Vulva lesions seen at a tertiary health centre in southwest Nigeria
Olaofe OO
Abstract
Background: Some researchers have emphasised the need for more studies on vulvar cancers. The aim of our study is to describe the vulvar lesions identified in biopsies seen in our department over a five-year period to serve as baseline data for future studies.
Methods: We conducted a five-year cross-sectional study on all vulva specimens received by the department of Morbid Anatomy and Forensic medicine at the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife, Nigeria. From the departmental records, we retrieved data on the patients' biodata, medical history, and vulva lesion diagnosis.
Results: We recorded 15 vulva biopsies during the study period, with an age range of 13 to 80 years. Two cases were benign tumours, and two cases were inflammatory in nature. A case of a pre-malignant lesion was seen. Nine cases were malignant tumours, all of which are epithelial in origin. We saw two non-neoplastic lesions. These are acute on chronic inflammation and lichen sclerosus et atrophicus.
Of the malignant tumours seen, five were well-differentiated squamous cell carcinoma (SCC), two were moderately differentiated SCC, and two were cases of verrucous carcinoma. One case of verrucous carcinoma and a well-differentiated SCC had a background HIV.
Conclusion: Vulva lesions are rarely seen at our centre. The absence of preinvasive lesions in our study may be due to the late presentation of cases in clinics or the reluctance of gynaecologists to take biopsies of non-tumoral lesions of the vulva. HIV may be associated with an increased risk of HPV-related cancers.
Keywords: Vulva Neoplasms, HIV Infections, Papillomavirus Infections, Squamous Cell Carcinoma
Introduction
Vulvar biopsies are rare in many health centers. Hence, many lesions of the vulva are rarely diagnosed by pathology laboratories.
The most important lesion diagnosed in vulvar biopsies is squamous cell carcinoma. This is more or less a forgotten disease, despite the fact that there has been an increase in its incidence in some regions of the world.1 Researchers focus more on the more common gynaecological tumours, to the detriment of this important disease.
Vulvar cancer is mainly associated with high-risk types of human papilloma viruses (HPV). This is particularly true in low-income countries where there is a relatively high incidence of HPV infection, partly due to the low use of HPV vaccines. In more developed countries where there is a lower incidence of HPV infection, vulvar cancers are usually associated with non-infectious causes like Lichen sclerosus et atrophicus.2 Although different molecular events have been identified in HPV and non-HPV-related vulvar cancers, the treatment has remained the same.3
Like cervical cancer, vulvar cancer has preinvasive lesions that can easily be detected and managed appropriately to prevent invasive carcinoma. A high-grade vulvar intraepithelial neoplasm is known to have a high risk of transformation into an invasive carcinoma. Unfortunately, because of the rarity of the tumour, there is no widely used screening method. However, early detection is required and strongly associated with a good prognosis.
Many of the chronically irritative lesions commonly associated with intensive pruritus are associated with vulvar carcinoma. Some vulva lesions not caused by HPV, particularly lichen sclerosus, are known to transform into invasive carcinomas. Prompt identification and proper management of these diseases may prevent the development of a malignant lesion.
There are various morphological types of squamous cell carcinoma (SCC) of the vulva. These include well differentiated SCC, moderately differentiated SCC, and poorly differentiated SCC. Verrucous carcinoma is also a form of squamous cell carcinoma that can involve the vulva.
Vulvar cancer commonly affects elderly, postmenopausal women. This has been related to atrophic changes that occur in this age group following atrophy of the genital organs.
Condyloma acuminatum, a tumour caused by low-risk HPV types, can also involve the vulvar. It is usually unsightly and commonly excised, with very little chance of recurrence if appropriately managed.
Some researchers have emphasised the need for more studies on vulvar cancers.4 The aim of our study is to describe the vulvar lesions identified in biopsies seen in our department over five years (January 1, 2018, to December 31, 2022) to serve as baseline data for future studies.
Methods
From January 1, 2018, to December 31, 2022 (a span of five years), we conducted a cross-sectional investigation on all vulva specimens received by the department of Morbid Anatomy and Forensic medicine at the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife, Nigeria. Nigeria's southwest is home to the Obafemi Awolowo University Teaching Hospitals Complex. The study was approved by the ethics and research committee in our institution. From the departmental records, we retrieved data on the patients' biodata, medical history, and vulva lesion diagnosis. To verify the diagnosis noted in the records, we examined each case.
Every instance with biodata and accessible histopathological reports was included. Cases without tissue and biodata were disregarded. We looked at fourteen vulva specimens. The absence of data only applied to one case.
We used Microsoft Excel to construct the data after extracting it. Excel was the programme we used to analyse the data.
Results
There were 15 vulva biopsies during the study period, with an age range of 13 to 80 years. One case was excluded because of missing data. Two cases were benign tumours, and two cases were inflammatory in nature. A case of a pre-malignant lesion was seen. Nine cases were malignant tumours, all of which are epithelial in origin.
The benign tumours, of which there were two cases, are epithelial in origin. There was no benign mesenchymal tumour. All the benign tumours are condyloma acuminatum. There were no background illnesses in any of the patients with condyloma acuminatum.
There were two non-neoplastic lesions. These are acute on chronic inflammation and lichen sclerosus et atrophicus. These lesions are seen at a very wide range of ages.
Of the malignant tumours seen, five were well-differentiated squamous cell carcinoma, two were moderately differentiated squamous cell carcinoma, and two were cases of verrucous carcinoma. One case of verrucous carcinoma and a well-differentiated squamous cell carcinoma had a background infection with the human immunodeficiency virus (HIV). A case of moderately differentiated squamous cell carcinoma had a background of cervical cancer that was successfully treated in the past. The average parity for each of the malignant entities was greater than four. We could not obtain information on the level of education and socio-economic status of the patients. Table 1 below shows the details of the various vulva lesions seen in our study.
Table 1: The age, parity, and background characteristics of the vulva lesions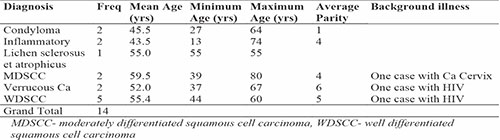

Figure 1: Photomicrograph of a condyloma acuminatum of the vulva in a young woman
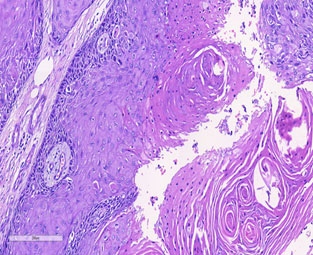
Figure 2: Photomicrograph of a well differentiated squamous cell carcinoma of the vulva in an elderly woman
Figures 1 and 2 show a photomicrograph of a condyloma acuminatum and a well differentiated squamous cell carcinoma of the vulva respectively.
Discussion
Vulva lesions are rarely seen at our centre. This is in conformity with reports from other researchers. It has been reported that many of these diseases have been relegated to the background and almost forgotten because of their rarity.1,5 The attention of physicians has been more focused on the more common cervical, endometrial, and ovarian cancers. It is important to know that these lesions still exist and to regularly report data on them to know if there are changing patterns or modes of presentation. It is also important to check if there are previously unknown conditions that may be associated with them.
Condyloma acuminatum of the vulva has been reported by many researchers. It is a benign epithelial tumour that is believed to be caused by low-risk human papilloma viruses (HPV). It can be found in the young and old, as seen in our study. It may be an indication for seeking the presence of sexually transmitted diseases, as infection by low-risk HPV may be accompanied by infection by high-risk HPV. Fortunately, this tumour is benign and can be appropriately managed by gynaecologists, but it is important for pathologists to be able to identify this tumour and distinguish it from the more aggressive verrucous carcinoma. In our experience, condyloma may be associated with a progressive lesion, an invasive squamous cell carcinoma. Hence, a complete excision and thorough examination of all areas of the specimen should be done to make sure the appropriate lesion is managed.6–8
In our study, we noticed a single case of lichen sclerosus et atrophicus in a middle-aged woman. This is a highly pruritic lesion that has the potential to transform into a malignant lesion. It is important that pathologists are aware of this disease entity, as the patient needs to be managed appropriately and monitored for disease progression.9,10
We did not identify any cases of pre-invasive intraepithelial lesions. It is known that, similar to squamous cell carcinoma in other organs, vulvar epithelial cancers have preinvasive lesions that can be identified long before malignant or aggressive transformation takes place.11–13 The absence of preinvasive lesions in our study may be due to the late presentation of cases in clinics or the reluctance of gynaecologists to take biopsies of non-tumoral lesions of the vulva. A specific study directed to look for this behaviour is required to make a conclusive statement regarding the cause of the absence of preinvasive lesions.
It is important to emphasise to the medical community that vulva cancer still exists, particularly in postmenopausal women. Early detection of cancerous or preinvasive lesions will substantially improve the prognosis of these cases. As the number of cases reported is generally low, the introduction of screening programmes may not be the best alternative to reducing the disease burden. Fortunately, many of the lesions are locally aggressive and may not metastasize early; hence, patient education directed at elderly women may be most beneficial in preventing vulvar cancers.14–16
We found a patient who has had treatment for cervical carcinoma in the past. She was believed to be disease-free before developing a moderately differentiated squamous cell carcinoma of the vulvar. It is very essential that patients who have had cervical cancer are continually monitored for the development of cancers in other organs of the female reproductive tract. The high-risk HPV, which is responsible for many cervical cancers, is well-known to cause vaginal and vulva squamous carcinomas. It is also necessary to monitor these patients, as radiotherapy commonly used to treat locally invasive cervical cancers can cause secondary malignant tumours unrelated to HPV infection. One of these is angiosarcoma.17,18
Two of the patients with vulva cancer had background immunosuppression caused by HIV. Unlike cervical cancer, which is an AIDS-defining illness, vulvar cancer is not as strongly associated with HIV/AIDS. However, it is known that many patients exposed to HIV are commonly co-infected with other sexually transmitted diseases, including high-risk HPV. HIV is associated with an increased risk of HPV-related cancers.19–22 This probably explains the co-occurrence of these diseases in the two patients seen in our study.
It is interesting to note that most of the cases of vulvar cancers are well-differentiated squamous cell carcinomas that are generally known to be less aggressive than the poorly differentiated or moderately differentiated subtypes. This has the great advantage that many of the lesions can be easily diagnosed without ancillary tests like immunohistochemistry. It is also advantageous, as many of the patients can be cured by wide local excision. This is important as our cases are managed in a resource-limited setting.
From our experience, some of the malignant lesions were diagnosed as inflammatory lesions in the initial biopsies but eventually correctly identified as malignant after one or two repeat biopsies. Many of the lesions are accompanied by intense inflammatory infiltrates, either as a result of the precursor inflammatory lesion or as a reaction of the stroma of the vulvar tissue to infiltration by malignant squamous cells. The production of keratin in the stroma elicits an intense inflammatory reaction. It is important that gynaecologists and pathologists are aware of this and have a high index of suspicion of carcinomas in postmenopausal women, particularly those with high parity. They should not be quick to dismiss such lesions as inflammatory.
Due to the low number of cases seen in our centre, it is better to pool cases from different centres before definitive statements regarding risk factors and other associated features of vulvar cancers can be made.
Conclusion
Vulva lesions are rarely seen at our centre. Condyloma may be associated with a progressive lesion, an invasive squamous cell carcinoma. Hence, a complete excision and thorough examination of all areas of the specimen should be done to make sure the appropriate lesion is managed. The absence of preinvasive lesions in our study may be due to the late presentation of cases in clinics or the reluctance of gynaecologists to take biopsies of non-tumoral lesions of the vulva. HIV may be associated with an increased risk of HPV-related cancers.
Acknowledgement
We thank Dr. Chigozie Okongwu and Dr. James Oladele for the production of the photomicrographs and the retrieval of slides and tissue blocks of the cases.
References
- Clancy AA, Spaans JN, Weberpals JI. The forgotten woman’s cancer: vulvar squamous cell carcinoma (VSCC) and a targeted approach to therapy. Annals of Oncology. 2016 Sep;27(9):1696–705.
- Bucchi L, Pizzato M, Rosso S, Ferretti S. New Insights into the Epidemiology of Vulvar Cancer: Systematic Literature Review for an Update of Incidence and Risk Factors. Cancers (Basel). 2022 Jan 13;14(2):389.
- Xing D, Fadare O. Molecular events in the pathogenesis of vulvar squamous cell carcinoma. Semin Diagn Pathol. 2021 Jan;38(1):50–61.
- Kaur S, Garg H, Nandwani M. The Unmet Needs in the Management of Vulvar Cancer and a Review of Indian Literature. JCO Glob Oncol. 2022 Nov;8:e2200197.
- Preti M, Querleu D. Vulvar Cancer: Facing a Rare Disease. Cancers (Basel). 2022 Mar 20;14(6):1581.
- Samarska IV, Epstein JI. Condyloma Acuminatum of Urinary Bladder: Relation to Squamous Cell Carcinoma. Am J Surg Pathol. 2019 Nov;43(11):1547–53.
- Whitaker JA. Condyloma acuminatum of the urinary bladder with underlying squamous cell carcinoma: a case report. J Med Case Rep. 2022 Dec 1;16(1):449.
- Rafiei R, Eftekhari H, Granmayeh S, Nickhah N, Rafiee B. Extramammary Paget’s Disease Associated With Genital Wart and Lichen Sclerosus. Acta Med Iran. 2017 Sep;55(9):591–3.
- Fergus KB, Lee AW, Baradaran N, Cohen AJ, Stohr BA, Erickson BA, et al. Pathophysiology, Clinical Manifestations, and Treatment of Lichen Sclerosus: A Systematic Review. Urology. 2020 Jan;135:11–9.
- Sim SJY, Dear K, Mastoraki E, James M, Haider A, Ellery P, et al. Genital lichen sclerosus and melanoma; a systematic review. Skin Health Dis. 2023 Apr;3(2):e198.
- Thuijs NB, van Beurden M, Bruggink AH, Steenbergen RDM, Berkhof J, Bleeker MCG. Vulvar intraepithelial neoplasia: Incidence and long-term risk of vulvar squamous cell carcinoma. Int J Cancer. 2021 Jan 1;148(1):90–8.
- Deb PQ, Heller DS. Molecular Features of Preinvasive and Invasive Vulvar Neoplasms. J Low Genit Tract Dis. 2023 Jan 1;27(1):40–6.
- Jenkins TM, Mills AM. Putative precancerous lesions of vulvar squamous cell carcinoma. Semin Diagn Pathol. 2021 Jan;38(1):27–36.
- Mancini S, Bucchi L, Zamagni F, Baldacchini F, Crocetti E, Giuliani O, et al. Trends in Net Survival from Vulvar Squamous Cell Carcinoma in Italy (1990-2015). J Clin Med. 2023 Mar 10;12(6):2172.
- Viktora L, Minář L, Felsinger M, Weinberger V. Vulvar carcinoma and its recurrences - principles of surgical treatment. Ceska Gynekol. 2022;87(6):401–7.
- Shin DW, Bae J, Ha J, Lee WM, Jung KW. Trends in incidence and survival of patients with vulvar cancer in an Asian country: Analysis of the Korean Central Cancer Registry 1999-2018. Gynecol Oncol. 2022 Feb;164(2):386–92.
- Khaled CS, Sinno SAJ. Radiation-induced angiosarcoma of the vagina and vulva: Case report and review of literature. Gynecologic Oncology Reports. 2022 Jun 1;41:100990.
- Matsuo K, Blake EA, Machida H, Mandelbaum RS, Roman LD, Wright JD. Incidences and risk factors of metachronous vulvar, vaginal, and anal cancers after cervical cancer diagnosis. Gynecol Oncol. 2018 Sep;150(3):501–8.
- Lekoane KMB, Kuupiel D, Mashamba-Thompson TP, Ginindza TG. The interplay of HIV and human papillomavirus-related cancers in sub-Saharan Africa: scoping review. Systematic Reviews. 2020 Apr 22;9(1):88.
- Chaturvedi AK, Madeleine MM, Biggar RJ, Engels EA. Risk of Human Papillomavirus–Associated Cancers Among Persons With AIDS. JNCI: Journal of the National Cancer Institute. 2009 Aug 19;101(16):1120–30.
- Fanta MB. Vulvar cancer and HIV at a teaching hospital in Ethiopia. Gynecologic Oncology. 2019 Jun 1;154:279.
- Simbiri KO, Jha HC, Kayembe MK, Kovarik C, Robertson ES. Oncogenic viruses associated with vulva cancer in HIV-1 patients in Botswana. Infectious Agents and Cancer. 2014 Aug 24;9(1):28.