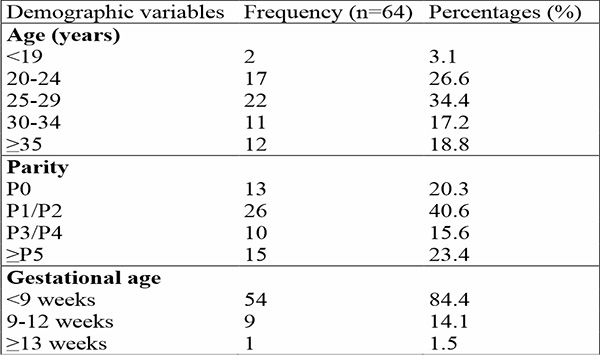
The presentation of the patients varied; however, amenorrhea was the most common clinical feature, and it was found in all the patients. This was followed by abdominal pain and vaginal bleeding in 98.4% and 96.9% of the patients respectively. Other clinical features include pallor, nausea and vomiting and adnexal mass on examination. The ectopic pregnancy was found to be ruptured in 57 of 64 patients (89.1%) and 5 (8.8%) of those with ruptured ectopic pregnancy presented with hypovolaemic shock (Table 2).
Table 2: clinical features of ectopic pregnancy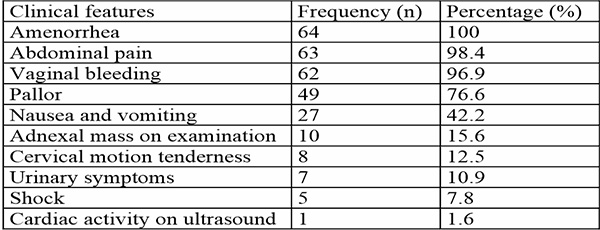
The most common risk factor for ectopic pregnancy was a previous history of unsafe abortion and it was found in 28.1% (18 of 64) of the patients. The other risk factors include history of pelvic surgery, previous history of PID and previous history of infertility.
Table 3: Risk factors for ectopic pregnancy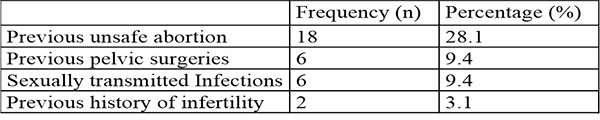
The commonest site of implantation of the ectopic pregnancy was the fallopian tube, in 63 of 64 patients (98.4%). The ampullary region was the most common site in women diagnosed with tubal pregnancy, 47 of 63 patients (74.6%). Other sites included the fimbrial, the isthmic and the interstitial portions. Ovarian ectopic pregnancy was found in one patient (1.6%). (Table 4).
Table 4: Sites of ectopic pregnancy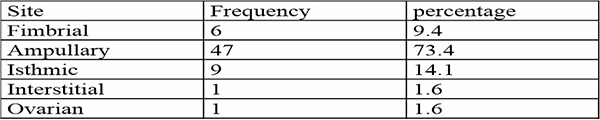
Laparotomy was done for all the patients and salpingectomy was the choice of surgery in 98.4% (63 of 64 patients). Oophorectomy was done alongside salpingectomy in two patients.
The most common complication of ectopic pregnancy was anaemia, which was found in 45/64 (70.3%) of the patients, necessitating blood transfusion in 95.6% of the patients. None of the patients developed post-operative sepsis and there was no case fatality recorded.
Discussion
Ectopic pregnancy is a common life-threatening emergency in gynaecological practice. It is an important contributor to maternal morbidity and mortality with far-reaching consequences on the subsequent fertility of women.
The prevalence of ectopic pregnancy in our study was 3.1 per thousand deliveries, this is similar to findings from a study done by Etuknwa et al in South-South, Nigeria.4 However, this is lower than the 2.1% quoted by Lawani et al.15, 1.68% by Gharoro et al16 and 18.1 per thousand by Alrede et al17. More recent studies by Chukwu et al in the South-Eastern region and Ononuju et al in North-Central Nigeria both quoted an incidence of 0.89%,18,19 though higher than the incidence from our study; is lower than those reported in older literature. This could suggest a lower trend in the prevalence of ectopic pregnancy in our environment.
This review showed that the peak ages of presentation of ectopic pregnancy were between 25 and 29 years, this is consistent with reports from Etuknwa et al and Ononuju et al.4,19 Given that this is the age at which sexual activity and reproduction reach their pinnacle20, it is scarcely surprising.
The risk factors for ectopic pregnancy found in this series were previous history of unsafe abortion, history of PID, history of pelvic surgeries and infertility, this is consistent with findings from Gharoro et al. and John et al.16,21 This also helps to corroborate the hypothesis that the common mechanism for the occurrence of ectopic pregnancy is tubal injury.22
The majority of the patients presented with a ruptured ectopic pregnancy and the commonest site of the ectopic pregnancy was the ampullary region of the fallopian tube. This is is similar to reports from other Nigerian studies.15,16,21 This supports the fact that people in lower-middle-income countries such as Nigeria have poor health-seeking behaviours.21 This is hardly surprising considering the cumulative effect of high levels of poverty, low levels of education, limited accessibility to healthcare facilities and limited healthcare insurance policies in these countries, where patients have to pay out of pocket.
Some patients presented in hypovolaemic shock from massive blood loss as a result of ruptured ectopic pregnancy. In such women, an immediate resuscitation and definitive surgery are important to prevent morbidity and mortality.
Open laparotomy and salpingectomy were the mainstay of treatment in our study, this is also similar to findings in their Nigerian studies.18,19 However, in developed countries, minimally invasive surgery via laparoscopy has become the preferred surgical modality as a result of reduction in the estimated intraoperative blood loss, postoperative hospital stay, postoperative analgesic requirement, time to return to normal activity, and total hospital cost.23
Laparotomy was the surgical approach used for all the patients in this review and salpingectomy was done in most, however, other more conservative surgical options have been described such as salpingotomy and salpingostomy.24 This is because the majority of the patients presented with a ruptured ectopic pregnancy. Where the ectopic pregnancy is unruptured, medical and conservative management are options.25
In this review, anaemia was found in 70.3% of the patients and 95.6% of them had blood transfusion, this was similar to reports of 67.3% and 93.9% documented by Egwuatu et al.26 This places more demand on the already constrained health resources in our environment, and underscores the importance of early presentation before a complication arises. Maternal mortality due to ectopic pregnancy reported in various studies is between 0% and 3.0%.4,16,27 This may be an underestimation as many patients may die before presentation to the hospital.16 There was no case fatality in our study.
This study was cross-sectional with retrospective data collection. Also, this study could not evaluate the fertility outcomes of the patients that were reviewed in the study; therefore further prospective longitudinal studies are recommended to identify the trends and fertility outcomes among those who have been managed for ectopic pregnancy.
The prevalence of ectopic pregnancy in our centre is low. The most common risk factor is a history of unsafe abortion and the majority of the patients presented late with an already ruptured ectopic pregnancy. Appropriate management of abortion could reduce the prevalence of ectopic pregnancy. Also, Early localisation of pregnancy with the aid of an ultrasound in women with a missed period would identify those with an ectopic pregnancy before it ruptures.
References
- Yeasmin MS, Uddin MJ, Hasan E. A clinical study of ectopic pregnancies in a tertiary care hospital of Chittagong, Bangladesh. Chattagram Maa-O-Shishu Hospital Medical College Journal. 2014 Nov 28;13(3):1-4.
- Bello OO, Akinajo OR. A 10-year review of ectopic pregnancy at University College hospital, Ibadan Nigeria. Glob J Med Res. 2018;18:7-11.
- Olamijulo JA, Okusanya BO, Adenekan MA, Ugwu AO, Olorunfemi G, Okojie O. Ectopic pregnancy at the Lagos University Teaching Hospital, Lagos, South-Western Nigeria: Temporal trends, clinical presentation and management outcomes from 2005 to 2014. Nigerian Postgraduate Medical Journal. 2020; 27(3): 177-183
- Etuknwa BT, Azu OO, Peter AI, Ekandem GJ, Olaifa K, Aquaisua AN, Ikpeme E. Ectopic pregnancy: A Nigerian urban experience. Korean Journal of Obstetrics & Gynecology. 2012; 55(5): 309-314.
- Banu H, Hui JW, Hua L. Role of Laparoscopy in Management of Ectopic Pregnancy. Journal of Enam Medical College. 2015; 5(3): 170-174.
- Ikechebelu JI, OKAFOR CD. Laparoscopic salpingectomy for ruptured tubal ectopic pregnancy: A case report. Annals of Medical and Health Sciences Research. 2017; 7:203-205.
- Jurkovic D, Wilkinson H. Diagnosis and management of ectopic pregnancy. BMJ 342, jun10 1: d3397, 2011. doi: 10.1136/bmj.d3397.
- Orazulike NC, Konje JC. Diagnosis and management of ectopic pregnancy. Women’s Health. 2013 Jul;9(4):373-385.
- Patel M, Chavda D, Prajapati S. A retrospective study of 100 cases of ectopic pregnancy: clinical presentation, site of ectopic and diagnosis evaluation. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2016 Dec 7;5(12):4313-4316.
- Ding DC, Chu TY, Kao SP, Chen PC, Wei YC. Laparoscopic management of tubal ectopic pregnancy. JSLS: Journal of the Society of Laparoendoscopic Surgeons. 2008; 12(3):273-276.
- Baggio S, Garzon S, Russo A, Ianniciello CQ, Santi L, Laganà AS, Raffaelli R, Franchi M. Fertility and reproductive outcome after tubal ectopic pregnancy: comparison among methotrexate, surgery and expectant management. Archives of Gynecology and Obstetrics, 2021; 303: 259-268.
- Clement WF, Ijeoma NE, Ledee KP. Ectopic pregnancy in Rivers State University Teaching Hospital, Port Harcourt, southern Nigeria: a five-year review. World Journal of Advanced Research and Reviews. 2020; 6(2): 44-53.
- Akaba GO, Agida TE, Onafowokan O. Ectopic pregnancy in Nigeria's federal capital territory: a six year review. Nigerian journal of medicine, 2012; 21(2): 241-245.
- Dubuisson JB, Morice P, Chapron C, De Gayffier A, Mouelhi T. Salpingectomy-the laparoscopic surgical choice for ectopic pregnancy. Human reproduction. 1996; 11(6): 1199-1203.
- Lawani OL, Anozie OB, Ezeonu PO. Ectopic pregnancy: a life-threatening gynaecological emergency. International journal of women's health. 2013; 5: 515-521.
- Gharoro EP, Igbafe AA. Ectopic pregnancy revisited in Benin City, Nigeria: analysis of 152 cases. Acta obstetricia et gynecologica Scandinavica. 2002; 81(12): 1139-1143.
- Alrede, LR and Ekele BA. Ectopic pregnancy in Sokoto, Northern Nigeria. Malawi Medical Journal. 2005; 17(1): 14-16.
- Chukwu JA, Agulanna AE, Okafor IA, Nwakanma AA, Osuji BC. A decade study of the incidence and clinical analysis of ectopic pregnancy at a tertiary hospital in Eastern Nigeria. Int J Reprod Contracept Obstet Gynecol. 2022; 11(2): 315-322.
- Ononuju CN, Ogbe AE, Changkat LL, Okwaraoha BO, Chinaka UE. Ectopic pregnancy in Dalhatu Araf specialist hospital Lafia Nigeria–A 5-year review. Nigerian Postgraduate Medical Journal. 2019; 26(4): 235-238.
- Udigwe GO, Umeononihu OS, Mbachu II. Ectopic pregnancy: A 5 Year Review of Cases at Nnamdi Azikiwe University Teaching Hospital (NAUTH) Nnewi. Nigerian Medical Journal, 2010; 51(4): 160-163.
- John CO, Alegbleye JO. Ectopic pregnancy experience in a tertiary health facility in South-South Nigeria. Nigerian Health Journal. 2016; 16(1): 2-5.
- Shaw JLV, Dey SK, Critchley HOD, Horne AW. Current knowledge of the aetiology of human tubal ectopic pregnancy. Human Reproduction Update, 2010; 16(4): 432-444.
- Miao H. Comparative Analysis of Laparoscopy Versus Laparotomy Approaches in Treating Ectopic Pregnancy. Advances in Obstetrics and Gynecology Research. 2023; 1(3): 33-37.
- Ozcan MC, Wilson JR, Frishman GN. A systematic review and meta-analysis of surgical treatment of ectopic pregnancy with salpingectomy versus salpingostomy. Journal of minimally invasive gynecology. 2021; 28(3): 656-667.
- Newbatt E, Beckles Z, Ullman R, Lumsden MA. Ectopic pregnancy and miscarriage: summary of NICE guidance. BMJ 2012;345:e813-6.
- Egwuatu EC, Okafor CG, Eleje GU, Umeononihu OS, Okoro CC, Mamah JE, Njoku TK, Oguejiofor CB, Okafor CC, Okeke CF, Ogabido CA. Ectopic Pregnancies in a Tertiary Hospital in Nigeria: A 10-Year Retrospective Experience. American Journal of Clinical Medicine Research. 2023; 11(2): 35-40.
- Igwegbe AO, Eleje GU, Okpala BC. An appraisal of the management of ectopic pregnancy in a Nigerian tertiary hospital. Annals of medical and health sciences research. 2013; 3(2): 166-170.