A 5-year review of hysterectomy at the Delta State University Teaching Hospital, Oghara, south-south Nigeria
Ukah C E1, Okhionkpamwonyi O1,2, Okoacha I1,2, Okonta P I1,2
Abstract
Context: Hysterectomy is a major surgical procedure that is performed worldwide for several indications ranging from benign to malignant conditions. It may be life-saving especially in certain obstetric situations.
Objective: The aim was to determine the incidence, indications and complications of hysterectomy in Delta State University Teaching Hospital (DELSUTH), Oghara.
Materials and methods: This was a retrospective descriptive study of hysterectomy performed in DELSUTH, Oghara from January 1st, 2012 to December 31st 2016. Every patient that had hysterectomy was included.
Results: During the period, there were there 468 major gynaecological surgeries. Eighty-five patients had hysterectomy accounting for 18.2%. The mean age of the patients was 47.9±10.6 years. Majority (46.6%) of the patients were para 5 and above. The mean parity was 3.2±0.83. Uterine fibroid accounted for majority (30.0%) of the cases. Total abdominal hysterectomy accounted for 78.75% while 8.75% had sub-total abdominal hysterectomy and 12.5% had vaginal hysterectomy. Fifty-two percent of the patients had bilateral salpingo-oophorectomy while 6.25% had unilateral salpingo-oophorectomy. Anaemia and wound sepsis were the most common complications. One patient (1.25%) ended as a mortality during the period under review.
Conclusion: The indications for, and surgical outcome following hysterectomy are comparable to that from other public hospitals across the country.
Keywords: Hysterectomy, indications, complications, DELSUTH.
Introduction
Hysterectomy is a word that originates from hysteros, a Greek word that means uterus. It was first coined in 1889 and it simply means surgical removal of the uterus including the cervix.1 Depending on the patient’s conditions and risk factors, the ovaries, fallopian tubes, upper portion of vagina and pelvic nodes may also be removed. There are different routes through which the uterus can be assessed at surgery- abdominal, vaginal, laparoscopic and a combination of vaginal and laparoscopic routes.2
Differences exist in the rate of hysterectomy from country to country and in different settings in Nigeria. In Nigeria, it accounted for 8.5% to 18.2% of all major gynaecological operations in both secondary and tertiary health care facilities across Nigeria.1,6-14 Approximately 20% of women at age 55 would have undergone hysterectomy in the United Kingdom, mainly for menstrual disorders and uterine fibroids.4 In the United States, an average of 622,000 hysterectomies are performed every year;1 and the procedure is the next most commonly performed major surgery, after caesarean section in reproductive aged women.5 Also in Demark an estimated one in every ten women would have hysterectomy in their life time.1
Studies done in the Niger Delta region of Nigeria, where DELSUTH is located, have reported abdominal hysterectomy to account for 81.9% to 91.6% of all hysterectomies being done.9,10,12,13 The commonest indication for hysterectomy in our setting is uterine fibroid and menstrual problems as in developed countries except that the uterine fibroid are larger in our environment due to late presentation.15 Other indications include dysfunctional uterine bleeding, adenomyosis, endometriosis and pelvic organ prolapsed.8-10,15
Hysterectomy has a number of complications associated with it and they include haemorrhage, wound infection, bladder injury, ureteric injury, injury to the bowels, urinary tract infection and paralytic ileus.9,10 Others include pelvis sepsis/ collection, vault haematoma and pulmonary embolism. Death can occur as a result of complication of the procedure or anaesthesia.2
Majority of women are relieved of symptoms after hysterectomy and expressed satisfaction with the procedure on follow up.12 However, in the developing countries, many women are adverse to hysterectomy for the fear associated with surgery, loss of feminity and sexual rejection by their spouses2 or because of their religious beliefs and cultural attachment to child bearing potential and menstruation.16 Others believe that when they reincarnate they will live without a uterus or suffer primary infertility in the future.2,15
Although several works have been done on hysterectomy, none has been reported in this new centre. The findings from this study would document the incidence, indications and morbidities and/or mortalities associated with hysterectomy which would serve as a baseline for subsequent reviews to measure improvements in management of hysterectomy in the centre.
Materials and methods
This was a five-year retrospective descriptive study which was conducted between January 2012 and December 2016 at the department of Obstetrics and Gynaecology of Delta State University Teaching Hospital, Oghara. Delta State University Teaching Hospital is located in Oghara town of Delta state in the Niger-Delta region of Nigeria. It is a tertiary hospital which consists of highly specialized teams in all the various specialties of clinical practice.
Case notes of patients who were evaluated and had hysterectomy at the Delta State University Teaching Hospital over a five year period between 1st January 2012 and 31st December 2016 were retrospectively reviewed. Gynaecological admission registers, clinic records and theatre records were searched to ascertain the number of patients and their case file numbers. The case notes of the patients were thereafter retrieved from the medical record department and relevant information extracted. All patients who had hysterectomy in DELSUTH within the period under review were included.
Permission to access hospital records and data for this study was obtained from the hospital management and ethical approval was obtained from the hospital’s Health Research and Ethics Committee.
Data collected; socio-demographic characteristics (age, parity), indication for hysterectomy, type of hysterectomy, type of incidental surgery (when done), intra & post-operative complications were extracted from the case notes. The completed data collection pro forma were collated, coded and entered into the computer using statistical package for social science (SPSS) computer software version 22. The data were analyzed using the same statistical package for social science (SPSS) and the results presented in frequencies and tables.
In this study, packed cell volume (PCV) less than 30% was regarded as anaemia.26 Postoperative pyrexia was taken as temperature greater than 380C on any two consecutive days after hysterectomy or temperature of 390C on any postoperative day.27 Some patients had more than one complications arising from the surgery.
Results
Table 1: Distribution of patients by age and parity
Table 2: Route of hysterectomy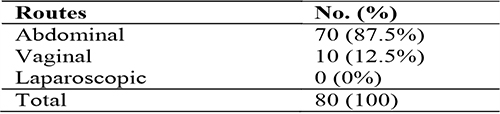
Table 3: Indications for hysterectomy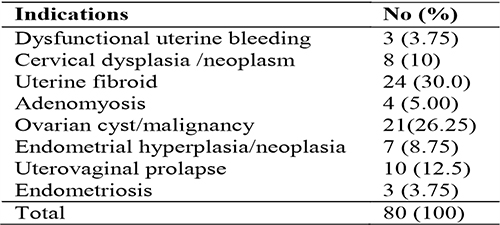
Table 4: Extent of hysterectomy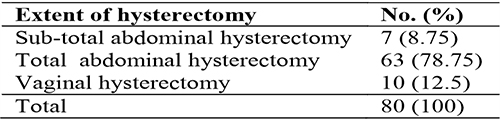
Table 5: Hysterectomy with salpingo-oophorectomy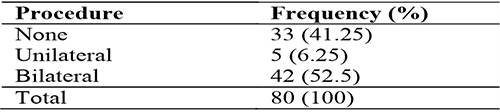
Table 6: Complications of hysterectomy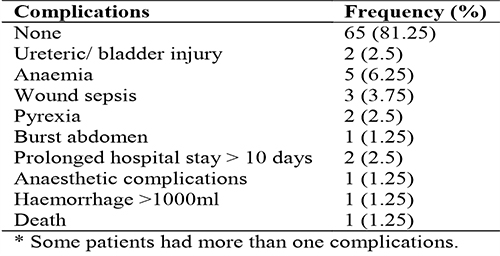
There were 468 major gynaecological surgeries during the five year period under review. Of these, 85 of them were hysterectomies, accounting for 18.2% of the major gynaecological procedures. Five case notes could not be retrieved for analysis. Eighty case notes were retrieved (giving a retrieval rate of 94.1%) and these formed the basis for further analysis.
Majority of the patients who had hysterectomy were aged 45 years and above. Majority of the patients (46.6%) were Para 5 and above (Table 1). There was one case of hysterectomy in a nulliparous woman (1.25%) due to recurrent multiple uterine fibroid and adenomyosis after two previous myomectomies. Most of the cases were through the abdominal route, accounting for 87.5% (Table 2). The rest of the cases were done through the vaginal route (12.5%) and these were due to utero-vaginal prolapse. There was no case of laparoscopic hysterectomy. Uterine fibroids accounted for 30.0% of the indications (Table 3). This was followed by ovarian pathology (26.25%) and utero-vaginal prolapse (12.5%). Three patients (3.75 %) had subtotal abdominal hysterectomy due to severe pelvic adhesions that posed challenges in performing total abdominal hysterectomy.
Over half of these patients (52.5%) had bilateral salpingo-oophorectomy while 6.25% had unilateral salpingo-oophorectomy during the course of hysterectomy (Table 5). Anaemia was the most common (6.25%) morbidity, followed by wound sepsis (3.75%) (Table 6). One of the cases (1.25%) resulted in mortality due to anaesthestic complication. The patient suffered cardiac arrest intra-operatively.
Discussion
Hysterectomy accounted for 18.2% of major gynaecological surgeries during the 5 years under review. This is similar to the figure reported by Anzaku in Jos University Teaching Hospital, Jos11 but higher than some studies in other centres in Nigeria with prevalence rate of between 5.1% and 12.8%, even in the same region of the country.6-10,12-15 This difference in the same region might be due to the different sample size and total number of gynaecological admissions and surgeries that were analyzed (131 and 236 in Central Hospitals, Benin and Warri respectively).9,10 Our centre has a lower patient load, being a referral centre. The incidence of hysterectomy in this study is, however, lower than figures reported by Okafor in Nnewi and in developed countries.4,17,20 The reasons for the higher figures are because of the small family size in developed countries, their higher literacy level and lesser influence of culture and myths on health decisions.2,4 The mean age was 47.9 ± 10.6 years and this bears a good relationship with figures obtained from similar studies.6-15 Majority of the women would have completed their family size at this age as most of them were grand-multiparous (Table 1).
The mean parity in this study was 3.2 ± 0.83. It is comparable to 3.79 ± 1.08 reported by Okhionkpamwonyi et al, who conducted their study in another centre in the same region,10 where religion, cultural belief and marriage are similar and inter-related. However, this is lower than 5.5 and 5.84 reported by Bukar and Omole-Ohonsi in Gombe and Kano States respectively.18,19 This could be due to the higher incidence of early marriage in their region. The mean parity in this study is higher than figures reported by researchers in developed countries.4,17 The usual practice in developed countries, where women cherish their freedom, is that after one or two children they opt for hysterectomy so that they are free to carry on with their normal activities without hindrance from menstruation.2
Uterine fibroid was the commonest indication for total abdominal hysterectomy. This is similar to findings by other workers both in developing and developed countries.4,6-15 This may be attributed to the fact that uterine fibroid is the most common tumour of the uterus.7 Majority of the patients (78.75%) had total abdominal hysterectomy while 12.5% and 8.75% had vaginal hysterectomy and sub-total abdominal hysterectomy respectively. This is comparable to the findings reported by Ahmed et al in Aminu Kanu University Teaching Hospital.14
Majority of the patients (52.5%) had hysterectomy with bilateral salpingo-oophorectomy. This is comparable to 54.24% and 53% reported by Okhionkpamwonyi et al and Abe et al respectively.9,10 However, it is higher than 13.3% reported by Okafor in Nnewi.20 Bilateral salpingo-oophorectomy was done in the peri-menopausal and post-menopausal patients to prevent having to do another surgery if an ovary left in situ became diseased. Patients who had unilateral salpingo-ophorectomy accounted for 6.25%. This was to prevent premature menopause which can be very distressing especially in the absence of easy access to natural conjugated equine oestrogens for hormone replacement therapy in many developing countries.21
Twelve patients had various degrees of complications from the surgery, giving a complication rate of 15%. This is lower than 21.2%, 33%, 45.15%, 26.9% and 44% reported by Okhionkpamwonyi, Daru, Geidam, Omole-Ohonsi and Verol et al respectively.10,19,22-24 Anaemia and wound sepsis/breakdown were the common morbidities; comparable to the findings reported by Kawuwa in University of Maiduguri Teaching Hospital.25
There was 1 mortality reported in this study giving a mortality rate of 1.25%. This is lower than 1.6% reported by Abe in Central Hospital, Benin City.9 This difference may be due to the lower number of cases analyzed in this study.
Conclusion
Hysterectomy is a common surgery worldwide with similar indications for the operation and it is a relatively safe procedure. Furthermore, laparoscopic approach to hysterectomy is a form of minimal access surgery that did not feature in this study because such service was not available in this centre at the time of review. This is because of the non-availability of the necessary equipment at the time of the study. It is hoped that post-operative morbidities will be reduced by this approach. Training and re-training of more gynaecologist in minimal access gynaecological surgeries as well as provision of necessary equipment would be a worthwhile venture.
References
- Awoleke JO. An Audit of Hysterectomy at the Lagos University Teaching Hospital, Lagos. Trop J ObstetGynaecol. 2012, 29(1): 96-102
- Arowojolu AO. Hysterectomy In: Okonofua F, Odunsi K, (eds). Contemporary Obstetrics and Gynecology for Developing Countries. Women and Action Research Centre, Benin City. 2003; 227-242.
- Radmila S, Gernot H, Milica B, Aleksandra G and Snezana B. Hysterectomy Throughout History. ACI/IZ Istorije Medicine. 2010; 58: 9-11.
- Vessey MP, Villard- Mackintosh L, McPherson K, Coulter A, Yeates D. The Epidemic of Hysterectomy: findings in a large cohort study. British J ObstetGynaecol. 1992; 99: 402-7.
- Hysterctomy: Women Reproductive Health; Department of Health and Human Services, CDC. 2011.
- Oyawoye OA. Elective Hysterectomy at Ilorin, Nigeria- 4 year review. J Obstet Gynaecol.1998; 18(1):72-5.
- Roberts OA, Okunlola MA. Abdominal Hysterectomy for Benign Gynaecological Conditions at Ibadan, Nigeria. Trop J ObstetGynaecol. 2001; 18(1):19-23.
- Onah HE, Ezegwui HV. Elective Abdominal Hysterectomy: Indications and Complications in Enugu, Eastern Nigeria. Global J Med. Sci.2002; 1(1):49-53
- Abe E, Omo-Aghoja L. A Decade of Hysterectomy in a Tertiary Hospital in Urban Niger-Delta Region of Nigeria. Niger J ClinPract. 2008; 11(4):359-63.
- Okhionkpamwonyi O and Okonta PI. Total Abdominal Hysterectomy at the Central Hospital, Warri: A Five Year Review. Borno Med J. 2015; 12(1): 23-9
- Anzaku AS and Musa J. Total Abdominal Hysterectomy for Benign Gynaecological Conditions at a University Teaching Hospital in Nigeria. Nig J Med. 2012; 21(3): 326-30.
- Obilah-Abhulimen, Ibrahim IA and Omoregie OB. Hysterectomy in the Niger Delta of Nigeria: A Clinical Study of Indications and Outcome. Greener J Med Sc. 2013; 3(5): 160-5.
- Iklaki CU, Njoku CO, Ekabua JE, Odusolu PO, Agan TU and Ekabua KJ. Restrictive Use of Vaginal Hysterectomy: Another Skill Disappearing? A Five Year Review at the University of Calabar Teaching Hospital, Calabar, Nigeria. JMMR. 2013; 1(1): 1-6.
- Ahmed ZD and Nafi’ah T. Indications and Outcomes of Gynaecological Hysterectomy at Aminu Kano Teaching Hospital, Kano: A 5-Year Review. Open J ObstetGynaecol. 2015; 5:293-304.
- Okogbenin SA, Eigbefoh JI, Okonta PI and Onuh SO. Abdominal Hysterectomy for Gynaecological Disease: Six Year Review in University of Benin Teaching Hospital. Trop J ObstetGynaecol. 2004; 21(1): 29-30.
- Omigbodun AO and Ayinde OA. Commentary: Novel Approaches to the treatment of Uterine Leiomyomata. Trop J. ObstetGynaecol. 2003; 20 (1):1 – 3.
- Jacoby VL, Autry A, Jacbson G. A Nationwide use of Laparoscopic hysterectomy compared with abdominal and vaginal approaches. Obstet. Gynecol. 2009; 114(5):1041-1048.
- Bukar M, Audu BM, YahayaUR.Hysterectomy for Benign Gynaecological Conditions at Gombe, North East Nigeria. Niger Med Jour. 2010; 51(1):35-38.
- Omole-Ohonsi A, Ashimi OA. Non-emergency hysterectomy: why aversion. Arch. Gynecol. Obstet. 2009; 280(6):953-9.
- Okafor CI, Nkanwa U, Nwankwo ME, Ezeigwu CO. A Review of Gynaecological Hysterectomies in a Private Specialist Hospital in Nigeria. Orient J. Med.2012;24(3-4);53-57.
- Ogedengbe OK. Uterine Fibroids. In: Contemporary Obstetrics and Gynaecology for developing countries. Ed F Okonufua and K Odunsi.2003; Women’s Health and Action Reseach Centre, Benin City. 2003; 202-13.
- Verol N et al. A ten-year review of hysterectomy morbidity and mortality: can we change direction. Aust. N. Z.Jour. Obstet Gynecol.2001;41(3):295-301.
- Duru PH, Pam IC, Gamba IO, Ekwempu CC, Kigbu JH, Mutihur JT. Indication for abdominal hysterectomy at Jos University Teaching Hospital. Highland Med Research Jour.2008; 6(1-2)
- Geidam DA, Bukar MB. Hysterectomy at the University of Maiduguri Teaching Hospital, Nigeria.Niger Med Jour.2010;19(4):467-70.
- Kawuwa MB, Mairiga AG and Audu BM. Indications and Complications of Hysterectomy in Maiduguri, Northern Nigeria. Kanem Jour of Med Sc. 2007;1(1):20-25.
- Abudu OO. Anaemia in pregnancy. In: Agboola A, editor. Textbook of obstetrics and gynaecology for medical students. Vol. 11. Nigeria: Heinemann; 2001. p. 77-89.
- Abdelmaseeh TA, Azmat CE, Oliver TI. Postoperative Fever. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482299/