Prevalence and determinants of depression among patients attending adult HIV clinic of University of Uyo Teaching Hospital, Uyo, Southern Nigeria
Okeke DO1, Udoh SB2, Jiman AC3, John E4
Abstract
Background: Mental health challenges particularly depression is common among people living with HIV/AIDS and has been largely neglected. This is of great concern because depression is associated with high morbidity among its sufferers. An assessment of depression among PLWHA and its predictors will enhance their quality of life and improve their health outcomes.
Aim: To determine the prevalence and determinants of depression among patients attending the adult HIV clinic in University of Uyo Teaching Hospital, Uyo, Nigeria.
Method: This was a cross-sectional descriptive study conducted at the adult HIV outpatient clinic of University of Uyo Teaching Hospital Uyo. A total of three hundred and fifty one eligible respondents were recruited over three months. Their levels of perceived social support, depression, HIV stigma and substance abuse were assessed using the Multidimensional Scale of Perceived Social Support (MSPSS), Patient Health Questionnaire 9 (PHQ 9), Internalized AIDS-related Stigma Scale and CAGE questionnaire respectively.
Results: The mean age of the respondents was 39.8 ± 10.7 years. Two hundred and sixty six (75.8%) of the respondents were females, while eighty five (24.2%) were males. The overall prevalence of depression was 10%. Majority of respondents had disclosed their status and were experiencing HIV stigmatization representing 84.6% and 95.4% respectively. Most of the respondents (65.8%) had low perceived social support. Depression was found to be statistically associated with unskilled workers (χ2 = 13.08, p = 0.008), unmarried respondents (χ2 = 8.45, p = 0.03), low perceived social support (χ2 = 7.76, p = 0.02), shorter duration of ART use (χ2 = 8.41, p = 0.04), adverse life events (χ2 = 4.05, p = 0.04) and increasing levels of HIV stigma (χ2 = 7.66, p = 0.02) among the study participants.
Conclusion: The findings of this study showed that the prevalence of depression in PLWHA was high. Therefore, the screening and prompt treatment of depression in HIV positive persons should be inculcated into their management plan. Furthermore, policies should be made to minimize discrimination and stigmatization of PLWHA in the communities and healthcare systems. Finally, the relevant stakeholders should work in unison to improve the social welfare conditions of HIV infected persons.
Keywords: HIV/AIDS, depression, stigma, social support, mental health, Nigeria
Introduction
According to estimates by WHO and UNAIDS, 36.7 million people were living with HIV globally with 1.8 million newly infected persons, and 1 million deaths secondary to HIV-related causes.1 Depression and other mental health disorders are common among HIV infected persons with almost half of the HIV patients having at least one mental health disorder.2,3 Persons infected with HIV are more likely to suffer from depression and anxiety disorder compared to the general population.4 In a study done by Chikezie and his colleagues in Benin city, they found that HIV patients were five times more likely to develop depression when compared to the general population with a prevalence of 29.3% to 7.3% respectively.5 Also, depression is the most prevalent mental health disorder seen in persons with HIV.6 There is a two-way bi-directional relationship between HIV and depression. People living with HIV may experience stigma or possess a negative self-image which predisposes them to depression and they are more likely to belong to the demographic class associated with various social stressors such as financial insecurity and poor housing, thus further putting them at risk for depression.7,8 Also studies have implicated HIV in the development of depression by directly altering the neurotransmitter pathway in HIV patients.9 On the other hand, people who suffer from depression and some other mental problems are more likely to engage in risky sexual behaviours predisposing them to HIV infection.10
In a multi-centered study done in the United States involving 4,217 participants, the prevalence of depression among HIV patients was found to be 25.6% using the PHQ-8 questionnaire. This figure was three times higher than the depression in a control group comprising of people without HIV.11 In Africa, Besa, Paul and Hachaambwa in a study involving 185 patients attending HIV clinic in Zambia reported a prevalence of 7% using the Mini International Neuropsychiatric Interview (MINI).12 A study done in Botswana by Kathy Lawler et al showed a prevalence of 24%.13 In a hospital-based study done by Nel and Kagee in South Africa, they reported a prevalence of 11.7% among PLWHA.14 Similarly, Wroe and his colleagues also reported a prevalence of 11.2% among patients attending HIV clinics in three health centers in Rwanda.15
In Nigeria, several studies have highlighted the increased likelihood of HIV patients to develop depression and other mental health challenges. Shittu and his team in a hospital-based study in Ilorin reported a depression prevalence rate of 56.7% among patients attending the HIV clinic.16 Medsker et al in Ibadan Oyo State, South-West Nigeria reported an overall prevalence of 6.5% among patients attending the AIDS Prevention in Nigeria (APIN) clinic, University College Hospital.17
Although the etiology of depression in HIV infected persons is not entirely clear, some authors have highlighted some characteristics and conditions that may be associated with the development of depression among PLWHA. The evidence of risk factors for depression came primarily from observational studies and are crudely grouped into biological, psychological and social risk factors. Biological factors include the female gender, age, presence of other chronic medical illness, use of certain medications, substance abuse, HIV clinical stage, HIV viral load and CD4 count.13,18–22 The psychological factors are HIV associated stigmatization and HIV disclosure status while the social factors include low socioeconomic status, being unmarried, stressful life events and low social support.12,16,23,24 The aim of this study was to determine the prevalence and determinants of depression among patients attending the adult HIV clinic of University of Uyo Teaching Hospital, Uyo, southern Nigeria.
Methods
Study Site: The study was a hospital based cross-sectional descriptive study on adult HIV patients attending the adult HIV clinic of UUTH for three months. University of Uyo Teaching Hospital (UUTH) is a tertiary hospital in Akwa-Ibom State. The adult HIV clinic of UUTH is run by the hospital management and other international collaborators and offers counselling, drug treatment and laboratory services to HIV patients.
Sample Size Determination: The sample size was determined using the Leslie and Kish statistical formula for determining sample size for cross sectional studies, n=Z2pq/d2 by substituting p of 29.3% being the prevalence of depression among HIV patients in a study done in Benin city, southern Nigeria and a non-response rate of 10% to obtain a sample size of 351. A systematic sampling method with a sampling interval of 15 was used to select participants for this study.
Selection Criteria: HIV positive patients aged 18 years and above attending the adult HIV clinic of UUTH were included into the study. Also respondents must have had the HIV infection and commenced antiretroviral medication for at least six months. Patients that were acutely ill, pregnant or had frank psychosis were excluded from the study.
Study protocol: Pretested questionnaires were administered to eligible respondent attending the adult HIV clinic. The questionnaire comprised of 3 sections. The first section was used to collect socio-demographic data of the respondents while the second section assessed the respondents HIV related medical history such as duration on antiretroviral drugs, disclosure status, presence of other chronic illness, recent adverse life event, HIV stigma, substance abuse screening and perceived social support. PHQ-9 was used to screen for depression. The final section was used to evaluate relevant HIV-related parameters such as the level of cluster of differentiation 4 (CD4) cell count, HIV viral load, HIV clinical stage and the antiretroviral medications the respondent was using.
The PHQ 9 is a standardized questionnaire used to both screen and rate the severity of depression in primary care developed by Robert Spitzer and his colleagues from Columbia University in 2002.25 It is a 9-item questionnaire configured based on the DSM IV diagnostic criteria for depression. Each of the 9 items is scored on a four-point Likert scale (0-3) and the total score is summed up (0-27). Respondents with a score of 10 and above were considered as having depression. The severity of depression was graded as none (0-4), mild (5-9), moderate (10-14), moderately severe (15-19), and severe (20-27).25
The CAGE questionnaire is an easy-to-use tool to screen for alcohol dependency.26 Although initially designed to screen for alcohol dependency, the questionnaire has been adapted to screen for other forms of substance abuse.26 It consists of four questions and each question is scored 1 for ‘yes’ and 0 for ‘no’.27 The higher the score the greater the indication of alcohol problems.27 A total score of two or greater was considered clinically significant.27
The Internalized AIDS-related Stigma Scale was used to assess the level of stigma in HIV infected persons.28 It is a six item questionnaire with each item scored on a one-point binary scale (Agree, Disagree).28 The total score is summated with a possible score of 0 – 6 with a score of 0 categorized as no stigma, 1 – 3 as low stigma and 4 – 6 as high stigma.28
The level of perceived social support of the participants was assessed using the MSPSS.29 It is a 12 item questionnaire where each item is scored on a 7-point likert scale. The mean total is obtained by the summation of the total score and dividing them by 12. A total score of 1 – 2.9 represents low support, 3 – 5 moderate support and 5.1 – 7 for high support.29
Data Analysis: Data collected was collated, coded and imputed into the statistical package for social sciences (SPSS) version 22. Frequencies and percentages were used to represent categorical variables. Associations between depression and the other categorical variables were evaluated with Pearson’s Chi-square test (χ2). The level of significance was set at P value < 0.05 at 95% confidence level.
An informed consent was obtained from respondents while ethical approval from University of Uyo Teaching Hospital Research and Ethical Committee was obtained before the commencement of the study. Confidentiality was maintained throughout the conduct of the study.
Results
Socio-demographic characteristics of the respondents
The socio-demographic characteristics of the respondents are shown in table 1. The mean age of the respondents was 39.8 (± 10.7) years. Two hundred and sixty six (75.8%) of the respondents were females, while eighty five (24.2%) were males. Majority (49.6%) of the study participants were married. About 50% of the respondents attained secondary level of education while only 10 (2.9%) had no formal education. Majority (44.7%) respondents were traders.
Table 1: Sociodemographic characteristics of the respondents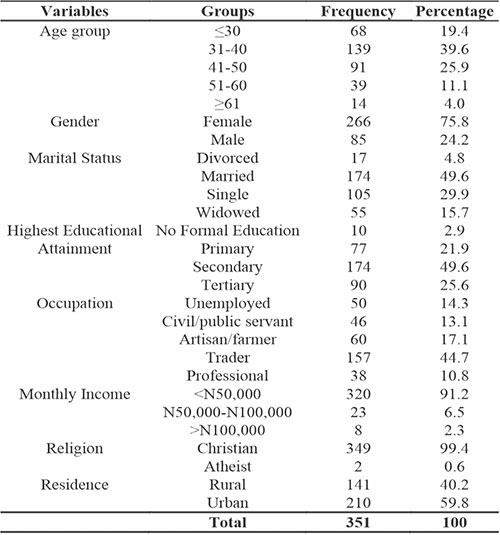
Table 2 shows the clinical characteristic of the respondents. All the respondents had commenced HIV medications. The average length on antiretroviral medication was one year and one month. One hundred and six (30.2%) had been on HIV medications for 3 years or less, eighty five (24.2%) for 4 -7 years, eighty (22.8%) for 8 – 10 years and eighty (22.8%) for more than 10 years.
Table 2: The HIV clinical characteristics of the respondents
One hundred and fifty seven (44.7%) had achieved HIV viral suppression (viral load <40), while one hundred and ninety four (55.3%) had not achieved viral suppression. Sixty five (18.5%) respondents had CD4 count <200, one hundred and fifty five (44.2%) had between 200 – 499 and one hundred and thirty one (37.3%) had above 499. Most of the respondents (98.9%) fell under HIV clinical stage one, while three (0.8%) were stage two and only one respondent was stage three (0.3%). No person with HIV clinical stage four was recruited in this study.
Majority of the respondents two hundred and ninety seven (84.6%) had disclosed their HIV status to someone. Only seventy five respondents (21.4%) were on efavirenz-containing antiretroviral medications. Forty nine (13.9%) had other chronic medical illness.
A little above half of the participants 177 (50.4%) had experienced a major adverse life event within two months of the study such as bereavement, job loss or relationship breaks. One participant (0.3%) had a score of 2 and above on the CAGE questionnaire for alcohol and substance abuse while three hundred and fifty (99.7%) respondents did not have a substance abuse problem.
Majority of the respondents three hundred and thirty five (95.4%) perceived some form of HIV stigmatization, while the remaining sixteen (4.6%) had none. Two hundred and thirty one (65.8%) of the respondents had low social support, ninety four (26.8%) had moderate social support, while only twenty six (7.4%) had high social support.
Table 3: Distribution of depression among the respondents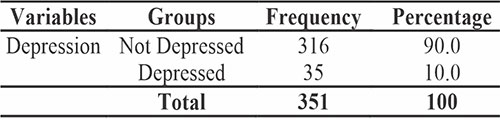
Table 3 shows the prevalence of depression among the study participants. Of the three hundred and fifty one respondents recruited for this study, thirty five (10%) had depression while three hundred and sixteen (90%) were not depressed. Assessing the pattern of severity, two hundred and forty three (69.2%) had no depressive symptoms, seventy three (20.8%) mild depressive symptoms, twenty five (7.1%) had moderate depressive symptoms, eight (2.3%) had moderately severe and two (0.6%) had severe depressive symptoms. This is illustrated in figure 1.
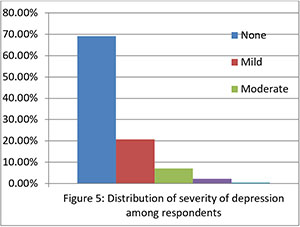
Figure 1: Pattern of severity of depression among respondents
Table 4: Relationship between sociodemographics and depression among respondents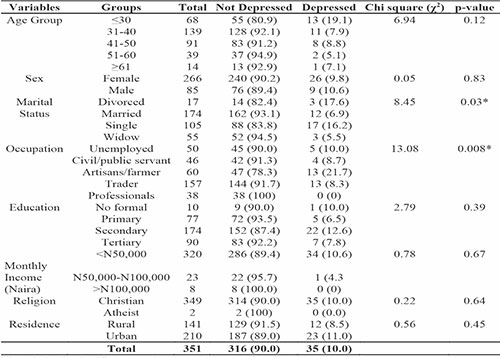
On bivariate analysis (table 4), there was a statistically significant relationship between marital status and depression (χ2 = 8.45, p = 0.03). The divorced (17.6%) and single (16.2%) respondents were more likely to be depressed compared to the married (6.9%) respondents. There was also a statistically significant association between the respondent’s occupation and depression (χ2 = 13.08, p = 0.008). Depression was more prevalent among the artisans/farmers (21.7%) and unemployed (10.0%) but least prevalent among the professionals (0%).
There was a statistically significant association between the duration of HIV medication (HAART) and depression (χ2 = 8.41, p = 0.04). Depression was more prevalent among respondents that have used anti-HIV medications for a short duration (6 months - 3 years). Additionally, there was a statistically significant relationship between recent major adverse life events and depression (χ2 = 4.05, p = 0.04). Depression was more prevalent among respondents that had no history of recent major adverse life events than those that did.
HIV stigma was found to be significantly associated with depression in this study (χ2 = 7.66, p = 0.02). Respondents with higher perceived HIV stigma levels were found to be more depressed compared to those with lower stigma levels.
The study found a statistically significant relationship between depression and perceived social support (χ2= 7.76, p = 0.02). The prevalence of depression was highest in patients with low support.
Table 5: Relationship between HIV clinical characteristics and Depression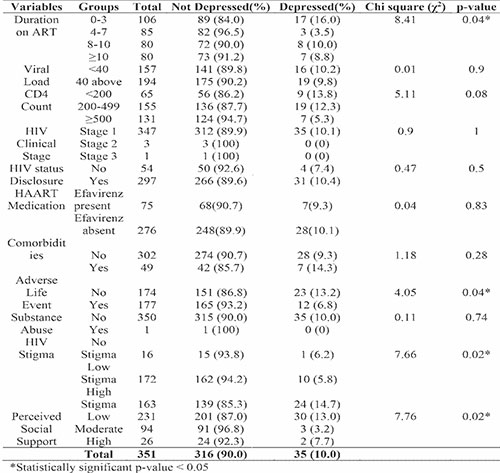
Discussion
The overall prevalence of depression of 10% observed in this study was comparable to the prevalence of 14.3% reported by Cohen et al among PLWH assessing care with health insurance across the United States in 2017.30 Similarly, Robertson and his team reported a prevalence of 15.7% among HIV infected persons in Canada and Western Europe in the CRANIum (sCReen for Anxiety, depression, and Neurocognitive Impairment in HIV+ patients) study. The study was a multi-national, multicentre study assessing neuropsychiatry impairment in HIV patients from 15 European countries and Canada.31 Although comparable, the study participants in these studies were mainly Caucasians. Nel and Kagee in a hospital-based study in South Africa reported a prevalence of 11.7% among HIV infected patients.14
Similarly, Wroe and his colleagues also reported a prevalence of 11.2% among patients attending HIV clinics in three health centres in Rwanda.15 A depression prevalence of 13% was reported by Wagner et al in a hospital based cohort study in Uganda.32 In Nigeria, Olisah and his team reported a prevalence of depression of 14.2% among patients attending a virology clinic at a tertiary hospital in Kaduna North-West Nigeria.33 Although comparable, their sample size was smaller than that used in this study.
Several studies however, reported prevalence of depression in PLWHA significantly higher than was recorded in this study. Vyanvaharkar and his colleagues working in Southern United States reported a prevalence of depression among HIV infected persons of 57.7% among African American women living in rural areas.24 The higher prevalence was because the study population was limited to only females who has been shown to be more prone to developing depression.34 Lawler reported a prevalence of 38% among HIV patients attending the Infectious Disease Care Clinic in Gaborone, Botswana.13 Prevalence of depression of 29.3% and 24.5% were reported by Chikezie et al and Umeadi among PLWHAs attending the HIV Clinic at the University of Benin Teaching Hospital Benin South-South Nigeria and Federal Medical Center, Umuahia, Abia State South-East Nigeria respectively.5,35 Although hospital based, these studies had significantly smaller sample sizes compared to this present study. Gaynes et al recoreded a substantially lower prevalence of 3% in a study among HIV patients in Cameroon.36
Assessing the pattern of severity of depression in this study, 69.2% had no depressive symptoms, 20.8% mild depressive symptoms, 7.1% had moderate depressive symptoms, 2.3% had moderately severe and 0.6% had severe depressive symptoms using the PHQ-9 tool. Other authors using the same tool also had similar findings.37–39 Musisi et al in Uganda observed that 70% of HIV patients had no symptoms, 19.2% with mild symptoms while 10.9% had moderate, moderately severe and severe depressive symptoms.37 Sule et al in Jos, Northcentral Nigeria, reported a severity pattern of 69% respondents with no depression, 26% mild, 4% moderate, 1% moderately severe and 0% severe depressive symptoms among HIV patients.38 Also, Onyebuchi-Iwudibia in Enugu, Southeast Nigeria observed a severity pattern of 66.7% respondents with no depression, 20% mild, 6.7% moderate, 2.9% moderately severe and 3.8% with severe depressive symptoms.39 Terloyeva et al in Kazakhstan and L’akoa et al in Cameroon also reported a pattern of severity predominantly mild depressive symptoms.21,40 In all, these findings show that majority of depressed person living with HIV had mild depressive symptoms. This trend is particularly worrisome because these symptoms are subtle and are easily missed by their caregivers, families, friends and even their healthcare providers.
On bivariate analysis the study observed a significant association between depression and low paying occupations, not being married, reduced duration on ART, adverse life events, HIV stigma and low perceived social support. This study found a statistically significant association between marital status and depression with divorced and single respondents more likely to develop depression than their married counterparts. Besa and his colleagues in Lusaka Zambia found that HIV patients with depression were more likely to be separated or widowed.12 Similarly, Abadiga in Ethiopia reported that being divorced, single and widowed were associated with depression.41 The loss or separation from a partner is usually associated with psychological and social challenges with lack of emotional and financial support which may eventually lead to depression in HIV patients.
A statistically significant association was found between the respondent’s occupation and depression in this present study. The prevalence of depression was observed to be higher among the unemployed and respondents who had low paying jobs such as artisans and farmers. This is in agreement with findings from Choi et al and Bekele et al, both in Canada, who reported that HIV infected persons who were unemployed/underemployed were more likely to be depressed.20,23 This may be attributed to the fact that the poor financial status of the unemployed/underemployed may represent a direct stressor causing depression. Furthermore, they may not have enough financial resources necessary to mitigate against mental health illness such as depression when it occurs.
This study found a significant association between the duration of HIV medication use and depression. Depression was found to be more prevalent among respondents that have used anti-HIV medications for shorter durations (6 months - 3 years). Since the HIV virus has been directly linked to the biologic development of depression by directly altering the neurotransmitter pathway, then elimination of the virus with ART with time should reverse this pathology.9,42 Hence HIV patients who have been on ART for longer periods should have reduced viral load and consequently reduced complications from HIV infection such as depression. Amiya et al in Nepal also reported significantly increased prevalence of depression among HIV patients on ART for less than two years.43 Similarly, Van Copperhagen and his colleagues in South Africa reported a similar finding.44
There was a negative association between depression and adverse life events in HIV patients. This contradicts the finding of Shittu et al who reported a positive association in Ilorin North-West Nigeria.16 Kinyanda et al in Uganda similarly reported an association between adverse life events, stress and depression among HIV positive persons.45 Stressful life events such as bereavement, financial failure, divorce, threat of separation, losing a job, relocation, retiring amongst others are psychosocial stressors that have been shown to trigger a state of depression particularly if the person does not possess healthy coping techniques.46–49 The finding from this study may be attributed to the fact that persons who experience major stressful life event may develop adaptive coping strategies that will in turn be protective against depression.
Depression was negatively associated with perceived social support. A longitudinal study carried out among homosexuals, heterosexuals and female PLWHA living in the United States by Mcdowell and Serovich also reported a significant relationship between low levels of perceived social support and depression/loneliness.50 Social support plays a significant regulating effect on the relationship between stress and depression by improving the sufferer’s self-esteem and self-efficacy, hence reducing the emergence of negative emotions such as depression.51
The results showed that 95.4% of the respondents perceived some form of HIV stigmatization, while 4.6% had none. This shows that HIV stigma is still very prevalent among PLWHA despite recent campaigns against it. This is particularly disturbing because stigma is associated with social rejection and exclusion. This feeling of exclusion and rejection may predispose the HIV patient to developing depression and other mental health issues. This study shows a positive relationship between increasing levels of HIV stigma and depression. This is in agreement with the findings of Tesfaw et al in Ethiopia, Kalomo in Namibia and Wagner et al in Uganda.52–54 In Nigeria, Umeadi in Umuahia and Onyebuchi-Iwudibia in Enugu South-East Nigeria reported a direct relationship between HIV stigma and depression, while Ndu in Enugu South-East Nigeria noted that 50.8% of HIV patients with depression attributed its cause to being stigmatized.35,39,55
Conclusion
The prevalence of depression (10%) in persons living with HIV/AIDS in this study is relatively high. This is particularly of major concern because these two diseases (HIV/AIDS and depression) are associated with significant morbidity. Majority of depressed person living with HIV had mild depressive symptoms which may be easily missed by their caregivers and primary care physicians. The study observed a significant association between depression and low paying occupations, not being married, reduced duration on ART, adverse life events, increased HIV stigma and low perceived social support.
Limitations
Respondents with atypical symptoms of depression may have been missed during screening. The cross-sectional design of the study limits assumption of causality. Finally, the instrument used to screen for depression depends on the respondent’s memory for recall of the previous two weeks, thus increasing the risk of recall bias.
References
- World Health Organization . HIV/AIDS [Internet]. [cited 2019 Dec 19]. Available from: https://www.who.int/features/qa/71/en/
- National Institute of Mental Health. HIV/AIDS and Mental Health [Internet]. [cited 2018 Jun 6]. Available from: https://www.nimh.nih.gov/health/topics/hiv-aids/index.shtml
- Malee K, Mellins CA, Huo Y, Tassiopoulos K, Smith R, Sirois PA, et al. Prevalence, Incidence and Persistence of Psychiatric and Substance Use Disorders Among Mothers Living with HIV. J Acquir Immune Defic Syndr. 2014;65(5):526–34.
- Vreeman RC, McCoy BM, Lee S. Mental health challenges among adolescents living with HIV. J Int AIDS Soc. 2017;20(3):100–9.
- Chikezie U, Otakpor A, Kuteyi O, James B. Depression among people living with Human Immunodeficiency virus/Acquired immunodeficiency syndrome in Benin city, Nigeria: A comparative study. Niger J Clin Pract. 2013;16(2):238–42.
- Abas M, Ali G., Nakimuli-Mpungu E, Chibanda D. Depression in people living with HIV in sub-Saharan Africa: time to act. Trop Med Int Heal. 2014;19(12):1392–6.
- Li L, Jae-Lee S, Thammawijaya P, Jiraphongsa C, Rotheram-Borus MJ. Stigma, social support and depression among PLWHA in Thailand. Natl Inst Heal Care. 2010;21(8):1007–13.
- Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food Insecurity, Depression and the Modifying Role of Social Support among People Living with HIV/AIDS in Rural Uganda. Soc Sci Med. 2013;74(12):2012–9.
- Guerra D, Fonseca J, Figueiredo V, Ziff E, Konkiewitz E. Human immunodeficiency virus-associated depression: contributions of immuno-inflammatory, monoaminergic, neurodegenerative, and neurotrophic pathways. J Neurovirol. 2013;19(4):314–27.
- Tsai AC, Mimiaga MJ, Dilley JW, Hammer GP, Karasic DH, Charlebois ED, et al. Does effective depression treatment alone reduce secondary HIV transmission risk? Equivocal findings from a randomized controlled trial. AIDS Behav. 2013;17(8):2765–72.
- Do AN, Rosenberg ES, Sullivan PS, Beer L, Strine TW, Schulden JD, et al. Excess Burden of Depression among HIV-Infected Persons Receiving Medical Care in the United States : Data from the Medical Monitoring Project and the Behavioral Risk Factor Surveillance System. PLoS One. 2014;9(3):1–10.
- Besa NM, Paul R, Hachaambwa L. Psychiatric symptoms among an HIV positive Urban Population in Lusaka , Zambia. Med J Zambia. 2015;42(2):84–9.
- Lawler K, Mosepele M, Seloilwe E, Ratcliffe S, Steele K, Nthobatsang RSA. Depression Among HIVPositive Individuals in Botswana: A Behavioral Surveillance. AIDS Behav. 2011;15(1):204–8.
- Nel A, Kagee A. The relationship between depression, anxiety and medication adherence among patients receiving antiretroviral treatment in South Africa. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2013;25(8):948–55.
- Wroe EB, Hedt-Gauthier BL, Franke MF, Nsanzimana S, Turinimana JB, Drobac P. Depression and patterns of self-reported adherence to antiretroviral therapy in Rwanda. Int J STD AIDS. 2015;26(4):257–61.
- Shittu RO, Issa BA, Olanrewaju GT, Mahmoud AO, Odeigah LO, Salami AK, et al. Prevalence and correlates of depressive disorders among people living with HIV/AIDS in North Central Nigeria. J AIDS Clin Res. 2013;4(11):1–7.
- Medsker B, Forno E, Simhan H, Juan C, Sciences R. Psychiatric disorders and adherence to antiretroviral therapy among a population of HIV-infected adults in Nigeria. Int J STD AIDS. 2016;70(12):773–9.
- Boing AF, Melo GR, Boing AC, Moretti-Pires RO, Peres KG, Peres MA. Association between depression and chronic diseases: results from a population-based study. Rev Saude Publica. 2012;46(4):617–23.
- Qato DM, Ozenberger K, Olfson M. Prevalence of prescription medications with depression as a potential adverse effect among adults in the United States. JAMA - J Am Med Assoc. 2018;319(22):2289–98.
- Bekele T, Rourke SB, Tucker R, Greene S, Koornstra J, Monette L, et al. Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care. 2013;25(3):337–46.
- Terloyeva D, Nugmanova Z, Akhmetova G, Akanov A, Patel N, Lazariu V, et al. Untreated depression among persons living with human immunodeficiency virus in Kazakhstan: A cross-sectional study. PLoS One. 2018;13(3):1–18.
- Eshetu DA, Woldeyohannes MS, Kebede MA, Techane GN, Gizachew KD, Tegegne MT, et al. Prevalence of Depression and Associated Factors among HIV / AIDS Patients Attending ART Clinic at Debrebirhan Referral Hospital , North Showa , Amhara Region , Ethiopia. Clin Psychiatry. 2015;1(1:3):1–8.
- Choi SKY, Boyle E, Cairney J, Collins EJ, Gardner S, Bacon J, et al. Prevalence, Recurrence, and Incidence of Current Depressive Symptoms among People Living with HIV in Ontario, Canada: Results from the Ontario HIV Treatment Network Cohort Study. Lima VD, editor. PLoS One. 2016 Nov 1;11(11):1–29.
- Vyavaharkar M, Moneyham L, Corwin S, Tavakoli A, Saunders R, Annang L. HIV disclosure, social support, and depression among HIV-infected African American women living in the rural South-Eastern United States. AIDS Educ Prev. 2011;23(1):78–90.
- Kroenke K, Spitzer RL. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr Ann. 2002;32(9):509–15.
- O’Brien CP. The CAGE questionnaire for detection of alcoholism: A remarkably useful but simple tool. JAMA - J Am Med Assoc. 2008;300(17):2054–6.
- Ewing JA. Detecting Alcoholism The CAGE Questionnaire. JAMA - J Am Med Assoc. 1984;252(14):1905–7.
- Kalichman S., Simbayi L., Cloete A, Mthembu P., Mkhonta R., Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93.
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 2010;52(1):30–41.
- Cohen JP, Beaubrun A, Ding Y, Wade RL, Hines DM. Estimation of the Incremental Cumulative Cost of HIV Compared with a Non-HIV Population. Pharmacoeconomics. 2020;10(1):1–10.
- Robertson K, Bayon C, Molina JM, McNamara P, Resch C, Muñoz-Moreno JA, et al. Screening for neurocognitive impairment, depression, and anxiety in HIV-infected patients in Western Europe and Canada. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2014;26(12):1555–61.
- Wagner GJ, Ghosh-Dastidar B, Garnett J, Kityo C, Mugyenyi P. Impact of HIV antiretroviral therapy on depression and mental health among clients with HIV in Uganda. Psychosom Med. 2012;74(9):883–90.
- Olisah VO, Baiyewu O, Sheikh TL. Adherence to highly active antiretroviral therapy in depressed patients with HIV/AIDS attending a Nigerian University Teaching Hospital Clinic. Afr J Psychiatry. 2010;13(4):275–9.
- Salk RH, Hyde JS, Abramson LY. Gender Differences in Depression in Representative National Samples: Meta-Analyses of Diagnoses and Symptoms. Psychol Bull. 2017;143(8):783–822.
- Umeadi CA. Effect of Social Support and HIV-Related Stigma on Depression in HIV / AIDS Patients. Walden University; 2015.
- Gaynes BN, Pence BW, Atashili J, O’Donnell J, Kats D, Ndumbe PM. Prevalence and predictors of major depression in HIV-infected patients on antiretroviral therapy in Bamenda, a semi-urban center in Cameroon. PLoS One. 2012;7(7):1–8.
- Musisi S, Wagner GJ, Ghosh-Dastidar B, Nakasujja N, Dickens A, Okello E. Depression and sexual risk behaviour among clients about to start HIV antiretroviral therapy in Uganda. Int J STD AIDS. 2014;25(2):130–7.
- Sule HM, Agbir MT, Agaba PA, Ojoh RO, Okonoda KM. Prevalence of Depression and Associated Factors in HIV-Positive Adults Attending an Antiretroviral Clinic in Jos, Nigeria. Niger J Fam Med Heal Care. 2018;4(4):26–32.
- Onyebuchi-Iwudibia O, Brown A. HIV and depression in Eastern Nigeria: The role of HIV-related stigma. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2014;26(5):653–7.
- Lakoa RM, Noubiap JJN, Fang Y, Ntone FE, Kuaban C. Prevalence and correlates of depressive symptoms in HIV-positive patients : a cross-sectional study among newly diagnosed patients in. BMC Psychiatry. 2013;13(228):1–7.
- Abadiga M. Depression and its associated factors among HIV/AIDS patients attending ART clinics at Gimbi General hospital, West Ethiopia, 2018. BMC Res Notes. 2019 Dec 20;12(527):1–8.
- Arseniou S, Arvaniti A, Samakouri M. HIV infection and depression. Psychiatry Clin Neurosci. 2014;68(07):96–109.
- Amiya RM, Poudel KC, Poudel-tandukar K, Pandey BD, Jimba M. Perceived Family Support , Depression , and Suicidal Ideation among People Living with HIV / AIDS : A Cross- Sectional Study in the Kathmandu Valley , Nepal. PLoS One. 2014;9(3):1–10.
- van Coppenhagen B, Duvenage HS. Prevalence of depression in people living with HIV and AIDS at the Kalafong provincial tertiary hospital antiretroviral clinic. South African J Psychiatry. 2019;25(0):1–6.
- Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11(1):205–14.
- Ren Z, Zhou G, Wang Q, Xiong W, Ma J, He M, et al. Associations of family relationships and negative life events with depressive symptoms among Chinese adolescents: A cross-sectional study. PLoS One. 2019;14(7):e0219939.
- Phillips AC, Carroll D, Der G. Negative life events and symptoms of depression and anxiety: stress causation and/or stress generation. Anxiety, Stress Coping. 2015;28(4):357–71.
- Sokratous S, Merkouris A, Middleton N, Karanikola M. The association between stressful life events and depressive symptoms among Cypriot university students: A cross-sectional descriptive correlational study. BMC Public Health. 2013;13(1121):1–16.
- Healthline. Depression Risks: Medical, Social, and Substance Factors [Internet]. [cited 2019 Oct 13]. Available from: https://www.healthline.com/health/depression/risk-factors#4
- Mcdowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19(10):1223–9.
- Wang X, Cai L, Qian J, Peng J. Social support moderates stress effects on depression. Int J Ment Health Syst. 2014;8(41):1–5.
- Wagner GJ, Holloway I, Ghosh-Dastidar B, Kityo C, Mugyenyi P. Understanding the influence of depression on self-efficacy, work status and condom use among HIV clients in Uganda. J Psychosom Res. 2011;70(5):440–8.
- Tesfaw G, Ayano G, Awoke T, Assefa D, Birhanu Z, Miheretie G. Prevalence and correlates of depression and anxiety among patients with HIV on- follow up at Alert Hospital , Addis Ababa. BMC Psychiatry. 2016;16(368):1–7.
- Kalomo EN. Associations between HIV-related stigma , self- esteem , social support and depressive symptoms in Namibia. Aging Ment Health. 2017;1360(78):1–7.
- Ndu AC, Arinze-Onyia SU, Aguwa EN, Obi IE. Prevalence of depression and role of support groups in its management : A study of adult HIV / AIDS patients attending HIV / AIDS Clinic in a tertiary health facility in South-eastern Nigeria. J Public Heal Epidemiol. 2011;3(4):182–6.