Adolescents in urban and rural communities in Rivers state, Nigeria: Factors influencing access and utilization of reproductive health services
Ogbonna VI1,2, Alabere ID2,3, Babatunde O2,3
Abstract
Introduction: Reproductive health services (RHS) are used and accessed differently in rural and urban areas, though to what extent is unknown. In Rivers State, Nigeria, we identified and examined the characteristics impacting adolescents' access to and use of RHS in rural and urban areas.
Methods: A cross-sectional comparative study design was employed, five hundred and seven adolescents—255 from urban and 252 from rural communities—were surveyed. Access and utilization were measured and using adjusted odd ratios in multivariate logistic regression models, predictors of access and utilization were identified.
Results: The corresponding median ages and interquartile ranges were 16.0 (14–19) and 14.0 (12–16) years, respectively. RHS utilization was low, with 57 (22.6 percent) in rural areas and 65 (25.5 percent) in urban areas. There was also a lack of access to services; only 8 (3.17 percent) rural and 81 (31.76 percent) urban residents had economic access to RHS. Access and utilization were predicted by age, level of education, awareness of RHS, sexual experience in both communities, beliefs that condoms can prevent STIs/ HIV, and exposure to mass and socio-media influenced access and utilization of RHS. Specifically, age group (15-19 years) of respondents was found to be a significant predictor of utilization of RHS for both urban (cOR=4.32, 95% CI; 0.82-22.69, p=0.001) and rural (aOR=7.65, 95% CI; 1.99-29.40, p=0.003) adolescents.
Conclusion: Adolescents in urban areas have more access (3 in 10) and utilization of RHS compared with their rural (3 in 100) counterparts. There is a need to promote information and education on RHS among adolescents, especially in rural areas.
Keywords: Access, Utilization, Reproductive Health Service, Adolescents, Rivers State.
Introduction
The World Health Organization (WHO) defines adolescents as people between the ages of 10 and 19 years, it is a period of transition from childhood to adulthood.1 Adolescents comprise 20% of the world’s population, about 1.2 billion.1,2 In sub-Saharan Africa, they make up 23% of the region’s population.3,4 This population is expected to continually increase more so in sub-Saharan Africa and Nigeria in particular where the total fertility rate (TFR) is still.3,5 The period of adolescence is characterized by physiological and psychosocial changes that put them at risk of sexual and reproductive health problems such as early marriage, teenage pregnancy, and unsafe abortion.1,6 The behavioural patterns learned throughout this period tend to last all through adult life.4,7
Reproductive health is defined as a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity, in all matters relating to the reproductive system and its functions and processes.8 Reproductive Health Services (RHS) comprise access to information and services on prevention, counselling, diagnosis, and treatment and entails that all individuals can safely reach services without travelling a long distance or wasting time to get to the service delivery points.9 According to the United Nations (UN), RHS incorporates prevention, diagnosis, and treatment as related to STIs and contraceptive service and counselling, pre-and post-natal care, delivery care, safe abortion, and post-abortion care, and access to information and education to the above issues.8,10
This means services must be available/accessible and affordable to individuals based on the principles of equity, fairness, and justice.9 Access to reproductive health care is a multidimensional concept with multiple determinants.11 Access comprises at least five components of service provision: availability, affordability, acceptability, appropriateness, and quality.11
In this study, “access” will be measured in terms of availability, looking at services available, availability of health information, and the existence of equity when receiving services by adolescents. Access will also be measured in terms of location, that is, geographical distance as well as affordability in terms of cost of services, having health insurance coverage, and use (number of young people who report receiving any of the specified SRH services in the preceding 12 months / total number of young people surveyed who report being sexually active in a defined period x 100) of RHS.12
Quality will be measured by using confidentiality and privacy in terms of service provision and adolescent involvement.
Several factors have been reported to influence access to and use of reproductive health services such as age, gender, socioeconomic status, geographical location, ethnic group, and disability.13 Others include social, environmental, cultural, and psychosocial factors and distances to health facilities.14 Many indicators of the use of reproductive health services show variations among population subgroups as well as variations according to urban/rural dwelling, ethnicity, education, and income.15 There are also variations in the availability and quality of reproductive health services.15
Rural and urban differences exist in access to and use of reproductive health services. That service is available does not mean that they are equally available to all. The extent to which existing disparities are inequitable needs to be unravelled to intervene appropriately for universal access to reproductive health care.11 Studies have been conducted on reproductive health services among adolescents in urban areas,16-19 but very few studies compared the access and use in urban and rural areas.20-22 Those done are mostly among in-school adolescents (they may have left out those not adolescents who are out of school, street, and those in the communities). We considered it necessary to determine and compare the factors influencing access and utilization of reproductive health services among adolescents in urban and rural communities in Rivers State, Nigeria.
Materials and Methods
The study was conducted in Rivers State, in South-South, Nigeria. The State is comprised of 2 urban and 21 rural Local Government Areas (LGAs). Each of the urban and rural LGAs is delineated into political wards.23 Rivers State has an estimated population of 7,303,924 million as of 2016 with a total fertility rate of 3.38.24 About 23% of the population is made up of adolescents. In sub-Saharan Africa, adolescents make up 23% of the region’s population.3
A cross-sectional comparative study design was employed. About five hundred and seven adolescents, male and female, —255 from urban and 252 from rural communities—were surveyed. This was derived by applying the formula for calculating sample size for comparative study proportions as stated by Lwanga & Lemeshow, 1991.25 In applying the formula, the first proportion inputted was the prevalence reported in a similar study on awareness and utilization of adolescent RHS in Oyo state, South-West Nigeria by Ilori et al26 among urban 15.1 % and the second proportion is 11.1% among rural adolescents.26 A non-response rate of 10% was factored in, (139/0.9 =154.4) and a design effect of 1.5, giving a sample size of each group. A multistage sampling technique was used to select participants for this study with an interviewer-administered semi-structured questionnaire adapted from the WHO illustrative questionnaire27 for interview surveys with young people used to elicit information on socio-demographic variables, and factors influencing access to and utilization of reproductive health services. Data was collected using the validated tool inputted into the Kobo toolbox and collected using Android phones. Data was then cleaned and analysed using IBM Statistical Package for Social Science (SPSS) now Statistical Product for Service Solution version 25. In measuring the overall geographic Access to Reproductive Health Services, two questions were used to assess this: If the nearest RH service delivery point from their home was greater than 5 km, and if it takes greater than 30 minutes to the nearest RH service delivery point from your home. Participants who answered “No” to either of these questions were said to have geographic access.
In measuring the overall Economic Access to Reproductive Health Services, three questions were used to assess this: How well can you afford the cost? Have health insurance? and how well were you able to afford the cost of treatment. Participants who answered “Always” or “Usually” in the first and third questions and “Yes” in the second question are said to have economic access. Chi-square (χ2) test was performed to test for association between the explanatory variables and the outcome variables. It used the chi-square test of independence for the difference in proportion between groups (chi-square test for goodness of fit). Socio-demographic and economic factors influencing access and utilization were determined using the chi-square test of independence, and logistic regression models for rural and urban settings separately.
The variables that were significant at the level of Chi-square (χ2) test analysis was used for the bivariate analysis. Multivariate Logistic Regression analyses were done where applicable to adjust for the effect of confounding variables, only those variables that were significant at the bivariate level analysis were input into the multivariate analysis. A variable was said to be statistically significant if the p-value is less than or equal to 0.05 (≤0.05) at a 95% confidence interval. Access and utilization were measured and using adjusted odd ratios in multivariate logistic regression models, predictors of access and utilization were identified.
Ethical approval was sought and obtained from the Research and Ethics Committee of the University of Port Harcourt Teaching Hospital with ethical approval number UPTH/ADM/90/S. 11/VOLXI/1226.
Informed consent (Consent for participants 18 years and above, assent for those less than 18 years as well as consent from their parents/guardian) was sought and obtained from participants and caregivers who signed assent/consent forms before the survey to ensure their willingness to participate in the study, and they were told that they have a right to refuse to participate or to withdraw at any time.
Results
Table 1a: Socio-demographic profile of respondents
As shown in Table 1a, the median age and interquartile range (IQR) for urban was 16.0 (14-19) whereas, the rural was 14.0 (12-16), this difference was statistically significant as depicted by the Mann-Whitney test. The median was used because the normality test showed that the data set was not normally distributed with a Shapiro-Wilk test of 0.001 significance. In addition, the other variables that showed significant association were level of education completed, currently attending school, occupation, marital status, and residing with other relatives, at p≤ 0.05.
Table 1b: Socio-demographic (socioeconomic) profile of respondents (2)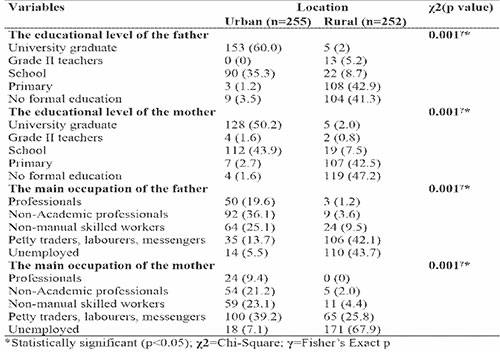
Table 1b shows the socio-demographic (economic) profile of the respondents. As shown, for the educational level of fathers, 60% of the respondents in urban have their fathers as university graduates whereas among rural respondents it was 2%. In addition, 50.2 % of the respondents in urban have their mothers as university graduates whereas, among rural respondents, it was 2%. Fathers with no formal education in urban were 3.5% whereas in rural it was 41.3% in addition, mothers with no formal education am urban respondents were 1.65 whereas; in rural, it was 47.2%. These differences in proportion in the educational level of parents among rural and urban respondents were statistically significant as depicted by Fisher’s Exact.
For the main occupation of father, 36.1% of the respondents in urban have their fathers as non-academic professionals whereas among rural respondents it was 3.6%. In addition, 21.2 % of the respondents in urban have their mothers as non-academic professionals whereas, among rural respondents, it was 2%.
Fathers that were unemployed in urban was 5.5% whereas in rural it was 43.7%. In addition, mothers were unemployed among urban respondents was 7.1% whereas; in rural, it was 67.9%. These differences in proportion in occupation of parents among rural and urban respondents were statistically significant as depicted by Fisher’s exact test.
Utilization of reproductive health services among adolescents in urban and rural communities in Rivers State
Table 2: Utilization of Reproductive Health Services among adolescents in urban and rural communities in Rivers State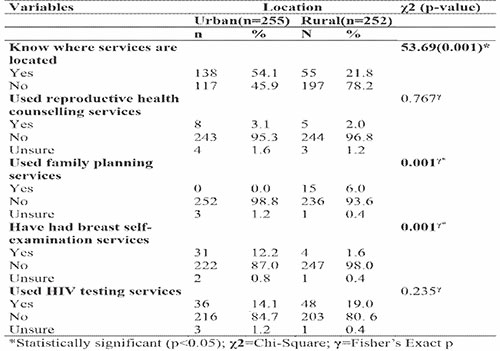
Table 2 shows the utilization of reproductive health services among male and female adolescents in urban and rural communities in Rivers State. As shown, 54.1% of urban versus 21.8% of rural respondents know where the services are located, this difference in proportion is statistically significant at p≤0.05. Utilization of reproductive health services, in general, was 65 (25.5 %) in urban versus 57 (22.6%) in rural, the difference in proportion was not statistically significant though utilization was higher in urban than rural. The utilization of family planning services at 0% in urban versus 5.9 % in rural was statistically significant. Breast self-examination services had a statistically significant difference in proportion between urban 12.2% and rural 1.6% respondents. Other services like the use of reproductive health counselling, post-abortion care services (them or their partners), and HIV testing services did not show a statistically significant difference in proportion between urban and rural respondents. The study shows that none of the respondents in urban and rural communities has ever been vaccinated with the HPV vaccine against cervical cancer.
Access to reproductive health services among adolescents in urban and rural communities in Rivers State
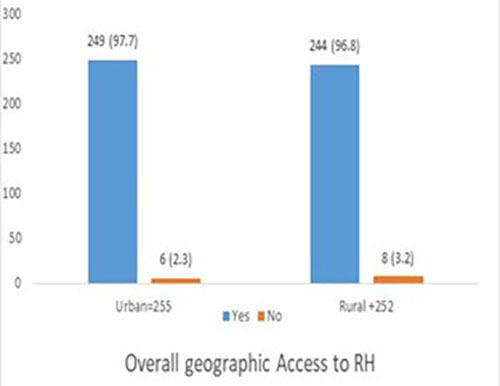
Figure 1: Overall geographic Access to Reproductive Health Services
Figure 1 shows overall geographic access to reproductive health services. As shown, 97.7% of urban versus 96.8% of rural have access (availability/geographic) to reproductive health services. Overall geographic Access to RHS was proportionally higher for the urban compared to rural (249; 97.7% versus. 244; 96.8%), and these findings were not statistically significant χ2= 0.09; p =0.769.
Table 3: Overall Affordability (Economic) Access to Reproductive Health Service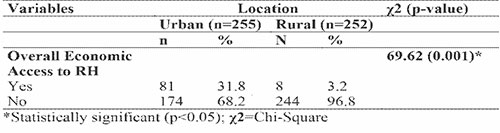
Table 3 shows overall economic access to reproductive health services. As shown, 31.8% of urban versus 3.2% of rural have access (economic) to reproductive health services. The Overall economic access to RHS was proportionally higher for the urban than the rural (81, 31.8% versus. 8, 3.2%), and this finding was statistically significant (p=0.001).
Factors associated with/ predictors of utilization of RHS in urban and rural communities
The study assessed the sociodemographic, awareness, Individual, family, and community factors associated with utilization in urban and rural communities.
Table 4: Bivariate and Multivariate analysis between associated factors and Utilization among urban respondents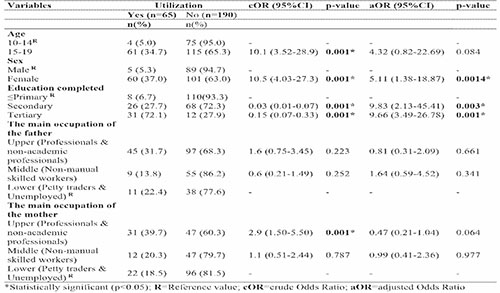
Table 4 shows the bivariate and multivariate analysis between associated factors and utilization among urban respondents. As shown, in the bivariate analysis, the age, sex, level of education, and occupation of the father and mother were significantly associated with the utilization of RHS among adolescents in urban communities. However, in the multivariate analysis, only sex, level of education completed, and father’s occupation were shown to be statistically significant.
The study shows higher odds of utilizing Reproductive Health Services among adolescents aged 15-19 (cOR=4.32, 95% CI; 0.82-22.69, p=0.001) compared to those younger (10-14). Those aged 15-19 were 4.32 times more likely to utilize services compared to those 10-14 after adjusting for confounders.
The study shows a higher odd (there is a 9-fold increase in utilization) of utilizing Reproductive Health Services among adolescents having secondary and tertiary education (aOR=9.83, 95% CI; 2.13-45.41, p=0.003), (aOR=9.66, 95% CI; 3.49-26.78, p=0.001) compared to those with primary education or no formal education.
Table 5: Bivariate and Multivariate analysis between associated factors and Utilization in rural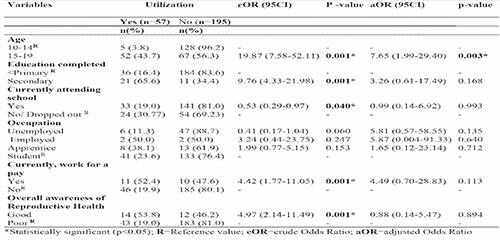
Table 5 shows the bivariate and multivariate analysis between associated factors and utilization among rural respondents. As shown, in the bivariate analysis, age, level of education, currently attending school, currently working for pay and overall awareness of reproductive health were the factors that were significantly associated with the utilization of RHS among adolescents in rural communities. However, in the multivariate analysis, only age was shown to be statistically significant. The study shows higher odds of utilizing Reproductive Health Services among adolescents aged 15-19 (aOR=7.65, 95% CI; 1.99-29.40, p=0.003) compared to those younger (10-14). Those aged 15-19 were 7.7 times more likely to utilize services compared to those 10-14 years.
Table 6: Bivariate and Multivariate analysis between associated factors and Utilization in rural (2)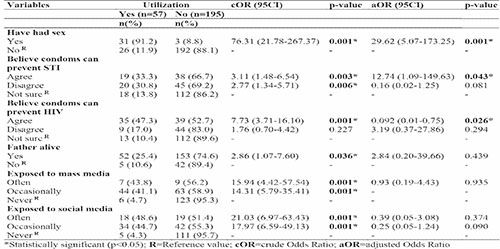
Table 6 shows a continuation of individual, family and community factors associated with utilization in urban and rural communities. As shown, in the bivariate analysis, sexual experience, belief that condoms can prevent STI, belief condoms can prevent HIV, father alive, exposed to mass and social media were all significantly associated with the utilization of RHS among adolescents in rural communities. However, in the multivariate analysis, sexual experience, belief that condoms can prevent STIs, and belief that condoms can prevent HIV were the factors that were shown to be statistically significant.
The study shows higher odds of utilizing Reproductive Health Services among adolescents who had had sex (aOR=29.62, 95% CI; 5.07-173.25, p=0.001) compared to those who did not. Also, there are higher odds of utilizing Reproductive Health Services among adolescents who believe (agreed) condoms can prevent STIs (aOR=12.74, 95% CI;1.09-149.63, p=0.043) compared to those who did not (disagreed).
However, it showed lower odds of utilizing Reproductive Health Services among adolescents who believe (agreed) condoms can prevent HIV (aOR=0.092, 95% CI;0.01-0.75, p=0.043) compared to those who did not (disagreed).
Those who have had sex were 29.6 times more likely to utilize RHS among the respondents in rural communities. In addition, those who agreed that condoms can prevent STIs were 12.7 times more likely to utilize RHS among the respondents in rural communities.
Factors associated with/ predictors of access to reproductive health services in urban and rural communities
Table 7: Bivariate and Multivariate analysis between associated factors and Access (Availability) in urban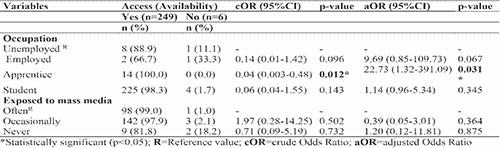
Table 7 shows the bivariate and multivariate analysis between associated factors and Access (Availability) in urban communities. As shown, only occupation was significantly associated with access (availability) after adjusting for co-founders. The study shows a higher odd of access to Reproductive Health Services among adolescents who were apprentices (aOR=22.73, 95% CI; 1.32-391.09, p=0.031) compared to those who were unemployed. Those who were apprentices were 22.7 times more likely to have access (availability) than unemployed, employed and students after adjusting for cofounders.
Table 8: Bivariate and Multivariate analysis between associated factors and Access (Availability) in rural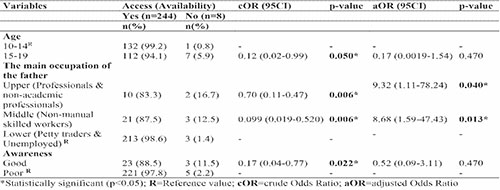
Table 8 shows the bivariate and multivariate analysis between associated factors and Access (Availability) in rural communities. As shown in the bivariate analysis, age, occupation of the father, and awareness were significantly associated with access (availability). However, in the multivariate analysis, only the occupation of the father was significantly associated after adjusting for co-founders. There is a higher odd to access (availability) Reproductive Health Services among adolescents whose fathers belong to the Upper (professionals & non-academic professionals) and middle (non-manual skilled workers) (aOR=9.32, 95% CI; 1.11-78.24, p=0.04), (aOR=8.68, 95% CI; 1.59-47.43, p=0.013) compared to those Lower (petty traders and unemployed).
Table 9: Bivariate and Multivariate analysis between associated factors and Access (Affordability) in rural communities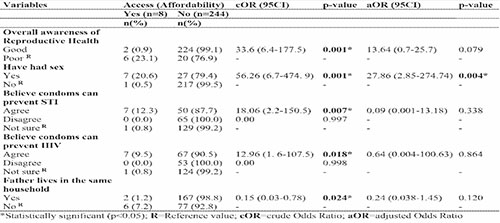
Table 9 shows the bivariate and multivariate analysis between other associated factors and Access (affordability) in rural communities. As shown, in the bivariate analysis, overall awareness, sexual exposure, belief that condoms can prevent STIs, belief condoms can prevent HIV, and fathers living in the same household were all significantly associated with access (affordability) among adolescents in rural communities. However, in the multivariate analysis, only those who had had sex had more access 7 (20.6%), than those who had not 1 (0.5%) these factors were shown to be statistically significant (aOR=27.86, 95% CI; 2.85-274.74, p=0.004) compared to those who have not had sexual experience.
Discussion
The study determined and compared the utilization of and access to reproductive health services among adolescents in urban and rural communities in Rivers State, Nigeria. It also determined the associated factors influencing the utilization of and access to reproductive health services among adolescents in urban and rural communities in Rivers State. The socio-demographic and economic profiles of the respondents varied significantly across geographic locations (urban versus rural). The utilization of reproductive health services among adolescents was higher in urban compared to rural communities, the difference in proportion is however not statistically significant. The utilization is demonstrated to be less than average, and it is unsatisfactory. In this study, the services that showed significant associations were family planning services and breast self-examination services. None of the respondents in urban and rural communities has ever been vaccinated with the HPV vaccine against cervical cancer, though there was a significant difference in awareness of HPV.
The findings were in tandem with a similar study in South-West Nigeria by Ilori et al,26 among rural and urban adolescents, which reported much lower utilization levels, of rural than urban respondents who ever utilized adolescent reproductive health services, the difference between the utilization in both groups was also not statistically significant.26 It is similar because utilization is higher in urban than in rural, and the difference is not statistically significant. It also differs from this study because only about one-tenth utilized RHS. This contrasts with a similar study in Ethiopia that reported a significant difference in SRH service utilization between urban (56.9%) and rural (30.8%) participants.22
Also, in this study, the utilization of family planning methods was shown only among rural adolescent respondents while breast self-examination services utilization was higher in urban than rural. It is in contrast with a study in Ghana that reported a much higher utilization of contraceptive/family planning methods 30.76%, and for breast examination, 2(2.19%).28 This may be because of the perception/misconceptions surrounding Adolescent reproductive health services in Nigeria as young people are not expected to openly express their sexual and reproductive health needs.
Studies that were done in Ghana, Ethiopia, and China reported similar results (low utilization) of reproductive health services among adolescents.18,19,28 In contrast with this study, a similar study in California reported that the use of family planning services was lower among rural than urban participants.29 This may be because adolescents in rural areas are likely to have more need for family planning services compared to those in urban areas. Therefore, the call for shifting the narrative and encouraging adolescent utilization of reproductive health services and strategically involving key players in communities, schools, and policy arena. To ensure that key attention is paid to adolescents, especially in rural communities.
Overall geographic Access to RHS was proportionally higher for the urban compared to rural, and these findings were not statistically significant. Overall economic (affordability) access to RHS was proportionally higher for the urban than the rural), and this finding was statistically significant. Although availability/geographic access was high, affordability/economic access was low. These differences in access to reproductive health services can put adolescents in rural areas at greater risk of unintended pregnancy.
The findings from this study on high availability and low economic access corroborate with some studies done in other parts of the country. A qualitative study conducted in Kaduna, Nigeria reported that access to RHS was low.30 Another study in Enugu Nigeria reported high geographic access but low financial access 58.4 and 50.5% respectively among respondents.16 This is also in tandem with a similar study in Nigeria which reported that 53.9% of the urban respondents and 35.1% of the rural respondents had geographic access.31 They agreed that the distance between their house and the places of procurement of contraceptives was about a walking distance. Although geographic access is lower than what was found in this study, it was higher in urban than in rural. These findings also corroborate a similar study in Myanmar which reported geographical accessibility was high (79.3%), and financial accessibility was low (19.1%) resulting in low overall accessibility (34.5%) to RH services.32
Several factors were shown to influence the utilization of and access to RHS among adolescents in urban and rural communities in this study. The level of education completed was predictive of the utilization of RHS in both urban and rural communities.
Of the sexually active respondents, about three-fifths are urban respondents and two-fifths are rural respondents. This is similar to a study done among rural and urban unmarried in-school Adolescents in Osun State, Nigeria where almost three-fifths of the urban respondents and more than two-fifths of the rural respondents were sexually active.31 In addition, those who agreed that condoms can prevent STIs were 12.7 times more likely to utilize RHS among the respondents in rural communities.
These findings on factors influencing utilization also corroborate with some Nigerian studies16,31,33 done in Osun State Nigeria which reported that age and sex were significant predictors of utilization of contraceptives for urban and rural adolescents,31 and Ogun State Nigeria, which reported a significant gender difference in utilization of reproductive health services among undergraduates.33 Also, Odo et al16 in Enugu State Nigeria reported that gender, age, education, income, and living status were predictors of utilisation of RHS.16 These findings are also in tandem with similar studies in Ethiopia,1,19,22 which showed that factors associated with the utilization of sexual and reproductive health services were age from 15 to 19 years (AOR=0.36; 95% CI: 0.17, 0.76),19 and Kenya.34 Therefore, intervention to target improvement in access to and utilization of reproductive health services among adolescents needs to be age and gender appropriate.
Conclusion
In conclusion, this study revealed that utilization of RHS among adolescents was low, especially among those in rural communities. About one in four adolescents in urban communities utilize RHS whereas in rural it was about one in five. Therefore, utilization of RHS among adolescents in rural and urban communities is low especially in rural communities.
Access to RHS is mostly available at 97% and 96% in both urban and rural communities respectively. Access in terms of affordability (economic), only about 3 in 10 adolescents in urban communities have economic access to RHS, this is worse among adolescents in rural where only about 3 in 100 have access (economic/affordability) to RHS.
Recommendation
Access and utilisation of reproductive health services is very low across rural and urban regions however, it is remarkably lower in the rural areas. To bridge this gap, governments in Rivers State and elsewhere and stakeholders must begin to redirect our efforts to target rural areas in an attempt to improve access to information on RHS among the rural and urban adolescent populace, to improve utilization and access to RHS. By ensuring that adolescents especially in rural areas have access to quality education in the Spirit of equity and fairness.
References
1. Abajobir AA, Seme A. Reproductive health knowledge and services utilization among rural adolescents in east Gojjam zone, Ethiopia: A community-based cross-sectional study. BMC Health Serv Res. 2014;14(1):1–11.
2. Williams K, Sassier S, Addo F, Frech A. First-birth timing, marital history, and women’s health at midlife. J Health Soc Beha. 2018;56(4):514–33.
3. Lehtimaki S, Schwalbe N. Adolescent Health. The missing population in Universal Health Coverage. 2019.
4. Ezenwaka U, Mbachu C, Okeke C, Agu I, Ezumah N, Onwujekwe O. Socio-demographic and economic determinants of awareness and use of contraceptives among adolescents in Ebonyi State , South-east , Nigeria. Afr J Reprod Health. 2021;25(June):21–9.
5. Adebowale AS, Fagbamigbe AF, Adebayo AM. Regional differences in Adolescent childbearing in Nigeria. Journal of Population and Social Studies. 2016;24(2):101–16.
6. Kyilleh JM, Tabong PT nefaah, Konlaan BB. Adolescents ’ reproductive health knowledge, choices and factors affecting reproductive health choices : a qualitative study in the West Gonja District in Northern Region, Ghana. BMC Int Health Hum Rights. 2018;18(6):1–12.
7. Dehne KL, Riedner G. Sexually transmitted infections among adolescents: The need for adequate health services. Reprod Health Matters. 2001;9(17):170–83.
8. United Nations Department of Economic and Social Affiairs Population Division. Reproductive health policies 2017. Data Booklet. 2016. p. 9–13.
9. Tlaye KG, Belete MA, Demelew TM, Getu MA. Reproductive health services utilization and its associated factors among adolescents in Debre Berhan town , Central Ethiopia : a community-based cross-sectional study. Reprod Health. 2018;15(217):1–11.
10. United Nations. Report of the International Conference on Population and Development Cairo, 5-13 September 1994. 1995. 5–13 p.
11. WHO, UNFPA. Measuring access to reproductive health services: Report of a WHO/UNFPA technical consultation 2-3 December 2003. health services: Report of a WHO/ …. 2004.
12. Measure Evaluation. Use of specified sexual and reproductive health services by young people — MEASURE Evaluation [Internet]. [cited 2021 Jun 21]. Available from: https://www.measureevaluation.org/rbf/indicator-collections/service-use-and-coverage-indicators/use-of-specified-rh-health-services-by-young.html
13. National Academies of Sciences, Engineering and Medicine. Health-Care Utilization as a Proxy in Disability Determination. Health-Care Utilization as a Proxy in Disability Determination. Washington, DC: The National Academies Press; 2018. 1–160 p.
14. Sialubanje C, Massar K, Hamer DH, Ruiter RAC. Understanding the psychosocial and environmental factors and barriers affecting utilization of maternal healthcare services in Kalomo, Zambia: A qualitative study. Health Educ Res. 2014;29(3):521–32.
15. Worku F, Gebresilassie S. Reproductive health for health science students. University of Gondar. Ethiopia; 2008. 1–416 p.
16. Odo AN, Samuel ES, Nwagu EN, Nnamani PO, Atama CS. Sexual and reproductive health services ( SRHS ) for adolescents in Enugu state , Nigeria : a mixed methods approach. BMC Health Serv Res. 2018;18(92):1–12.
17. Ojoniyi OO, Ogujiuba K, Stiegler N. Susceptibility of Nigerian adolescents to pregnancy and use of modern contraceptives. Afr J Reprod Health. 2022;26(2):106–17.
18. Lim MSC, Zhang XD, Kennedy E, Li Y, Yang Y, Li L, et al. Sexual and reproductive health knowledge, contraception uptake, and factors associated with unmet need for modern contraception among adolescent female sex workers in China. PLoS One. 2015;10(1):1–17.
19. Tilahun T, Bekuma TT, Getachew M, Seme A. Assessment of access and utilization of adolescent and youth sexual and reproductive health services in western Ethiopia. Reprod Health. 2021;18(1):1–9.
20. Seifu A, Fantahun M, Worku A. Reproductive health needs of out-of-school adolescents: A cross-sectional comparative study of rural and urban areas in northwest Ethiopia. EthiopJHealth Dev. 2006;20(1):13–17.
21. Ilori O, Awodutire P, Ilori O. Awareness and utilization of adolescent reproductive health services among in-school adolescents in urban and rural communities in Oyo state. Nigerian Medical Journal. 2020;61(2):67.
22. Habte A, Dessu S, Bogale B, Lemma L. Disparities in sexual and reproductive health services utilization among urban and rural adolescents in southern Ethiopia, 2020: a comparative cross-sectional study. BMC Public Health. 2022;22(1):1–7.
23. Tella AO, Tobin-west CI, Babatunde S. Pattern, Consequences and Medical Cost of Domestic Violence Among Pregnant Women In Rural And Urban Areas of Rivers State, Nigeria. The Nigerian Journal of Public Health. 2017;2(2):151–61.
24. National Bureau of Statistics. Demographic statistics bulletin. 2018. p. 1–25.
25. Lachenbruch PA, Lwanga SK, Lemeshow S. Sample Size Determination in Health Studies: A Practical Manual. J Am Stat Assoc. 1991;86(416):1149.
26. Ilori O, Awodutire P, Ilori O. Awareness and utilization of adolescent reproductive health services among in-school adolescents in urban and rural communities in Oyo state. Nigerian Medical Journal. 2020;61(2):67.
27. Cleland J. Illustrative questionnaire for interview-surveys with young people. Asking Young People About Sexual and Reproductive Behaviors. Illustrative Core Instruments, Geneva: World Health Organization. Geneva: World Health Organization. 2001;3–5.
28. Amissah C. Factors Influencing Accessibility and Utilization of Reproductive Health Services Among Adolescent in Ga East Municipality. 2019. p. 5–9.
29. Yarger J, Decker MJ, Campa MI, Brindis CD. Rural–Urban Differences in Awareness and Use of Family Planning Services Among Adolescent Women in California. Journal of Adolescent Health. 2017;60(4):395–401.
30. Nmadu AG. Access and utilization of reproductive health services among in Kaduna North Local Government, Nigeria. University of the Western Cape; 2017.
31. Israel OK, Adeomi AA, Adeoye OA, Isreal MG, Olugbenga-Bello AI. Contraceptive Knowledge, Access and Uptake among Rural and Urban Unmarried in-school Adolescents in Osun State, Nigeria: A Comparative Study. J Community Med Public Health. 2019;3(3):1–12.
32. Thin Zaw PP, Liabsuetrakul T, Htay TT, McNeil E. Equity of access to reproductive health services among youths in resource-limited suburban communities of Mandalay City, Myanmar. BMC Health Serv Res. 2012;12(1):1–12.
33. Adebisi G, Olanrewaju K. Factors Influencing Access and Utilization of Reproductive Health Services among Undergraduates in Selected Tertiary Institutions in Ogun State, Nigeria. Int J Health Sci (Qassim). 2019;7(2):2372–9.
34. Kibani OK. Factors influencing utilization of reproductive health servicesamongst young people in Rift Valley Provincial Hospital, Nakuru County- Kenya. Plan of Action. 2015;24(14):542–6.