Assessment of depressive symptoms among post stroke patients attending a Nigerian tertiary hospital
Bakare AT1, Amin HH4, Adebisi A3, Abubakar A2, Yakubu AI2, Yahaya H3, Bello A3, Attahiru A2, Abdulsalam HS2, Ahmad M2, Shehu S3, Amira B2, Eneojo IS2, Lawal HA2, Yunusa MA1
Abstract
Background: Post Stroke Depression (PSD) occurs in a significant number of patients and constitutes an important complication of stroke, leading to greater disability as well as increased mortality. This study examined depressive symptoms among post stroke patients attending neurology clinic in a tertiary hospital in Northwest Nigeria.
Methods: This cross-sectional study was carried out among 83 stroke survivors. Participants were administered socio-demographic, clinical characteristics pro-forma questionnaire and depression subscale of the Hospital and Anxiety Depressive Scale (HADS).
Results: The 83 participants recruited for study had a mean age of 56.8 years (s.d. = 10.2) and 62.7 % were female. Majority (60.2%) had formal education, 83.1% were employed, and 73.5% were married. Overall, the prevalence of depressive symptoms was 34.9% while 2.4% were rated as having severe depressive symptoms. Unemployment, having disabilities and post stroke complications were significantly associated with depressive symptoms.
Conclusion: The presence of depressive symptoms among stroke patients supports the need to consider routine screen for psychiatry morbidity among patients with medical condition that causes disabilities. Disability has been identified as the main predictor of depressive symptoms. In view of this, psychosocial evaluation and intervention should be integrated into clinical care of stroke patients for early detection of depressive symptoms.
Keywords: Depressive-symptoms, stroke, patients, neurology
Introduction
Depression is associated with isolated lives, the absence of pleasure, and social and vocational impairment.1 Post-stroke depression (PSD) is frequent among stroke patients.2 PSD is associated with failure to maintain a proper diet and exercise regimen and to adhere to medical care.1 PSD occurs in a significant number of patients and constitutes an important complication of stroke, leading to greater disability as well as increased mortality.3 In a study conducted to access the level of anxiety and depression in post stroke patients in Jordan, exactly 74.5% of the participants exhibited symptoms of depression.4 Furthermore, in a study conducted to access the level of depressive in post stroke patients in Lagos state Nigeria, out of the 51 participants that completed the study,13 (25.5%) showed signs and symptoms of depression using Depression Anxiety Stress Scale, DASS-21.5
Post stroke depression has received less attention in the Northwestern Nigeria and the scanty or lack of research evidence in this region of Nigeria may deprive post stroke patients from the treatment of possible comorbid depression symptoms. Identification, treatment of post stroke patients with depressive symptoms and knowledge of associated factors may improve the quality of life of the patients. This study investigated the prevalence, socio-demographic, clinical correlates, and determinants of depressive symptoms among post stroke patients attending a tertiary hospital in Northwest Nigerian.
Materials and methods
Study design and setting: This cross-sectional study was conducted among 83 post stroke patients attending a neurology clinic in a Usmanu Danfodiyo University Teaching (UDUTH) Sokoto state, Northwest Nigeria. Data was collected over a period of 4 months from April 2022 to July 2022. Recruitment of participants was performed using non-probability convenience sampling of every eligible participant who met the study criteria (must be eighteen years and above, consented to participate, not too physically ill to participate in the study). Consecutive patients presenting at the clinic were interviewed until it was observed that almost all the patients with previous stroke who are regular at the follow up had been interviewed. All the 83 post stroke survivors gave informed consent to participate in the study.
Stroke diagnosis was determined using neuroimaging computerized tomography (CT) or magnetic resonance imaging (MRI) studies and the clinical judgment of the managing neurologists, as noted in participants' case folders. No participants reported a history of mental illness, which was an exclusion criterion in this study. Participants' case records were used to acquire information on their physical health and medication use.
Instruments and procedure: Socio-demographic and clinical characteristics questionnaire (SCQ) designed by the researchers and the depression subscale of the Hospital Anxiety and Depression Scale (HADS) were administered to the participants. The SCQ was administered to obtain socio-demographic and clinical data, other relevant clinical information was obtained from case notes. Computed Tomography (CT) scan or Magnetic Resonance Imaging (MRI) were used to categorize stroke subtypes as reported in the case notes. In the absence of radiological scans, stroke subtype was based on clinical assessment performed by the managing consultant neurologists. Study participants were also administered the depression subscale of HADS. HADS was formulated by Zigmond and Snaith, it is used to identify probable anxiety and depression among patients in nonpsychiatric clinical setting. It has seven anxiety and depression subscales each, rated from 0 to 3 and a maximum score of 21 and minimum of 0 for each. An HADS score of ≥8 was used as cutoff for presence of depression symptoms. A score of 8-10 is classified as mild anxiety, 11-15 moderate, and 16-21 severe depression symptoms.6 It usually takes 3-7 minutes to administer the HADS.
Ethical consideration: The study proposal was approved by the hospital (UDUTH) ethical committee. Following an explanation of the study's purpose, procedure, and expected duration of involvement, all participants provided informed consent. Other issues concerning participation, such as confidentiality and voluntariness, were also addressed. Those who were discovered to have depression symptoms were appropriately guided.
Data analyses: All data collected were coded and entered into the computer for analysis. Data were analysed using the Statistical Package for Social Sciences (SPSS) for windows Version 22.0. Mean (± SD), frequencies and percentages were used to describe data. Chi-square test analysed significance between categorical variables and depressive symptoms, Fischer’s exact test was used when the criteria for chi-square were not met. Binary logistic regression was used to determine the predictors of depressive symptoms. A confidence interval of 95% was used which allows for 5% sampling error at significance of ≤ 0.05.
Results
Participants
The eighty-three participants recruited for study had a mean age of 56.8 years (s.d.= 10.2), 62.7% were females, 60.2% had formal education, majority (83.1%) were employed, and 73.5% were married. A summary of characteristics of the participants is shown in Table 1.
Table 1: Sociodemographic characteristics of the participants
Ischaemic stroke was prevalent (71.1%) among the participants, 18 (21.7%) had haemorrhagic stroke, and 6 (7.2%) had unclassifiable stroke. Regarding the location of stroke, 25 (30.1%) of the participants had stroke located at the cortical region, 18 (21.7%) sub-cortical, 6 (7.2%) brainstem and 34 (41%) cerebellar. Hypertension was the prevalent (95.2%) risk factor for stroke among the participants. Most (97.6%) of the participants had one episode of stroke. Using the Modified Ranklin Scale (MRS) for assessment of disabilities after stroke, a few (3.6%) participants had no symptoms, 17 (20.5%) no significant disability (able to perform all usual duties and activities), 20 (24.1%) slight disability (unable to perform all previous activities) 20 (24.1%), moderate disability (requires some help), 6 (7.2%) moderate severe disability (unable to walk without assistance), 17 (20.5%) severe disability (bed ridden, incontinent, requires constant nursing care). This is summarised in table 2.
Table 2: Clinical characteristics of the post stroke survivors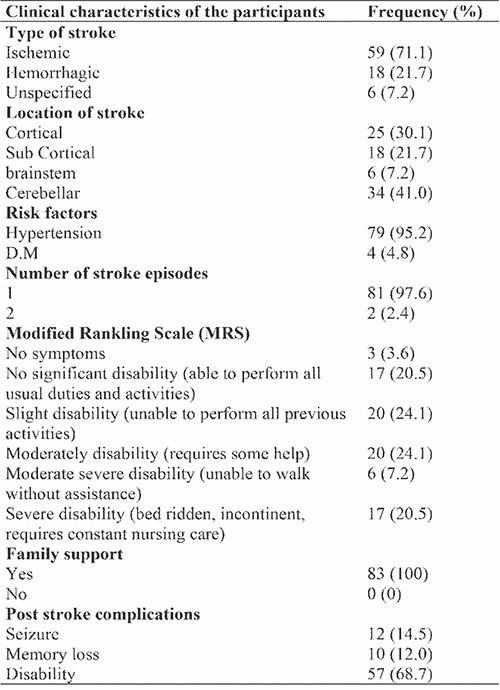
Table 3: Prevalence of depressive symptoms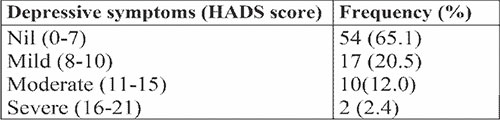
Table 3 shows the rates of depressive symptoms based on the severity (mild, moderate, and severe). Overall, the prevalence of depression symptoms was 34.9%.
Association between characteristics of the participants and depressive symptoms
The participants characteristics associated with depressive symptoms are shown in Table 4. Having disabilities (0.49 CI (0.02-0.17), p< 0.001) and having seizure (3.65 CI 1.36-9.76), p=0.01) were significantly associated with depressive symptoms. Furthermore, it is remarkable to note that higher proportion of participants that had depressive symptoms were 65 years old and above, male, had informal education, unemployed, not married, had haemorrhagic stroke, had stroke located at cortical region, and had non-vascular risk factors for stroke, even though these characteristics were not statistically significant.
Table 4: Association between characteristics of the participants and depressive symptoms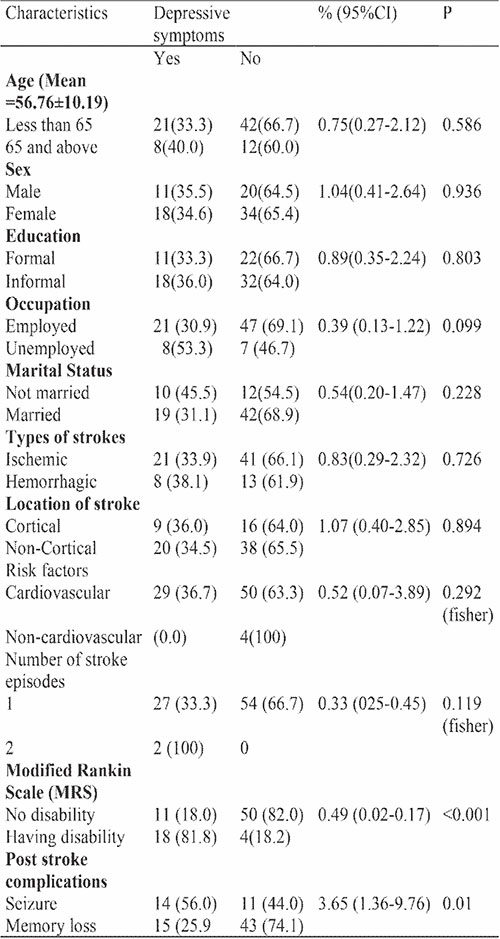
Table 5: Predictors of depressive symptoms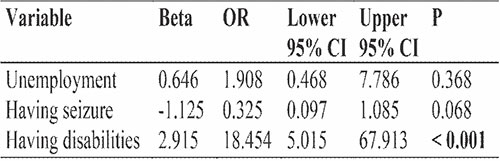
Predictors of depressive symptoms
Binary logistic regression analysis was used to determine the predictors of depressive symptoms among the two variables (having seizure, having disabilities) that were significantly associated with depressive symptoms. Having disabilities was the only characteristic that predict depressive symptoms (p< 0.001).
Discussion
Main findings and findings from other studies
We have assessed the prevalence of depressive symptoms and identified significant associated factors and predictors of depression symptoms among post stroke patients attending a neurology clinic at UDUTH. We found that the prevalence of depressive symptoms was high. However, those with severe symptoms were the least. Our estimate is consistent with previous research and deserves some comment. In previous observations, the incidence of depression ranged from 10 to 72%.7 These variations can be explained by methodological differences. Other studies used the DSM-IV (3) or research diagnostic criteria or diagnostic tools such as the Present State Examination (PSE), Hamilton Depression Rating Scale, and Composite International Diagnostic Interview.8
Guidelines on rehabilitation after stroke have also recommended that patients are screened again at 6 months and annually thereafter.9 The use of self-administered screening instruments in our study could explain higher prevalence rates when compared to assessments done with diagnostic interview scales due to stringent diagnostic criteria. The Hospital Anxiety and Depression Scale-Anxiety subscale ‘probable’ and ‘possible’ cutoff scores (≥ 8) were the most widely used assessment criteria10 which are in concordance with our study.
Having disabilities and the presence of complications following stroke were significantly associated with depressive symptoms. The findings in our study correspond with what was reported in a previous study. Participants with PSD were significantly more likely to be unemployed, and paid more for overall treatment when compared to those without PSD.11 This emphasizes the importance of being unemployed before stroke or loss of job as an outcome of disabilities post stroke. These findings are not out of place, especially in developing countries where job loss could eventually lead to inability to meet financial obligations coupled with the lack of social services. Contrary to the findings of our study, a study reported no significant association between depressive symptoms and stroke-related clinical characteristics (type of stroke, side of stroke and co-morbidity). This phenomenon suggests that depressive symptoms, instead of originating from the pathological development of stroke, may be a psychological consequence arising from the disrupted activity of daily living (ADL) functioning and the difficult life experiences after the incidence of stroke. However, it is equally likely that poor ADL functioning is a consequence of depressive symptoms.9
Our study showed a peculiar trend as higher proportions of participants with PSD were older, had more than one episode of stroke, stroke located in the cortical area, ischaemic stroke, informal education, were unmarried, and female, but these findings were not statistically significant. In contrast, a study found that gender and self-reported physical diseases other than stroke were significantly associated with depressive symptoms.4 Multivariable analysis found that self-reported unmarried status (odds ratio, 3.27; 95% confidence interval, 1.44-7.44), excessive fatigue (odds ratio, 4.46; 95% confidence interval, 1.87-10.63), and depression (odds ratio, 1.24; 95% confidence interval, 1.16-1.33) were independently associated with PSD.12 This difference may be due to the relatively small sample size recruited in our study.
The type of stroke or lesion location are not significantly associated with post stroke depression. Available clinical data on the relationship between PSD and lesion location are conflicting. Patients with acute frontal lobe infarction were more likely to have PSD.13
Although degree of stroke disability is usually dependent on factors such as health-care setting, type of stroke (hemorrhagic or ischemic), the location of stroke, and the extent of tissue damage, some recovery is usually made by a good number of stroke survivors; hence, severe physical loss may be transient.14 However, the potential of a reoccurrence often makes stroke to constitute a long-lasting threat. The possibility of future strokes and loss of independence are likely explanatory factors for predisposition of stroke survivors to the experience of depression.11 This study represents a significant contribution to literature on the significance of PSD in the management of post stroke patients especially in the hospital where the study was conducted.
Conclusion and Recommendations
The presence of depressive symptoms among stroke patients supports the need to consider routine screen for psychiatry morbidity among patients with medical condition that causes disabilities. Disability has been identified as the main predictor of depressive symptoms. In view of this, psychosocial evaluation and intervention should be integrated into clinical care of stroke patients for early detection of depressive symptoms.
Limitations
There were certain limitations to our study. The small number of the participants is a major limitation. Also, patients with severe clinical state like having severe cognitive impairment and aphasia were excluded which limits the generalization of our findings. Furthermore, we only used a screening tool (HADS) rather than the standard psychiatric interview to define PSD. Lastly, the relationship between PSD and associated factors was only examine once (cross-sectional) instead of multiple times to determine whether the depressive symptoms would fluctuate over time.
This study has a few strengths. We used an instrument which has been reported to be the commonly used scale to assess depressive symptoms among non-psychiatric population. Our interaction with the patients was minimal in duration to avoid stressing the patients further considering clinical condition. Depression is still under-recognized and under-treated, especially in stroke patients.
References
- Rabkin JG. HIV and depression: 2008 review and update. Current Hiv/aids Reports. 2008;5:163-71.
- Fiedorowicz JG, He J, Merikangas KR. The association between mood and anxiety disorders with vascular diseases and risk factors in a nationally representative sample. Journal of psychosomatic research. 2011;70(2):145-54.
- Robinson RG. Poststroke depression: prevalence, diagnosis, treatment, and disease progression. Biological psychiatry. 2003;54(3):376-87.
- Almhdawi KA, Alazrai A, Kanaan S, Shyyab AA, Oteir AO, Mansour ZM, et al. Post-stroke depression, anxiety, and stress symptoms and their associated factors: a cross-sectional study. Neuropsychological Rehabilitation. 2021;31(7):1091-104.
- Aiyejusunle SA, Aina OF, Oladiji J, Okafor UC. Prevalence of post-stroke depression in a Nigerian sample. Nigerian Journal of Medical Rehabilitation. 2009:36-9.
- Bragança GMG, Lima SO, Pinto Neto AF, Marques LM, Melo EVd, Reis FP. Evaluation of anxiety and depression prevalence in patients with primary severe hyperhidrosis. Anais Brasileiros de Dermatologia. 2014;89:230-5.
- Narushima K, Robinson RG. The effect of early versus late antidepressant treatment on physical impairment associated with poststroke depression: is there a time-related therapeutic window? The Journal of nervous and mental disease. 2003;191(10):645-52.
- Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck depression Inventory‐II (BDI‐II), center for epidemiologic studies depression scale (CES‐D), geriatric depression scale (GDS), hospital anxiety and depression scale (HADS), and patient health Questionnaire‐9 (PHQ‐9). Arthritis care & research. 2011;63(S11):S454-S66.
- Allan LM, Rowan EN, Thomas AJ, Polvikoski TM, O'Brien JT, Kalaria RN. Long-term incidence of depression and predictors of depressive symptoms in older stroke survivors. The british journal of psychiatry. 2013;203(6):453-60.
- Marinus J, Leentjens AF, Visser M, Stiggelbout AM, van Hilten JJ. Evaluation of the hospital anxiety and depression scale in patients with Parkinson's disease. Clinical neuropharmacology. 2002;25(6):318-24.
- Oni OD, Olagunju AT, Ogunnubi PO, Aina OF, Ojini FI. Poststroke anxiety disorders in a Nigerian hospital: Prevalence, associated factors, and impacts on quality of life. Journal of Clinical Sciences. 2017;14(3):106.
- Beauchamp JES, Montiel TC, Cai C, Tallavajhula S, Hinojosa E, Okpala MN, et al. A retrospective study to identify novel factors associated with post-stroke anxiety. Journal of Stroke and Cerebrovascular Diseases. 2020;29(2):104582.
- Tang WK, Liu XX, Liang H, Chen YK, Chu WCW, Ahuja AT, et al. Location of acute infarcts and agitation and aggression in stroke. The Journal of Neuropsychiatry and Clinical Neurosciences. 2017;29(2):172-8.
- Campbell BC, De Silva DA, Macleod MR, Coutts SB, Schwamm LH, Davis SM, et al. Ischaemic stroke. Nature reviews Disease primers. 2019;5(1):70.