Sensitivity and Specificity of Digital Rectal Examination for the Diagnosis of Prostate Cancer at the Kano Teaching Hospital- A Comparative Analysis
Bashir Y1,2, Ayun C2,3, Muzzammil A1, Sharfuddeen AM1, Sani AA1, Sani UA1
Abstract
Background: Prostate cancer (CaP) is the most common non-cutaneous cancer among males and the fourth most common cause of cancer in males globally. Unfortunately, Sub-Saharan Africa lacks the relevant resources and organized screening program that has led to the late presentations in the region. Digital rectal examination (DRE) is a test commonly used to screen for prostate carcinoma and is by far the oldest and cheapest modality available for screening.
Objective: We hypothesized that digital rectal examination has a correlation to the diagnosis of prostate cancer. This study was meant to evaluate the sensitivity and specificity of DRE in the diagnosis of prostate cancer and compare the outcome to published data.
Methodology: This is a prospective study conducted at the Aminu Kano Teaching Hospital involving 87 symptomatic patients who were screened for prostate cancer (2014). Patient with DRE suspicious of malignancy i.e. (nodular, hard, asymmetrical prostate) or PSA >4ng/ml despite the prostate consistency were included in the study. The digital rectal exams were performed in a lateral decubital position to assess the prostate consistency and underwent transrectal ultrasound guided sextant biopsy for histological diagnosis.
Results: There was a total of 87 participants that underwent DRE in the study with age range from 50 – 96 years. Univariate analysis showed a mean age of 68.1 years with standard deviation of (SD +9.4). The detection rate of prostate cancer was 28.7%. Bivariate analysis of DRE to diagnosis of prostate cancer showed a sensitivity of 68.0% and specificity of 83.9%. The positive predictive value and the negative predictive value were 63.0% and 86.7% respectively. The study showed some evidence of a relationship between DRE and the diagnosis of prostate cancer with a (Pearson Chi Square Test=23.4, df=1,) with a statistical significance (p=<0.001).
Conclusion: PSA and Digital rectal exam combined have a higher sensitivity in the diagnosis of prostate cancer. However, DRE alone has a lower sensitivity but a much higher specificity in the diagnosis of CaP. DRE still has a role in the diagnosis of CaP because it is minimally invasive, cheaper and can detect some prostate cancers that are missed by PSA screening.
Keywords: Digital Rectal Exam (DRE), Prostate Cancer, Sensitivity, Specificity
Introduction
Prostate cancer (CaP) is the most common non-cutaneous cancer among males and the fourth most common cause of cancer in males globally.1,2 Nearly 32000 men are diagnosed in the UK each year, out of which 9000 will die of the disease.3 The incidence in Nigeria (127/100,000) is comparable to that in African American men, with an annual death rate of about 20,000.3
In 2012 the U.S. Preventive Services Task Force recommended against the routine use of PSA based screening for prostate cancer but did not fully address screening via digital rectal exam (DRE).4,5 The American Urologic Association recommends “informed decision with a doctor” starting at age 40 with baseline PSA and digital rectal examination.4
The increasing level of awareness and availability of wide‑spread screening programs for prostate cancer has led to early detection in developed nation.6 Unfortunately, Sub-Saharan Africa lacks the relevant resources and organized screening program that has led to the late presentations in the region.6 The currently available modalities for screening or early detection of prostate cancer are digital rectal examination (DRE), prostate specific antigen (PSA) testing, and transrectal ultrasound scan (TRUS).6
Digital rectal examination (DRE) is a test commonly used to screen for prostate carcinoma and is by far the oldest and cheapest modality available for screening.4,6 Although DRE has not been found to be effective in preventing metastatic prostate cancer or death from prostate cancer, few studies have shown that DRE does detect some prostate cancers that are missed by PSA screening.7 In spite of the high sensitivity of PSA, the diagnostic yield is augmented when it is combined with digital rectal examination.2 Moreover, a study by Catalona et al. reported 20% of prostate cancer following suspicious DRE in men with normal PSA (<4ng/ml).8
We hypothesized that digital rectal exam has a correlation to the diagnosis of prostate cancer. The study objective was meant to evaluate the sensitivity and specificity of digital rectal exam in the diagnosis of prostate cancer and compare the outcome to published data. The analysis was intended to determine the role of DRE as a screening tool for prostate cancer.
Methodology
This is a prospective study conducted at the Aminu Kano Teaching Hospital (2014) involving 87 patients who were screened for prostate cancer presenting with both irritative and obstructive symptoms. Patient with digital rectal exam suspicious of malignancy i.e. (nodular, hard, asymmetrical prostate) or PSA >4ng/ml despite the prostate consistency were included in the study. The digital rectal examinations were performed in a lateral decubitus position to assess the prostate consistency. All the examinations were done by specialist urologists. Each patient underwent transrectal ultrasound guided sextant biopsy of the prostate. A univariate analysis of mean, range and standard deviation of age was evaluated using the IBM SPSS statistical software. The statistical significance between variables were determined through a Chi Square Test and p-value. We used the following statistical equations below to assess the sensitivity and specificity, the positive predictive value and detection rate of digital rectal examination in the diagnosis of prostate cancer:
- Detection rate= population with prostate cancer/total population screened times 100.
- Percentage of abnormal DRE= population with abnormal prostate examination on palpation (nodule, asymmetry, hard) as a percentage of total population screened.
- Positive predictive value of DRE= percentage of positive biopsies/total positive DRE.
- DRE sensitivity= percentage of abnormal DRE/total positive biopsies.
- DRE specificity= percentage of normal DRE/total negative biopsies.
The Literature was searched using PubMed, African Journal Online, Google Scholar electronic data bases. Studies on the sensitivity and specificity of digital rectal examination in the diagnosis of prostate cancer were included in the study and compared against the outcome from our center as shown (table 1) below.
Results
Table 1: Univariate Analysis of Age![]()
Table 2: Bivariate analysis of digital Rectal Exam and Histology Cross tabulation to assess the sensitivity, Specificity, the positive predictive value, negative predictive value and detection rate of prostate cancer.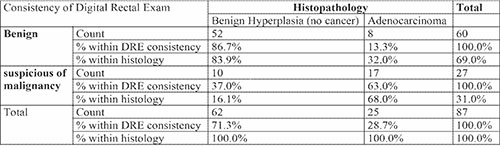
Table 3: Chi-Square Tests showing evidence of relationship between DRE and the diagnosis of Prostate Cancer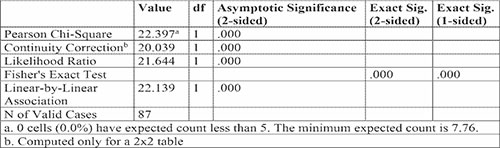
Table 4: Literature Review tabulation of various studies on DRE and the diagnosis of CaP considering the following parameters as study population, age range, detection rate sensitivity, specificity, positive and negative predictive values
There was a total of 87 participants that underwent DRE in the study with age range from 50 – 96 years. Univariate analysis showed a mean age of 68.1 years with standard deviation of (SD +9.4) shown below in table 1. The peak age range of patients screened was 60-69 years accounting 33/87 (35.5%) of the study population. The detection rate of prostate cancer was 28.7%. Bivariate analysis of DRE to diagnosis of prostate cancer showed a sensitivity of 68.0% and specificity of 83.9%. The positive predictive value and the negative predictive value were 63.0% and 86.7% respectively tabulated in table 2 below. The study showed some evidence of a relationship between DRE and the diagnosis of prostate cancer with a (Pearson Chi Square Test=23.4, df=1,) with a statistical significance (p=<0.001) as displayed in table 3.
Discussion
There are not many published data on the correlation of DRE for the diagnosis of prostate cancer. The age range in our study was (50-96 years) with similar reports by El-Hahas et al and Manyahi et al.9,10 Other studies showed a much younger age range6,11,12 as some of the participants in those reports may have presented with lower obstructive urinary symptoms requiring investigation or had a significant family history of prostate cancer. The mean age of diagnosis 68.1+9.4 years is comparable to other studies including Walsh et al., Ojewola et al., Manyahi et al.2,6,10,12 The highest burden of prostate cancer was seen in ages 60- 69 years with similar results displayed by Ojewola, et al.6
The detection rate of prostate cancer in this study (28.7%) is much higher than other reported studies (1.8%, 2.2%, 7.3%)7,9,13 which included one prospective study[9] and pooled analysis of data from two metanalysis by (Mistry et al. and Hoogendam et al.) respectively.7,13 The variability in the statistical results to our data may be alluded to the much larger sample sizes and the inclusion criteria of these reports. Nevertheless, data from (Jones et al, Ojewola et al and Irekita et al) as shown above in (Table 4) revealed a greater detection rate than our study.
Bivariate analysis of digital rectal in the diagnosis of prostate cancer revealed a sensitivity of 68.0% and specificity of 83.9% with a positive predictive value and negative predictive value of 63.0% and 86.7% respectively, statistically significant with (p=<0.001). This result showed that there was evidence of correlation between DRE and diagnosis of prostate cancer. The relatively lower sensitivity (68%) found in this study correlates numerically with other published data4-7,9,10 as shown above in (Table 4). Two meta-analysis by (Mistry et al. and Hoogendam et al.) and a systemic review by (Jones et al) showed a comparatively lower sensitivity (53.2%, 59.0% and 28.6%) respectively. The study provided a much higher specificity (83.9%) which is supported by much evidence from two meta-analysis7,13 and one systemic review5 with similar results (83.0%, 94.0% and 90.7%) respectively.
Limitations to this study was its much lower sample size that could have impacted the statistical analysis and the study design which is prone to selection bias. Practically, there is an inter-observer variability amongst Urologists performing a digital rectal exam; this could have altered the indication for a prostate biopsy.
Conclusion
The diagnosis of prostate cancer is still a challenge in much of Sub-Saharan Africa. Screening programs are poorly organized and lack appropriate funding. PSA and Digital rectal exam combined have a higher sensitivity in the diagnosis of prostate cancer. However, DRE alone has a lower sensitivity but a much higher specificity in the diagnosis of CaP. DRE still has a role in the diagnosis of CaP because it is minimally invasive, cheaper and can detect some prostate cancers that are missed by PSA screening.
Acknowledgement
Special thanks to the Department of Surgery, Bayero University/Aminu Kano Teaching Hospital, Kano, Nigeria.
Conflict of Interest
The authors declare no conflict of interest regarding this article.
Funding
No external funding available to disclose.
References
- Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of 25 major cancers in 1990. Int J Cancer 1999; 80:827.
- R. W. Ojewola, K. H. Tijani, E. A. Jeje. An Evaluation of Usefulness of Prostate Specific Antigen and Digital Rectal Examination in the Diagnosis of Prostate Cancer in an Unscreened Population: Experience in a Nigerian Teaching Hospital. West Afr J Medicine (2013)32(1):10-13
- Yunusa B, Abdullahi M, Mashi SA, Aji SA, Alhassan SU. Determination of the sensitivity and specificity of serum prostate-specific antigen in the diagnosis of prostate cancer in Kano, Northwestern Nigeria. Niger J Basic Clin Sci 2017;14:88-91
- DiGiorgio L, Patel N, Bargman V, Weiss R. The diagnostic value of digital rectal examination for prostate cancer: an analysis of over 20,000 biopsies. the journal of urology Vol. 197, No. 4S, Supplement, Saturday, May 13, 2017
- Jones D, Friend C, Dreher A. The diagnostic test accuracy of rectal examination for prostate cancer diagnosis in symptomatic patients: a systematic review BMC Family Practice (2018) 19(79):1-6
- Ojewola RW, Jeje EA, Tijani KH, Ogunjimi MA, Anunobi CC. Clinico-pathological correlation of digital rectal examination findings amongst Nigerian men with prostatic diseases: A prospective study of 236 cases. Niger J Surg 2013;19:26-31.
- Mistry K, Cable G. Meta-Analysis of Prostate-Specific Antigen and Digital Rectal Examination as Screening Tests for Prostate Carcinoma JABFP March–April 2003 Vol. 16 No. 2:95-101
- Catalona WJ, Ramos CG, Carvalhal GF, Yan Y. Lowering PSA cutoffs to enhance detection of curable prostate cancer. Urology. 2000;55:791–795. [PubMed]
- El-Hahas, Abol-enein H, Abdel-Khalek M. A Rationale for Prostate Cancer Detection in A Developing Country: Comparison of Screening and Case Findings. Afr J Urol. (2003) 9(3):123-128
- Manyahi JP, Musau P, Mteta AK. Diagnostic Values of Digital Rectal Examination, Prostate Specific Antigen And Trans-Rectal Ultrasound In Men With Prostatism East African Medical Journal Vol. 86 No. 9 September 2009 :45-453
- Irekpita E, Owobu C, Aibbe E. Assessment of DRE and PSA as diagnostic and screening Tool for Carcinoma of the Prostate in Rural Nigeria. East Cent, Afr J Surg (2014) 19(30):53-58
- Walsh A, Considine S, Thomas A, Lynch T, Manecksha RP. Digital rectal examination in primary care is important for early detection of prostate cancer. Br J Gen Pract 2014; DOI:10.3399/bjgp14X682861
- Hoogendam A, Buntinx F and de Vet HCW. The diagnostic value of digital rectal examination in primary care screening for prostate cancer: a meta-analysis. Family Practice 1999; 16: 621–626.