Grand-multiparity and its impact on delivery outcomes: A ten-year retrospective study at Aminu Kano Teaching Hospital, Kano
Adeyemi MT1, Adamou N1,2, Omeje I1, Muhammad ID1
Abstract
Background: Grandmultiparity, defined as having given birth to the fifth to ninth child, and great grandmultiparity, involving ten or more childbirths, present obstetric challenges due to their association with high-risk pregnancies. Adverse outcomes can strain resources and healthcare systems. This retrospective study examines the delivery outcomes of grandmultiparous women at Aminu Kano Teaching Hospital over a decade.
Methods: A retrospective analysis covered January 2012 to December 2021, involving women who delivered at the hospital. Data, including socio-reproductive characteristics, mode of delivery, complications, and outcomes, were extracted from records. SPSS version 25 was used for statistical analysis (p < 0.05).
Results: Grandmultiparous women accounted for 8.4% of parturients, primarily aged 30-39 (76.8%) with parity ranging from 5 to 9 (90.9%). Approximately 52% received antenatal care at the hospital or peripheral facilities. Most (73.2%) had spontaneous vaginal deliveries, 25.2% underwent cesarean sections, and 1.6% had instrumental deliveries. Complications included postpartum hemorrhage (27.6%), hypertensive disorders in pregnancy (19.9%), and malpresentation (7.2%). Neonatal outcomes revealed 21.8% low birth weight, 9.6% macrosomic infants, and 6.2% birth asphyxia.
Conclusion: The study highlights that grandmultiparity remains evident among parturients in tertiary hospitals, primarily in older and less educated women. It underscores the need for vigilant antenatal care to mitigate associated risks and improve maternal and neonatal outcomes. Tailored interventions for grandmultiparous women are essential to ensure their well-being and that of their newborns in high-risk pregnancies.
Keywords: Multiparity, maternal, neonatal, outcomes
Introduction
The International Federation of Gynaecology and Obstetrics (FIGO) has defined grand multipara as women who have given birth between their fifth and ninth times, while those who have delivered ten or more times are classified as great-grandmultiparas.1,2 Grand multiparity, in the context of obstetric performance, is recognized as a high-risk condition.3 It is often associated with adverse complications that can affect maternal, perinatal, or both outcomes.4 Research has shown that the best obstetric outcomes are typically observed in women with a parity of less than four. The risk to both the mother and the child is relatively high during the first pregnancy, gradually declines during the second and third pregnancies, and then starts to rise slowly with increasing parity. By the sixth pregnancy, these risks surpass those of the first, and they increase significantly with each subsequent pregnancy.5
Notably, the prevalence of grand multiparity varies considerably across different regions and countries. In developed nations, such as the United States, the prevalence is as low as 2.97%, whereas developing countries, including Tanzania, may report much higher rates, such as 9.44%. Remarkably, the Gambia has reported a prevalence as high as 26.5%.5-7 In Nigeria, the prevalence of grand multiparity also exhibits regional variations, with rates ranging from 4.11% in Lagos to 18.8% in Maiduguri.8-11 This divergence in prevalence is attributed to factors like cultural norms, religious beliefs, gender preferences, education levels, and the desire for larger families.12
Several factors contribute to the persistence of high grand multiparity rates, particularly in low-income countries. Early marriages, a desire for larger family sizes, inadequate access to specialized healthcare, limited availability and utilization of contraception, and the underperformance of family planning initiatives all play significant roles.13 Social determinants also come into play, as many grandmultiparous individuals may face economic hardships, lack formal education, suffer from psychological stress, and experience unemployment.14 These challenges can lead to health issues, such as anemia, which may persist from one pregnancy to the next due to inadequate nutritional support. Grandmultiparous women often prioritize the nutrition of their numerous children over their own health, leading to deficiencies in iron, vitamin B12, and folic acid. Moreover, their health needs may be neglected to avoid further financial strain on their families.15
The complications associated with grand multiparity are multifaceted and encompass various medical conditions and adverse outcomes. These include diabetes mellitus, hypertensive disorders, premature labor, malpresentation and malposition of the fetus, twin gestation, placenta previa, abruptio placentae, puerperal sepsis, uterine rupture, postpartum hemorrhage, utero-vaginal prolapse, precipitate labor, instrumental vaginal delivery, increased cesarean section rates, and maternal mortality. Perinatal complications linked to grand multiparity encompass intrauterine growth restriction, congenital malformations, fetal macrosomia, stillbirth, low Apgar scores, increased neonatal intensive care unit admissions, and perinatal mortality.16
In our specific environment, these complications may be even more pronounced due to limited improvement in socioeconomic status and a lack of adequate maternal and child health facilities, particularly at the primary and secondary levels of healthcare. Despite the health implications of high parity and its decline in industrialized societies, the prevalence of grand multiparity remains elevated in sub-Saharan Africa and other developing regions. This places an increased burden on families, compromises economic stability, and strains healthcare systems, given the adverse obstetric outcomes associated with high parity.10
Furthermore, in our region, there is a paucity of research focusing on the obstetric outcomes of grandmultiparous women. Therefore, this study seeks to fill this gap by aiming to determine the outcomes of grandmultiparous women who delivered at Aminu Kano Teaching Hospital, Kano. Through this research, we aim to provide valuable insights into the unique challenges and risks faced by grandmultiparous women in our local healthcare context.
Methodology
Study design: This study employed a retrospective design to analyze the delivery outcomes of all pregnant women who gave birth at Aminu Kano Teaching Hospital over a ten-year period, from January 2012 to December 2021.
Data collection: The hospital identification numbers of grandmultiparous women managed in labor during the specified period were obtained from the in-patient registers in the labor ward and postnatal ward. Using these identification numbers, the researchers retrieved the case notes of the identified grandmultiparous women from the hospital's record department. Relevant information, including socio-reproductive characteristics, parity, mode of delivery, complications, and maternal and fetal outcomes, was meticulously extracted from the retrieved case notes. This data was systematically recorded in a predetermined proforma.
Inclusion and exclusion criteria: This study included antenatal women who had previously given birth to five or more viable children, classifying them as grandmultiparous. This criterion ensured that the focus was on grandmultiparous women with significant obstetric experience.
Women with fewer than five viable children were excluded from the study to maintain a clear distinction between grandmultiparous and non-grandmultiparous individuals. Additionally, multiple pregnancies were considered as singleton pregnancies, and cases involving abortion, ectopic pregnancy, or hydatidiform mole were excluded when determining parity. This allowed for a more accurate assessment of the parity status of the included women.
Data analysis: The collected data was subjected to statistical analysis using SPSS statistical software (version 25). The results were presented through frequency distributions, tables, and charts. To determine statistical significance, the Chi-square test was employed, with a significance level set at P < 0.05.
Results
Over the ten-year period from January 2012 to December 2021, a total of 38,573 deliveries took place at Aminu Kano Teaching Hospital. Among these deliveries, 3,239 were attributed to grandmultiparous women, yielding a prevalence rate of 8.4%. Out of the 3,239 grandmultiparous deliveries, 2,921 case records were successfully retrieved from the hospital's records department for detailed analysis, resulting in a retrieval rate of 90.1%.
Socio-demographic characteristics
The age range of the grandmultiparous women spanned from 20 to 47 years, with the majority falling within the 30-39 age bracket, comprising 2,245 individuals (76.8%). The mean age was calculated at 34.97 years, with a standard deviation of 4.13 years. The youngest participant was 23 years old, while the eldest was 47 years old. Regarding education, a significant portion of the women, 1,904 (65.2%), had some level of formal education, while 1,017 (34.8%) had no formal education. Among these women, 2,655 (90.9%) had a parity ranging from 5 to 9 (para 5-9), while 266 (9.1%) had a parity of 10 or above. Approximately 1,520 (52%) of the grandmultiparous women booked and received antenatal care (ANC) either at the teaching hospital or in other peripheral healthcare facilities. Conversely, 1,401 (48%) were unbooked, indicating that they did not receive formal ANC. These are shown in Table 1.
Table 1: Socio-demographic characteristics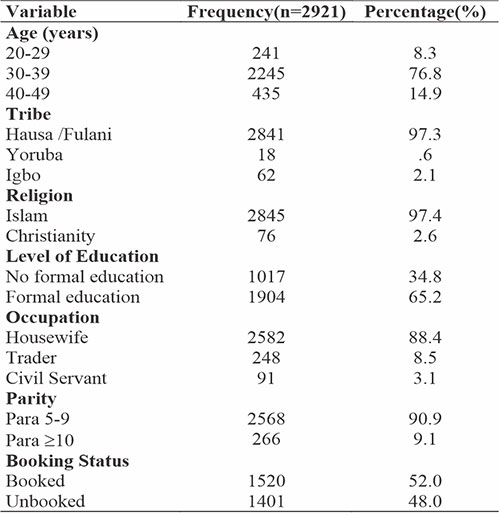
Maternal outcomes
The maternal outcomes of grandmultiparous women were analyzed (see Table 2), revealing that a significant proportion of them, 1,266 (43.3%), experienced complications. Notable complications included postpartum hemorrhage observed in 806 (27.6%) cases, hypertensive disorders in pregnancy affecting 583 (19.9%) women, malpresentation in 209 (7.2%) cases, and gestational diabetes mellitus in 138 (4.7%) instances. Other complications included prolonged labor in 57 (2.0%) cases, cephalopelvic disproportion in 55 (1.9%) and puerperal sepsis in 69 (2.4%) women. Spontaneous vaginal deliveries was the mode of delivery for the majority, 2,137 (73.2%), while 737 (25.2%) women underwent cesarean sections, and 47 (1.6%) had instrumental deliveries.
Table 2: Maternal outcome and complications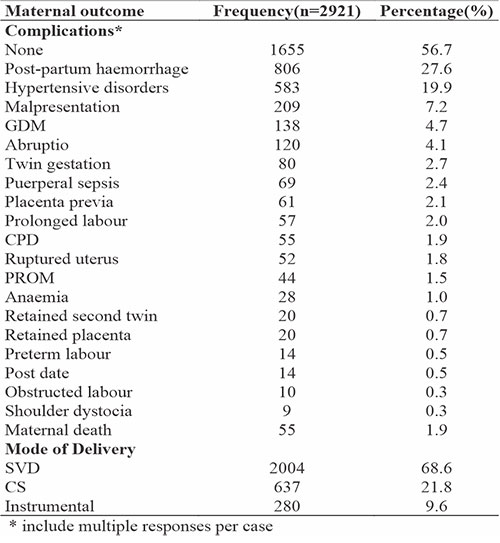
The majority of grandmultiparous women, 2,866 (98.1%), were discharged alive after delivery, while 55 (1.9%) sadly passed away during their admission. Notably, those with a parity of ten and above faced a higher maternal mortality rate than those women with a parity of 5 to 9, underscoring a statistically significant finding (p=0.002). This is shown in Table 3.
Table 3: Neonatal outcome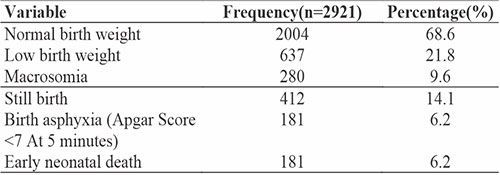
Neonatal outcomes
Neonatal outcomes were examined (Table 4), revealing that 2,004 neonates (68.6%) had normal birth weights. A portion of 637 neonates (21.8%) were classified as low birth weight babies, while 280 (9.6%) were macrosomic infants. Additionally, 181 neonates (6.2%) experienced birth asphyxia, while 412 (14.1%) were stillborn, and 181 (6.2%) sadly passed away during the early neonatal period.
Table 4: Comparison of maternal mortality between grandmultiparous and great-grandmultiparous women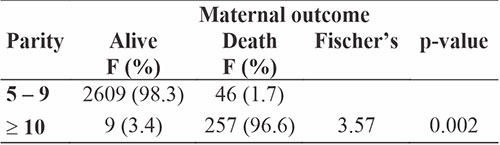
Discussion
This retrospective study spanning a decade aimed to assess the fetomaternal outcomes of grandmultiparous women delivering at Aminu Kano Teaching Hospital. The study revealed a prevalence of grand multiparity at 8.4%, which is notably lower than the rates reported in other regions of Nigeria such as Maiduguri (18.8%) and Enugu (16.4%).8,9 The lower prevalence observed in this study may be attributed to factors such as a significant proportion of grandmultiparous women opting for home births, limited utilization of hospital services, and possibly increased adoption of family planning methods within the community. Additionally, the availability of free maternity services in state-owned hospitals may have influenced the choice of healthcare facility. This decline in grandmultiparity prevalence reflects a positive trend towards lower parity, akin to figures seen in developed countries like the United States (4.7%)6 and London (1.9%).22
Grandmultiparous women were found to be generally older, with approximately 76% falling within the 30-40 age range, similar to findings in Uyo, Nigeria, and India.19,20 However, this advanced maternal age carries associated risks, including obesity, chronic hypertension, placenta previa, placental abruption, gestational diabetes mellitus, and macrosomic infants, posing threats to both mother and fetus.
A significant majority of the grandmultiparous women in this study were housewives (88.4%), a trend paralleled in India (85.2%).20 Furthermore, a substantial proportion had no formal education (62% in Maiduguri),8 possibly linked to early marriages and limited opportunities for education among women in this demographic. The absence of formal education may correlate with commencing their obstetric careers early in life, leading to an increased likelihood of becoming grandmultiparous.
In terms of parity, the majority of grandmultiparous women (54.4%) in this study were para 5 and 6, aligning with findings in Awka (59.3%).21 However, only 52% of the participants sought antenatal care, which is comparatively lower than rates reported in Enugu (83%)9 and Maiduguri (91%).8 This lower antenatal care utilization among grandmultiparous women may be attributed to a sense of overconfidence due to previous parous experiences.
Regarding delivery, most grandmultiparous women (73.2%) had spontaneous vaginal deliveries, while a quarter underwent cesarean sections. A higher rate of emergency cesarean sections was observed, possibly due to a high incidence of fetal malpresentation and fetal distress.
Hypertensive disorders in pregnancy and gestational diabetes mellitus, known risks associated with grand multiparity, were prevalent in this study (20.0%), likely influenced by the advanced maternal age of the participants. This finding echoes a study by Khan et al. (16%)22 and can be attributed to factors such as advanced maternal age, obesity, cardiac disease, vascular disease, renal parenchymal disease, and genetic predisposition.23
Postpartum hemorrhage, a common complication in grandmultiparas due to uterine atony, was noted in 27.6% of cases, higher than rates in Anambra (13.3%),21 Maiduguri (14.3%),8 and India (14%).22 Factors contributing to this increased risk include decreased uterine contractility, scarring, exhaustion, and atherosclerotic changes in uterine vasculature.24
Maternal mortality in this study was found to be 1.9%, lower than rates reported in Oshogbo (5.1%)2 and India (4%).20 This reduced maternal mortality is attributed to improved obstetric care, careful labor management, judicious use of oxytocics, the availability of blood transfusion services, and the presence of skilled obstetricians.
Neonatal outcomes revealed a high incidence of low birth weight (21.8%), macrosomia (9.6%), birth asphyxia (6.2%), stillbirth (14.1%), and early neonatal death (6.2%). These rates were higher compared to observations in Maiduguri and India, potentially due to advanced maternal age and underlying medical conditions. The loss of a child has been identified as one of the determinants of grand multiparity.16 To mitigate these risks, a multidisciplinary approach involving obstetricians, pediatricians, and internal medicine specialists is crucial for managing high-risk grandmultiparous women and achieving favorable maternal and perinatal outcomes.
Conclusion
The prevalence of grandmultiparity in this study was observed to be 8.4%. A significant proportion of the women in this category were housewives, advanced in age, and had no formal education. Notable complications included hypertensive disorders in pregnancy, malpresentation, and gestational diabetes mellitus, often resulting in cesarean deliveries. Neonatal outcomes were suboptimal, as indicated by a high rate of low birth weight babies, birth asphyxia, and stillbirths.
Recommendations
Based on the findings of this study, the following recommendations are put forth:
- Obstetricians should emphasize and encourage all women to seek and utilize antenatal care services, irrespective of their previous parity experiences. This proactive approach can play a pivotal role in preventing maternal morbidity, mortality, and perinatal mortality.
- Government bodies and stakeholders should prioritize and invest in girl child education to enhance literacy levels. This education can help women understand the importance of family size limitation, thereby reducing the complications associated with grandmultiparity.
- Healthcare providers and community health programs should ensure accessible and comprehensive family planning services. This includes education on various contraceptive methods, counseling tailored to individual needs, and easy access to birth control measures. Implementing these recommendations can contribute significantly to reducing the prevalence of grandmultiparity in the community.
References
- Payal A, Dipti C. Study of maternal and fetal outcome of grand multipara. Int J Med Biomed Stud. 2020;4:48–50.
- Afolabi A, Adeyemi A. Grand-multiparity: Is it still an obstetric risk? J Obstet Gynaecol (Lahore). 2013;3:411–5.
- Njoku C, Abeshi S, Emechebe C. Grand Multiparity: Obstetric Outcome in Comparison with Multiparous Women in a Developing Country. J Obstet Gynaecol (Lahore). 2017;7:707–18.
- Mgaya A, Massawe S, Kidanto H, Mgaya H. Grand multiparity: is it still a risk in pregnancy? BMC Pregnancy Childbirth. 2013;13:241–9.
- Idoko P, Nkeng G, Anyawu M. Reasons for current pregnancy amongst grand multiparous Gambian women - a cross sectional survey. BMC pregnancy childbirth. 2016;16:217–21.
- Bornstein E, Eliner Y, Chervenak F, Grünebaum A. Concerning trends in maternal risk factors in the United States:1989-2018. Am J Obstet Gynecol. 2020;222:428–9.
- Muniro Z, Tarimo C, Mahande M, Mchome B, Maro E. Grand multiparity as a predictor of adverse pregnancy outcome among women who delivered at a tertiary hospital in Northern Tanzania. BMC Pregnancy Childbirth. 2019;19:1–8.
- Geidam A, Audu B, Oummate Z. Pregnancy outcome among grand multiparous women at the University of Maiduguri Teaching Hospital: A case control study. J Obstet Gynaecol (Lahore). 2011;31:404–408.
- Eze J, Okaro J, Okafor M. Outcome of Pregnancy in the Grand multipara in Enugu,Nigeria. Trop J Obs Gynaecol. 2006;23:8–11.
- Emechebe C, Njoku C, Eyong E, Madueke K. The social class and reasons for grand multiparity in Calabar, Nigeria. Trop J Obs Gynaecol. 2016;33:327–31.
- Ogedengbe O, Ogunmokun A. Grandmultiparity in Lagos, Nigeria. Niger Postgr Med J. 2004;10:216–9.
- Oshodi K, Salami K. Sociocultural Factors Influencing Grand Multiparous Practices in Ibadan, Nigeria. Niger J Sociol Anthropol. 2017;15:55–68.
- Ozori E, Fumudoh B, Makinde O, Oriji P. Maternal and neonatal outcomes in grand multiparous women delivered at a tertiary hospital in Niger-Delta, Nigeria. Yenagoa Med J. 2020;2:38 – 46.
- Ikeanyi E, Ayuba I. Grandmultiparity: The Reasons Women Give for High Parity in South-South Nigeria. Clin Med Res. 2017;6:92–8.
- Jibrin I, Isah A, Abdullahi I. Pregnancy outcome among grand multiparous women in a tertiary hospital in Abuja. Eur J Pharm Med Res. 2018;5:685–90.
- Elmugabil A, Hassan B, Alhabrdi N, Ahmed A, Rayis D, Adam I. Maternal and neonatal outcomes of grand multiparity in Khartoum, Sudan. Afri Heal Sci. 2022;22:164–71.
- Nigeria Demographic and Health Survey Final Report, Abuja 2018 [Internet]. [cited 2022 Dec 20]. Available from: https://dhsprogram.com/pubs/pdf/SR264/SR264.pdf
- Ibrahim A, Takai I, Rahila G. Trends of contraceptive utilisation in aminu kano teaching hospital, Northern Nigeria. Kanem J Med Sci. 2015;9:8–14.
- Abasiattai A, Utuk N, Udoma E, Umoh A. Grandmultiparity: Outcome of Delivery in a Tertiary Hospital in Southern Nigeria. Niger J Med. 2013;20:345–8.
- Singh S, Chawan J, Mangla D. A descriptive study: maternal and fetal outcome of grand multipara. Int J Reprod Contracept Obs Gynecol. 2015;4:219–23.
- Ikeako L, Nwajiaku L. Grandmultiparity: experience at Awka, Nigeria. Niger J Clin Pract. 2010;13:301–5.
- Khan N, Perveen S, Begum Z, Qayyum R, Malik R. Grand multiparity and maternal outcome in absence of adequate antenatal care. J Postgr Med Inst. 2017;31:67–71.
- Ogbe A, Ogbe B, Ekwempu C. Obstetric Outcome in Grandmultiparous Women in Jos University Teaching Hospital. Jos J Med. 2012;6:39–43.
- Chukwudebelu W. Preventing Maternal Mortality in Developing Countries. In: Okonofua F, Odunsi K, editors. Contemporary Obstetrics and Gynaecology for Developing Countries. 2nd ed. Benin: Women’s Health and Action Research Centre (WHARC); 2021. p. 644–57.