Perception on Preparation for Transplantation and Medication Adherence: An Exploratory Study of Post Kidney Transplant Patients in Nigeria
Ajah C C1, Ogbo P U2, Akinola A A2
Abstract
Background: Many patients suffering from renal failure have embraced kidney transplant instead of dialysis despite huge financial implications. However, post kidney transplant patients (PKTPs) require strict adherence to immunosuppressant medications to prevent rejection of the allograft. Encounters during patients’ medication refill suggest information gaps about medication use burden.
Objectives: This study was set to explore PKTPs perspective on their preparation for transplant and determine possible information gaps during preparation for transplant.
Methods: This study was conducted by qualitative methods using in-depth interviews. Eighteen PKTPs were purposely recruited from their refill facility in Lagos and interviewed using an open-ended interview guide. The interviews were recorded, transcribed verbatim, coded, and analyzed using thematic analysis.
Findings: The main information received during preparation bordered mostly on expectation of improved quality of life, financial implication, and the need to maintain the new kidney using medications. While some respondents ambiguously stated that the team ‘did their best’ in preparing them for transplant, six respondents regretted not having information about the life-long use of medications until after the transplant. Some respondents totally adhered to their medications, never missing a dose; others missed some doses unintentionally while some others deliberately missed their doses just to save cost. All respondents’ experience of a better quality of life after transplant was as expected.
Conclusion: This study revealed that some respondents experienced information gaps concerning life-long use of medications post-transplant. The experience of very improved quality of life post-transplant seemed to be the driving force for medication adherence.
Keywords: Qualitative method, Post kidney transplant patients, Perception on preparation, Medication adherence
Introduction
Kidney disease has a major effect on global health both as a direct consequence of morbidity and mortality or as a risk factor to cardiovascular disease. The prevalence has increased over the years with as many as 1.2 million deaths from chronic kidney disease (CKD) in 2017 worldwide.1 The burden of CKD in some regions such as Sub-Saharan Africa, Latin America and Oceania is much higher than expected for the level of development.1 This indicates that these regions bear the brunt of kidney disease. With the inception of transplantation in the 1960s, death is averted but with enormous financial implication. The burden of CKD in Nigeria is high but variable.2 Since the start of transplantation in Nigeria, 201 transplants have been performed between 2000 and 2014 with many more done outside the country.3
Kidney transplantation seems to be the gold standard for the treatment of end stage renal disease (ESRD). While this treatment returns patients to near normal life with much improved quality of life, a study conducted in Ghana found factors such as fear of complications following transplant and financial constraints to be barriers to opting for transplantation by ESRD patients.4 The burden of treatment and care as well as financial implication post-transplant is enormous and could be a warning sign to non-adherence to the multilayered and dynamic concept of patient adherence involving lifestyle changes, laboratory visits and regular attendance at clinics. In addition, medication adherence involves strict adherence to the recommendation and instruction on taking the immunosuppressant medications. This therefore requires adherence to the prescribed dosage and times; and persistence to the duration and consistency with the specified behavior.5
In Nigeria, although the number of patients who undergo kidney transplant yearly is unavailable, there is clear evidence of kidney-transplant medical tourism to various developed countries of the world.6 The success of this procedure irrespective of the huge financial implication has encouraged ESRD patients and prospective kidney transplant patients to consider the procedure. Part of the burden of treatment on patients is the life-long use of anti-rejection medicines. While patients are happy to be off dialysis and have their lives back, concerns remain. A study done among post-transplant patients in Michigan, America found that although patients were grateful for the transplant, they had concerns about the burden it places on their loved ones, duration of graft survival, future health and cost and quality of healthcare.7 Another qualitative study done among 16 transplant patients attending the Mayo Clinic found three main themes on treatment burden: ‘work patients must do to care for their health, challenges and stressors that exacerbate felt burden and impacts of burden’.8 Adherence to medication use and lifestyle is key for kidney post-transplant patients because of the possibility of rejection of the graft. Studies have shown different levels of adherence among post-transplant patients ranging from 31% in India to 40% in Kuwait.9,10 A randomized control trial study done in Australia to improve adherence to medication among adult kidney transplant found that there was no difference in adherence between groups measured by Medication Event Monitoring System (MEMS) which detected a 40% adherence, with 42% underutilizing the tool despite training received.11 The study also found that based on the self-reported Basel Assessment of Adherence to Immunosuppressive Medication Scale (BAASIS) score, the percentage of adherent participants decreased significantly between baseline and 3 to 12 months in the control group (p<0.001), while the percentage of adherent participants in the intervention group remained constant over time. A study found that non-adherence shortly after kidney transplantation may be a risk factor for lower graft survival in the years to follow.12 Repeating a transplant due to rejection of graft has its own risks and other additional burdens. Therefore, it is important to explore the preparation of these patients for life post-transplant. This study was set to determine their perception of their preparation by the transplant team before the transplant and to determine if patients’ pre-transplant expectation matched their actual experience post-transplant. The study also sought to assess the adherence of patients to their medication and their coping mechanisms.
Methods
Study design: This was a qualitative study of post kidney transplant patients’ experiences before and after transplantation. A phenomenological approach was applied for the study to allow focus on the respondents’ perception of their preparation for transplantation and their lived experiences after transplantation. In-depth interview was conducted using a pretested, semi-structured, open-ended interview guide.13,14
Study setting: The study was conducted in one of the facilities in Lagos, Nigeria where patients refilled their medications after transplantation. Patients were recruited by the first author, as they came in for their monthly refill. The first author had many years of experience as a pharmacist, managing the facility and relating with the patients during their monthly refill. At the time of the study, the first author was undergoing a master’s program in Clinical Pharmacy, at the University of Lagos, Nigeria.
Participants: Eighteen post-transplant patients were purposely recruited. The eligibility criteria for the study were adults 21 years old and above with grafts more than six months and demonstration of literacy to comprehend and answer questions in English Language.
Data collection: Interviews were conducted by the first author at the refill facility. Each respondent was alone with the interviewer to ensure confidentiality and privacy. Respondents were asked open-ended questions to describe their experience living with kidney failure and their perception about their preparation for transplantation. Other questions include their expectation of life after transplant and if their experience post-transplant matched their expectation. Demographic information was collected during the interviews. Majority of the interviews lasted about ten minutes on the average. Interviews were recorded and transcribed verbatim. Interviews were conducted until thematic content was saturated at 18 respondents. Respondents were not compensated for participation.
Data Analysis: Thematic analysis was applied for this study. Transcripts were read and reread several times. The transcripts were then coded and sorted into themes and categories that answered the research questions. Sometimes the categories were moved from one theme to another because of the iterative nature of qualitative analysis until the analysis was completed. The COREQ guidelines were adapted for the reporting.
Ethical approval: This was obtained from the Health Research and Ethics Committee of the Lagos University Teaching Hospital (LUTH) with an assigned number. ADM/DCST/HREC/APP/3218. Respondents signed informed consent forms before the interview was conducted. The respondents were assured of confidentiality and so all interviews were coded at the point of transcribing.
Results
Table 1: Sociodemographic characteristics of participants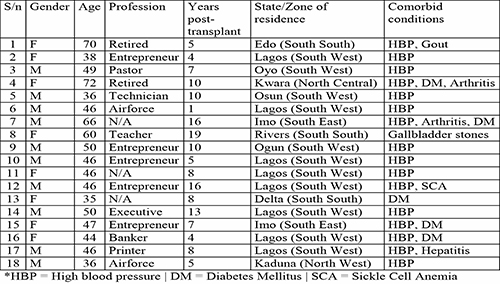
Table 2: Respondents' experiences living with kidney failure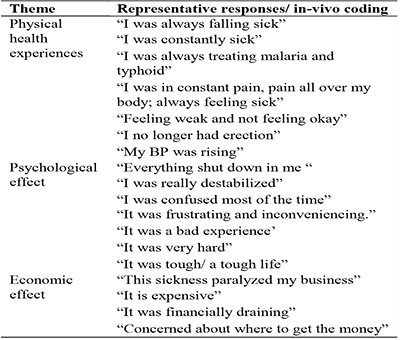
Table 3: Preparation for transplant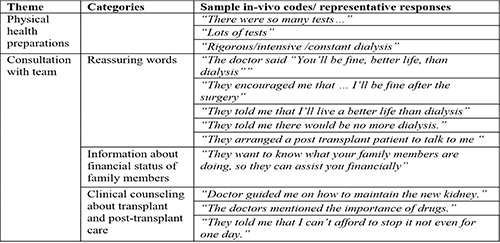
Table 4: Respondents' expectation of life after transplant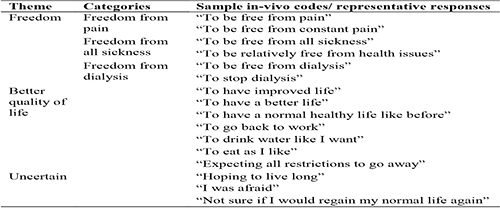
Table 5: Respondents experience since transplant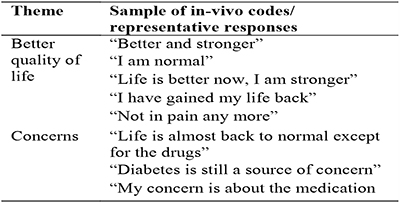
Sociodemographic characteristics of participants: The 18 participants in this study visited the refill facility from 10 of 36 states of the country represented by five geopolitical zones out of six. Eleven of the 18 participants resided in southwest Nigeria where the refill facility is located. There were 10 male and 8 ftemale participants. The age range was between 36 and 72 years with mean age being 49 years. Eleven patients were less than 10 years post-transplant, while 7 were 10-plus years post-transplant with a median of 7.5 years. Majority of the respondents were also taking medications for high blood pressure (Table 1).
Experiences living with kidney disease
In the first question, respondents were asked: “Describe your experience living with kidney failure before surgery”. Three themes emerged. Respondents experienced a threefold challenge of physical health, psychological effect and economic effect in concert. The answers to this question established their state of ill health pre-diagnosis, and post-diagnosis, as dialysis commenced. Having dialysis three times or more weekly escalated the burden in all three dimensions.
Preparation for transplant
In the second open-ended question, patients were asked: “How did the transplant team prepare you for transplant”? Respondents had common as well as diverse experiences with the different transplant teams. A common denominator for all respondents was the carrying out of so many tests for patient and donor, and frequent dialysis before transplant.
All patients described their path to transplantation with the medical team. They recounted the support they had from the team which bordered on tests for patient and donor, financial implication, and the need to care for new kidney with anti-rejection medications. One respondent said:
“There were so many different types of tests, blood tests, urine test and all. It was quite tedious for my children and me. It was also expensive. We had to get a donor, who was equally tested, severally, until the doctors were satisfied with the results.” (72 years old retired female, 10 years PT).
Some respondents understood the financial implication before the transplantation to run tests, for the transplantation itself and post-transplantation. However, six respondents claimed to be unaware of the life-long use of the medications which are quite expensive. Patients seemed to have received lots of empathy as the team assured them of a better quality of life after the transplantation and this brought hope alive for them.
Respondent’s expectation of life after transplant
Three themes emerged from the third open-ended question: “ What was your expectation of life after surgery?: freedom from pain, dialysis and sickness; better quality of life, and uncertainty about the outcome. Samples of codes are presented in table 4.
Freedom from all discomfort and improved quality of life: Respondents had great expectation of freedom from sickness, dialysis and pain, and earnest expectation that they would have improved and better quality of life depicted by ‘life as normal’. Their expectation was captured in the expression by one of the respondents who said:
“I was expecting all the restrictions to go away; like, don’t do this and that. Because they were telling me ‘don’t eat some certain foods like red meat and all that.’ I was also hoping to stop dialysis and go back to a normal healthy life. (50-year old executive; 13 months PT).
Uncertainty: Some respondents were uncertain of the outcome of the transplant. One of them said:
“Going by what I was hearing from some post transplant patients, I was afraid. They told me the operation is going to be painful and expensive to maintain after.“(46-year old businessman, 5 years PT).
Another said:
“I was hearing from some other patients about the Dos and Don’ts. I was really worried about this aspect; about some foods to avoid and that I cannot enjoy myself. I was somehow hoping that I would be able to make love after the surgery. I was really discouraged about this aspect. Some people even told me that I would need to be buying drugs of N2 million ($5,600) in 6 months. I was double minded, not sure if I will gain my life back.” (46-year old Air force personnel, 1 year PT).
Respondents experience since transplant:
From the fourth open-ended question, “What has been you experience since surgery”? two themes emerged: Better quality of life and concerns (Table 5).
Better quality of life: All the respondents expressed satisfaction to a large degree with only a few expressing concerns. Even those who had concerns before the surgery ended up experiencing better quality of life. One respondent who had concerns pre-transplant said:
“I did not feel any pain after the surgery. You won’t even know I did an operation, no pain until this moment. All the stories that some patients told me were not exactly true, like not having a normal life and eating what you want. I now eat anything.” (46-year old businessman, 5-years PT).
Another respondent who had concerns pre surgery said:
“My life is better now. I can now eat whatever I want; I am having erection. I have gained my life back; I am still running my business. They said I can’t drive till 6 months but I was driving in 3 months.” (46-year old Air force personnel, 1 year PT).
Concerns: Other respondents had unanticipated concerns after the surgery different from their expectations. One of them said:
“I had diabetes and hypertension before the operation. The blood pressure issue is controlled somehow with the drugs, but this diabetes of a thing and the instability is my major concern. I pass water very well, unlike before. The kidney is doing fine.” (66-year old man. 16 years PT).
All respondents but one indicated that their experience post-transplant was in tandem with their expectation.
Respondent’s retrospective view of their preparation for transplant
To the question, “Do you think that you were adequately prepared for the transplantation by the team”? Respondents gave ambiguous answers that unveiled dissatisfaction with their preparation for transplant.
Ambiguous expressions such as “they tried their best”, “the doctors did well”, “they tried”, were representative responses. However, a few respondents expressed their heart-felt opinion. One respondent said:
“I think they did well. Although it was after the surgery that they let me know that I will need the drugs for life. It was when I was in the ICU, before we were discharged. They told us everything then.” (47-year old business woman. 2 years PT).
Another said:
One thing I didn’t understand was this issue of drugs. I didn’t know it would persist for this long. My initial understanding was that I would use it, but not more than 6 months. I did not get that I will use it forever like this. (50-year old executive. 13 months PT).
Yet another respondent said:
”I was not given enough information about needing the drugs, until 3 days after my transplant! Nobody counseled me on that, specifically before the surgery. They also should have told me about my diet; they didn’t say anything about it. It was later another doctor told me to mind fried foods or anything that will increase my cholesterol.” (46-year old businessman. 16 years PT).
One respondent who was 8 years post transplant said:
At first I did not know that I would use the drug for long like this. I wish I had understood them very well (46-year old female. 8 years PT).
Use of medication
With regards to medication use and how to maintain the new kidney, respondents had this to say:
The doctor said I must take my medications regularly without fail (Respondent 5, 36-year-old male technician; 10 years post-transplant).
The doctors mentioned the importance of the drugs; that I can’t afford to stop not even for one day (Respondent 13, 35-year-old businesswoman; 8 years post-transplant).
They told me that the medications are very important after surgery, that my survival depends on the medications and that they would be for the rest of my life (Respondent 18, 36-year-old male Airforce officer, 5 years post-transplant).
Adherence to medications post-transplant
There were three categories: totally adherent, partially adherent (unintentionally missed some doses) and nonadherent (intentionally missing some doses to save cost). Some respondents emphatically said they never miss any dose, and they do everything possible to ensure adherence.
Others have unintentionally missed some doses.
“I sometimes miss them but not deliberately”; “I don’t miss them intentionally, I get tired of taking them”; “yes, sometimes I just forget. I miss more in the evenings when I fall asleep; I take it as soon as I remember”.
Others indicated that they deliberately miss their dose to save cost.
“I miss the dose just to manage it; I have terrible experiences when I miss the dose; I feel it and I know it is not a good sign” (Respondent 5, 36-year-old male technician; 10 years post-transplant).
No, I don’t, but I missed for one week because of money (Respondent 11, 46-year-old female, 7 years post-transplant).
I have missed severally, majorly because of finance (Respondent 12, 46-year-old male entrepreneur, 16 years post-transplant).
Additional findings
Expectation and experience after transplantation: All patients expected and experienced a better life free from sickness and dialysis. Respondents expected the ability to return to their normal life and resume work as usual and this was a dream come true. Six patients expected to be free from medications but that was not the case. Respondent 11 said, “I was expecting to be free from all drugs”. Respondent 17 echoed, “I was not expecting to be on drugs for this long”.
Patients’ opinion about cost of management/support: All patients reported that the whole process (before, during and after transplantation) is a very expensive venture, and so they were unable to cope with the financial implications. Hence, many respondents received financial support from family, friends, church, NGOs or from their workplaces. Only two respondents indicated that they had no financial support from anywhere or from anyone.
Satisfaction with the outcome of transplantation: All respondents reported that they were very much satisfied with the outcome of the transplantation and returned to their normal life. Respondent 15 said, “I am very much satisfied. I am now living a normal life, no more dialysis; I feel better, drink water as I like, eat well now; gone back to business”
Appointment with Nephrologist: A few respondents were able to keep their appointments as scheduled, while others do so when they have the finances to cover the cost or when they feel unwell.
One respondent said “I didn’t see him (nephrologist) throughout last year; Just busy with life. I feel well. The money is also a concern” (Respondent 9, 50-year-old male entrepreneur - 10 years post-transplant)
Another respondent said, “It is over a year I saw my nephrologist. I take myself as if I am normal. I am required to do all kinds of tests, both relevant and not relevant. I cannot afford it” (Respondent 10, 46-year-old entrepreneur, 5 years post-transplant).
Coping mechanisms to ensure adherence to medications: Respondents reported that they had to be self-disciplined to remember to take their medications. Others set alarms on their cell phones as additional source to enhance adherence while some others have family members who ensured that they adhered to their medications.
Discussion
This study has explored patients’ experiences and perspectives on their preparation for transplant and life after transplant. Our respondents shared their experiences of ill health and very poor quality of life before they made the decision for transplant, and their journey of wellness after transplant.
Preparation of patients for transplant is key to successful transplantation and life after transplant.15 Our respondents indicated clearly that they and their donors carried out lots of tests as part of the preparation even though they did not indicate the specific tests. These tests would include cardiovascular investigations, exclusion of bacterial and viral infections, immunological investigations, and compatibility of donor kidney with recipient amongst others.16 While these tests are imperative, they add to the financial burden of kidney transplantation right from the onset especially in a society like Nigeria where payment for healthcare is majorly out-of-pocket. Hence, the preparation team usually explained the financial involvement before, during, and after transplantation. These explanations help patients to understand their choice of kidney transplant. Other categories of preparation include pharmacotherapy, the need for life-long use of antirejection medications and psychological aspects. The counseling that patients would have a better life was notable in our study. This infused hope and positive prospects of life post-transplant. Our respondents reported better quality of life and noted that their experience of life after transplant met their expectations. A study carried out among 18 kidney patients to share their experiences before, during, and after transplant showed that although patients were enthusiastic to go home after the transplant, they were faced with the challenge of life transplant had; the challenges of balancing life in terms of hope, positive prospects, and health-related challenges.17 Our respondents were grateful that their lives have been restored and so found ways to cope with other everyday challenges.
Our study respondents had varying perceptions about their preparation for transplant. While many ambiguously reported that the team did their best, six respondents reported that they were not adequately prepared as they regretted making the decision of transplantation without enough information especially of the life-long use of medications. In the words of one such respondent, “The fact still remains that a proper orientation of the patient will help them manage the condition”. The outcome and success of transplantation lies in proper preparation of the patients.15
Our study showed that many respondents adhered religiously to their medication in terms of adherence and persistence.18 Factors that influenced such strict adherence were the desire to remain well and not experience rejection of graft. Some respondents reported that they intentionally missed their doses to save cost even though they were aware of the consequences. Healthcare professionals in South Africa, in a survey about their perception about self-management of kidney transplant patients identified non-adherence as a barrier to successful grafts.19 Other authors also found that nonadherence shortly after kidney transplantation may be a risk factor for lower graft survival in the years to follow.12 A quantitative cross-sectional study conducted in Indonesia found that the majority (79.1%) of their respondents adhered to their medication.19 In contrast, a study conducted among kidney transplant patients in Kuwait to find out the compliance to medication and lifestyle changes found that only 60% of the respondents adhered to their medication.10 Risk factors to noncompliance in the study were being female and having unrelated living donors. Adherence to medication post-transplant is non-negotiable as the consequences may be rejection of the grafted kidney which could lead to another transplantation as experienced by one of our respondents who was on her second graft. The main factor that influenced nonadherence in our study was cost because most healthcare costs in Nigeria are out-of-pocket. Many of the respondents were being supported financially by family, friends, church, workplaces, and some non-governmental organizations. The study revealed the connectedness with family and friends in Nigeria. The main factor that influenced partial adherence among our respondents was forgetfulness. This finding is like the study conducted in Indonesia where respondents who were not compliant to their medication reported that they forgot.19 The commonest way our respondents managed this was developing self-discipline followed by cellular phone alarms as a reminder. Some reported that close family members also reminded them daily to take their medications. This corroborates with findings from a study where post-transplant kidney patients used reminder methods and problem-solving abilities just to ensure adherence.20
All patients in our study experienced better life and health as promised by the healthcare team and as expected by the patients. Their experience of better and healthier lives seemed to be the motivation for adhering to medication rather than the information given to them on the life-long use of the medications, especially because some respondents were not told about it. Respondent 5 reported that she notices the difference anytime she skipped her medication and according to her, “it was not a good sign”. This corroborates with another study where respondents who were not compliant with their medications experienced low quality of life.19
This study also found nonadherence to other components of post transplantation. Respondents kept to their appointments after the transplantation but reduced the frequency of appointments with increasing graft survival. These appointments consist of consultations with nephrologist and laboratory tests which have huge financial implications. Hence majority of our respondents kept their appointments only when they were able or when not feeling well.
Overall, our respondents were very satisfied with their transplantation because they evidently felt well and had returned to normal life. Some respondents still regretted not having information on the life-long use of the medications before the transplantation.
Limitation of the study: This study was limited to patients who refilled their medications at the refill facility in Lagos, Nigeria. Furthermore, being a qualitative study, the findings are not necessarily applicable to all post kidney transplant patients.
Conclusion
This study revealed that our respondents had varying experiences during preparation for kidney transplantation. Some respondents experienced information gaps concerning the life-long use of medications post-transplant. The experience of very improved quality of life post-transplant seemed to be the driving force to achieve adherence rather than the information given about life-long use of medications during their transplant preparation. The huge financial burden was a main factor for nonadherence. This study shows the need for all transplant teams to work with a checklist of information for patients’ preparation for transplant to ensure that all patients have complete information.
References
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990 – 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–733. DOI https://doi.org/10.1016/S0140-6736(20)30045-3
- Chukwuonye II, Ogah OS, Anyabolu EN Ohagwu KA, Nwabuko OC, Onwuchekwa U, et al. Prevalence of chronic kidney disease in Nigeria: systematic review of population-based studies. Int J Nephrol Renovasc Dis. 2018;11 165–172 DOI https://doi.org/10.2147/IJNRD.S162230
- Ulasi II, Ijoma CK. Organ transplantation in Nigeria. Transplantation. 2016:100(4): 695-697 DOI https://doi.org/10.1097/TP.0000000000001149
- Boima V, Amissah-Arthur MB, Yorke E. Dey D, Fiagbe D, Yawson AE, et al. Determinants of willingness to accept kidney transplantation among chronic kidney disease patients in Ghana. BMC Nephrol. 2021; 22:129 DOI https://doi.org/10.1186/s12882-021-02335-9
- Nevins TE, Nickerson PW, Dew MA. Understanding medication nonadherence after kidney transplant. J. Am Soc Nephrol. 2017;28(8):2290-2301 DOI https://doi.org/10.1681/ASN.2017020216
- Liman HM, Makusidi MA, Sakajiki AM. Kidney transplant-related medical tourism in patients with end-stage renal disease: A report from a renal center in a developing nation. Sahel Med J. 2020;23(1):7-11. DOI https://doi.org/10.4103/smj_17_19
- Tucker EL, Smith AR, Daskin MS, Schapiro H, Cottrell SM, Gendron ES, et al. Life and expectations post-kidney transplant: A qualitative analysis of patient responses. BMC Nephrol. 2019:20:175 DOI https://doi.ord/10.1186/s12882-019-1368-0
- Lorenz EC, Egginton JS, Stegail MD, Cheville AL, Heilman RL, Nair SS, et al. Patient experience after kidney transplant: a conceptual framework of treatment burden’, JPRO. 2019;3(8) DOI https://doi:10.1186/s41687-019-0095-4.
- Adhikari UR, Taraphder A, Hazra A, Das T. Medication adherence in kidney transplant recipients in an urban Indian setting. Indian J Nephrol. 2017;27(4):294–300. DOI https://doi:10.4103/0971-4065.202835.
- Kenawy AS, Gheith O, Al-Otaibi T, Othman N, Atya HA, Al-Otaibi M, et al. Medication compliance and lifestyle adherence in renal transplant recipients in Kuwait. Patient Prefer Adher. 2019;(3):1477-1486. DOI https://doi.org/10.2147/PPA.S209212
- Low JK, Manias E, Crawford K, et al. Improving medication adherence in adult kidney transplantation (IMAKT): A pilot randomized controlled trial. Sci. Rep. 2019;(9):7734 DOI https://doi:10.1038/s41598-019-44002-y
- Tielen M. Exel J, Laging M, Walker R, Mulley WR. Toussaint ND, et al. Attitudes to medication after kidney transplantation and their association with medication adherence and graft survival : a 2-year follow-up study. J Transplant. 2014; DOI https://doi.org/10.1155/2014/675301
- Creswell JW. Research design. SAGE. 4th edn. Thousand Oaks, California; 2014
- Morse JM. Determining sample size. Qual. Health Res. 2000;10(1):3–5. DOI https://doi:10.1177/104973200129118183 .
- Hwang Y, Kim M, Min K (2021) Factors associated with health-related quality of life in kidney transplant recipients in Korea. PLoS ONE 16(3): e0247934 DOI https://doi.org/10.1371/journal.pone.0247934
- Zeier M. Ritz E. Preparation of the dialysis patient for transplantation. Nephrol. Dial. Transplant. 2002:17(4):552–556. DOI https://doi.org/10.1093/ndt/174.552
- Nielsen C, Clemenson J, Bistrup C, Aggerskov H. Balancing everyday life — Patients’ experiences before, during and four months after kidney transplantation. Nurs Open 2019;6(2):443–452 DOI https://doi:10.1002/nop2.225.
- Ndemera H, Bhengu B. Perceptions of healthcare professionals regarding self-management by kidney transplant recipients in South Africa: A qualitative study. Int. J. Africa Nurs. Sci. 2018;9 120-128 DOI https://doi.org/10.1016/j.ijans.2018.10.003
- Megawati, Yetti K, Sukmarini L. The factors affecting the quality of life of kidney transplantation patients at the Cipto Mangunkusumo General Hospital in Jakarta, Indonesia. Enferm. Clin. 2019;29(S2):428-433 DOI https://doi.org/10.1016/j.enfeli.2019.04.063
- Ruppar TM, Russell CL. Medication adherence in successful kidney transplant recipients. Prog. Transplant. 2009;19(2):167-172.