Prevalence of dry eye disease among visual display terminal office users in Uyo, Nigeria
Abraham E G1, Motilewa O O2, Itina E I1
Abstract
Context: Dry eye disease (DED) results from loss of tear film homeostasis. Increase use of visual display terminals (VDT) by individuals and professionals increases the risk of DED.
Objective: This study is aimed to determine the prevalence of dry eye disease among office workers who use visual display terminals in Uyo.
Methods: A descriptive, cross-sectional study of VDT office workers aged 19-65 years. Multi-stage sampling technique was used to recruit participants. Self-administered Impact of Dry Eye on Everyday Life (IDEEL) questionnaire and ocular examination was done to gather data; such data was analyzed using SPSS version 22.0
Results: Prevalence of dry eye disease (DED) was 5.8% (95% CI 3.44 - 8.16). Mean Schirmer’s 1 was 21.60 ± 9.29mm, mean TBUT was 9.74 ± 2.48s, mean IDEEL score was 76.15 ± 25.47. There was a statistically significant association between DED and educational level 7.56(p-value 0.02), hours of visual display terminal use per day 10.72(p-value 0.013), and use of air conditioning 7.66(p-value 0.006). Multivariate regression analysis to identify predictors of dry eye was statistically significant for module 1(Symptom bother) of the dry eye questionnaire (p-value 0.01, odds ratio 12.71,), tear break up time in the left eye (p-value 0.00, odds ratio 38.67), and Schirmer 1 test in the right eye (p-value 0.00, odds ratio 30.83)`.
Conclusion: The prevalence of DED increases with the number of hours spent on VDT Periodic medical and psychological evaluation of VDT users to identify office workers most at risk should be carried out by employers of labour.
Keywords: Dry eye disease, Prevalence, Visual display terminal workers
Introduction
Tear makes up an important part of the ocular surface. It aids in lubrication of the cornea and conjunctiva to provide ocular surface comfort and provide oxygen to the superficial layers of the cornea. Together with the cornea, it makes up the major refractive surface of the eye and provides both mechanical and humoral protection to the eye.1,2 The cornea, conjunctiva, lids, tear forming glands and the nerves connecting them make up the lacrimal functional unit (LFU).3 The lacrimal functional unit is important in tear secretion and maintenance of normal ocular surface homeostasis.3 Disruption of the normal homeostasis is what causes Dry Eye Disease (ED).1 An unstable tear film is unable to maintain the normal functioning of the ocular surface leading to a cycle of ocular surface inflammation with resulting pain.
Dry eye disease is a multifactorial disease of the tears and ocular surface resulting in symptoms of visual disturbance, ocular discomfort, tear film instability with potential damage to the ocular surface. It is associated with hyperosmolarity of the tear film and sub-acute inflammation of the ocular surface (DEWS Ocul Surf 2007)4. Any of the structures including the cornea, conjunctiva, the main or accessory lacrimal glands or the meibomian glands may be affected in dry eye disease. Dry Eye Disease (DED) is classified broadly into two main groups, the aqueous deficient dry eye disease and the evaporative dry eye disease. This classification is not mutually exclusive, since dry eye disease is chronic and no matter the etiological factor, features of both reduced tear quality and quantity may be seen.1
Visual display terminal (computer display) is a computer output surface and a projecting mechanism that shows texts and images to the computer user and includes the screen and the device that gives information to the screen.5 These visual display terminals include personal computers (desktops), laptops, tablets and smartphones.6 Persons who use visual display terminals typically develop evaporative dry eye (EDE) caused by reduced blinking, increased palpebral fissure height which encourages tear evaporation and working in cool dry environments with low relative humidity.1
The prevalence of Dry Eye Disease according to a meta-analysis by the Tear Film and Ocular Surface Society’s Dry Eye Workshop11 (TFOS DEWS II)1 on population studies reported a world-wide prevalence of 5-50% based on symptoms with or without signs but when only signs were taken into account, the prevalence went up to 75%. Females were noted to have a higher prevalence of dry eye disease than males and this was said to increase with each passing decade. East Asians were also reported to have a higher prevalence compared to the rest of the world.7 In Ghana, a 2018 study among undergraduates by Asiedu et al reported a prevalence of 44.3%;8 while in Nigeria, population-based studies had prevalence ranging from 23.7% to 32.5%.9,10 The prevalence of dry eye disease among visual display terminal users worldwide is 49.5% (with a range of 9.5-87.5%), the wide margin was due to different criteria for diagnosis of dry eye disease(usually based on a questionnaire for the symptoms, and tests for tear film abnormality and assessment of ocular surface damage for the signs.), different work environment, different population and different age groups.11 Many studies used combined criteria for diagnosis.12,13,14 A group of out- patient attendees who presented with non-specific symptoms suggestive of dry eye disease which according to them did not allow them to concentrate at work were noted to be younger than the people who usually present with DED. It was also found that these patients were using visual display terminals for long periods of time at their workplaces. There was need to determine the relationship between the use of VDT and the DED symptoms and the prevalence of DED among VDT office workers in Uyo, Nigeria hence this study as there is no record of earlier study carried in Uyo, Akwa Ibom State.
Methods
The study was carried out in Uyo the capital of Akwa Ibom state. The state is one of the oil rich states in the southern part of the country. Uyo has a projected population of 1,200,000 and majority of the people are civil servants.15
This was a population-based, descriptive, cross sectional study evaluating tear breakup time (TBUT), Schirmer 1 test in people working with visual display terminals in offices in Uyo. The study was carried out over a three-month period. Multi-stage sampling technique was used to recruit participants for this study. A major landmark in Uyo; Ibom Plaza was chosen. Ibom plaza is a roundabout in Uyo with four major roads terminating there; Abak/Aka road, Ikot Ekpene road, Oron road and Wellington Bassey way (Barracks road). These roads divide Uyo into four parts. A simple random sampling was carried out to select Wellington Bassey and Oron roads. Cluster sampling was done at the next stage. The area between Wellington Bassey way and Oron road was divided into ten clusters. Each cluster containing 30 buildings. Balloting was then used to select four clusters in order to achieve the sample size. Office buildings within the selected clusters with at least three people using computers were recruited and permission was sought. Eligibility criteria included participants who have worked on a visual terminal device for at least six months and at least two hours or more per day and have not used topical medication for at least two months before commencement of the study. Exclusion criteria were persons younger than 18 years or older than 65 years, known diabetic, anyone with gross lid abnormality or have done eye surgery in the last six months, those on topical medication, contact lens or oral antihistamines
Data collection was done with use of self- administered IDEEL questionnaire, ocular examination was done during which Schirmer 1 test and tear break up time (TBUT) were performed. Random blood sugar was also carried out. Indoor temperature and relative humidity were measured using a combined digital thermometer and hygrometer. Outdoor temperature and relative humidity readings were taken using online accuweather.com. This was done by checking the temperature and relative humidity of Uyo at this website each day (between 9-11am) samples were taken, then finding the average at the end of every month.
Diagnosis of Dry Eye Disease was made by combining the positive test results.13 DED was diagnosed by the presence of IDEEL questionnaire’s Module 1 of greater than ≥40, Schirmer 1 test of <10mm, and tear break up time (TBUT) <10s. Respondents with only one or two criteria were classified as normal. Both eyes for each participant were tested. All data generated was entered into a pro-forma and data analysis was done using the Statistical Package for Social Sciences (SPSS, Inc., Chicago, Illinois) for Windows version 22.0 with the aid of a statistician. Continuous variables were summarized using measures of central tendency and appropriate measures of dispersion, categorical variables were summarized using proportion. F- test was used to determine association across the means and chi square test for categorical variables at 5% level of significance. Results were presented in tables and charts.
Ethical approval was obtained from the Institutional Health Research Committee of the University of Uyo Teaching Hospital (UUTH/AD/S/96/VOL.XX/163). Permission letters were written to the management of various offices in the city. Written informed consent was obtained from all the participants and the study adhered to the Helsinki Declaration on studies involving human subjects.
Results
Table 1: Social demographics of study participants
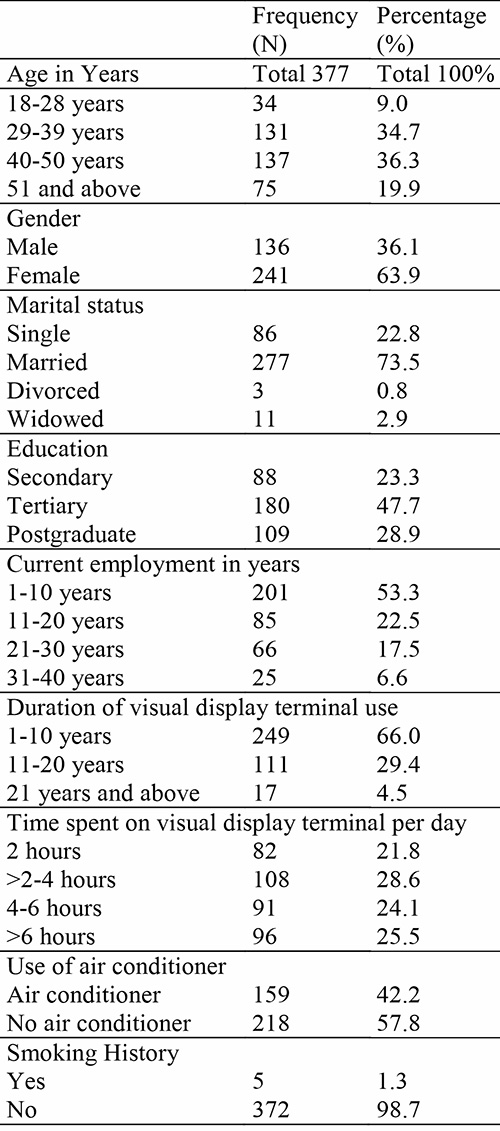
A total of 377 participants who met the inclusion criteria participated in the study. The response rate was 100% and total number of eyes examined was 754. The mean age of participants was 41.55 ± 9.66 years with a range of 19 to 65 years, median of 41 years.
Table 1 shows that of the 377 participants, 136(36.1%) were male and 241(63.9%) were female, giving a male to female ratio of 1:1.8 (Table 1). Most participants had tertiary (n=180; 47.7%) and post graduate education (n= 109; 28.9%). Most of the participants were married (n= 277; 73.5%), while divorced persons (n=3; 0.8%) made up the least number. Table 1 also shows that most people had worked at their current employment for at least 10 years (201; 53.3%) while the least number (n=25;6.6%) of persons had worked for over 30 years.
Table 1 also shows that most participants had used visual display terminals (VDT) for at least 20 years (n=360; 95.5%). Regarding the number of hours spent per day using VDT, most participants spent 4 hours or less per day (n=190; 50.4%); this is closely followed by persons who spent more than 4 hours a day using the VDT (n=187; 49.6%). Most of the participants (n=218;57.8%) did not use air-conditioners in their offices.
Table 2: Average relative humidity and temperature during sample collection
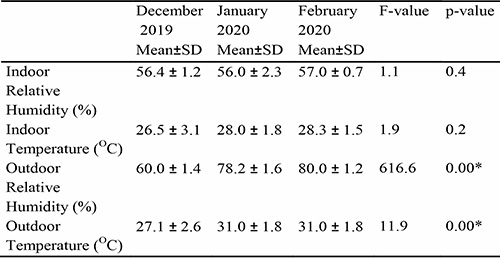
Table 2 shows the average relative humidity and temperature during the study period. The indoor relative humidity and temperature was based on the room allocated to the research team. December 2019 had recorded the lowest values with an average relative humidity indoors of 56.4 ± 1.2%, indoor temperature of 26.5 ± 3.10C and 60 ± 1.4% relative humidity and 27.1 ± 2.60C outdoors. Indoor and outdoor average temperatures were the same in January and February 2020. There was a statistically significant difference (F-ratio 616.6; p-value 0.00) between outdoor temperature in December (27.1 ± 2.60C), January and February (31.0 ± 1.80C). There was also a statistically significant difference (F-ratio 11.9; p-value 0.00) between relative humidity in December (60.0 ± 1.4%), January (78.2 ± 1.6%) and February (80.0 ± 1.2%)
Normal Schirmer I test was seen in 654 eyes (86.7%) abnormal Schirmer 1 test was seen in 77 eyes (10.2%), while severe Schirmer 1 test was seen in 23 eyes (3.1%). Mean Schirmer 1 test value for all eyes was 21.60 ± 9.3mm.
Table 3: Bivariate analysis of dry eye disease and social demographics and exposure to VDT
among the respondents
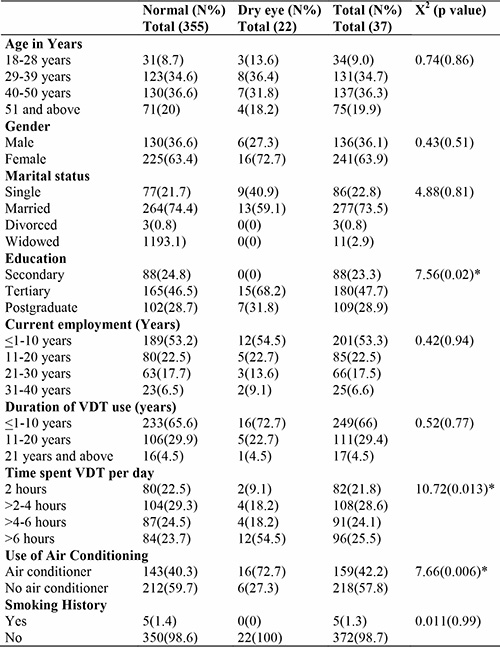
Table 3 shows the bivariate analysis of possible association between dry eye disease and social demographics of study participants. The following variables - education 7.56(p-value 0.02), time spent on a VDT per day 10.72(p-value 0.013), and the use of air conditioning 7.66(p-value 0.006) were found to be significantly associated with DED.
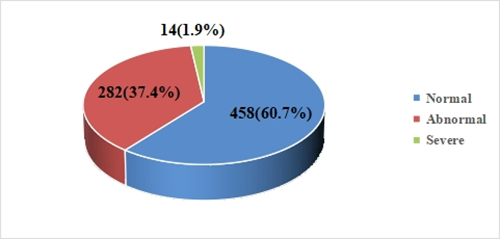
Figure 1: Tear breakup time (TBUT) for all eyes.
Most study participants had normal TBUT (n=458;60.7%). The mean TBUT for all eyes was 9.74±2.5s.
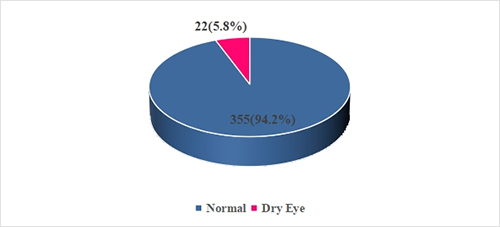
Figure 2: Prevalence of dry eye disease.
Figure 2 shows that 22 participants had dry eye disease giving a prevalence of 5.8% (95% CI 3.44 – 8.16).
Discussion
The prevalence of dry eye disease among VDT users in this study was 5.8%. Prevalence of DED in the general population vary from region to region with lowest in North America, 4.6% and the highest Eastern Asia the highest, 42.8%.16 Onwubiko et al17 in Enugu, Nigeria, who used similar test values had a prevalence of 19.2% among VDT workers compared to 5.8% in this study, the differences being that this study used the IDEEL questionnaire and it was a population-based study. Onwubiko et al17 used the OSDI questionnaire and theirs was a hospital-based study. Olaniyan et al13 in Ibadan, Nigeria, reported a prevalence of 32.5%; this study was however conducted in persons who were 40 years or older. Onua et al9 in Rivers State, used only Schirmer 1 test and had a prevalence of 27.4%. Outside the different test parameters, above mentioned Nigerian studies also used three different cut-off values for Schirmer 1 test. Onwubiko et al17 similar to this study, used <10mm, Olaniyan et al13 used ≤5mm, and Onua et al9 used <15mm. These differences, in addition to the different parameters used could also account for the different prevalence values obtained in these studies. Asiedu et al8 in Ghana assessed undergraduate university students between 18-34 years, and reported a prevalence of 44.3%. In contrast to the present study, that study used two (OSDI and SPEED) questionnaires as the basis of dry eye diagnosis. This may account for the higher prevalence of dry eye disease compared to this study. In other parts of Africa, Mostafa et al18 in Egypt had a prevalence of 22.8%, They used only the worse eye for each test and also used Schirmer 2 test (with anaesthesia) which was in contrast to this study and previous studies in Nigeria. Similar to Mostafa et al18, Castelyn et al19 in South Africa used Schirmer 2 test instead of Schirmer 1 test used in their study. This may be because the two previous African studies wanted to test only basal tear production and not total tear production like in the present study. Kluizenaar et al20 in a study done in about eight European countries had a prevalence of dry eye disease in office workers of 21.5-39.5%. These earlier studies all have a prevalence rate higher than this present study and may be due to different criteria for dry eye diagnosis and/or to the age of the participants. Hikichi et al21 in Japan had a prevalence of 17% and used double vital staining, tear breakup time, basal tear secretion and tear clearance as tests to diagnose dry eye. Many Japanese studies used a Japanese criteria system for diagnosis of dry eye disease: if two out of three criteria were met, probable dry eye disease was diagnosed and if three out of three criteria were met, then definite dry eye disease was diagnosed.6,22-25 This is in contrast to Nigeria where there is no uniform criteria for diagnosis of dry eye disease.9,13,16 This situation is however similar to what occurs in other parts of the world and it is one of the reasons why there is no gold standard in the criteria for diagnosis of dry eye disease.26
This study found no association between age and dry eye disease (p = 0.86), which was similar to results by Kolawole et al27 in Osun state, Nigeria, Hashemi et al28 in Iran and Bukhari et al29 in Saudi Arabia. This is however, in contrast to other dry eye disease studies.7-9,13,14 This result may have been because most of the participants were younger than 50 years, while those in other studies were 50 years or older. Mostafa et al18 in Egypt even reported that the prevalence of dry eye disease in those 45 years and older was more than those younger than 45 years.
There was no statistically significant association between dry eye disease and smoking in this study (p = 0.99), similar to Moss et al30 in the USA who found no association between dry eye disease and smoking. The probable reason for the result in this study could be because smokers only made up 1.3% (n = 5) of the study population thus making no impact on the study population. However, Lee et al31 in Indonesia and Bukhari et al28 in Saudi Arabia found an association between dry eye and smoking.
This study found a statistically significant association between dry eye disease and the time spent on the visual display terminal per day (p=0.013). This study used two hours as the minimum accepted amount of time spent per day, and a maximum of over six hours. Kojima et al32 in Japan found that visual display workers who used visual display terminals for four or more hours had reduced tear meniscus height, significant dry eye disease and visual symptoms. Patil et al33 in India found that increased duration of computer use was associated with an increased risk of dry eye disease.
There was no statistically significant association between duration in years of visual display terminal use and dry eye disease; this was in contrast to Akkaya et al34 in Turkey who found that increased duration of visual display terminal use was associated with an increased risk of dry eye disease. This may be the case because many Nigerians only began using visual display terminals about two decades ago with the introduction of the internet,35 while developed countries have been using visual display terminals for a much longer time.
Conclusion
The prevalence of DED increases with the number of hours spent on VDT but has no gender preference. Workers who use visual display terminals (VDTs) for more than 4 hours, had better education and work with air conditioning were found to have a higher risk of dry eye disease. This study did not however show that dry eye disease was associated with the duration of VDT use in years. It is recommended that regular eye healthcare consultations should be enforced by any office or department where there is intense use of VDT. Mandatory periodic medical and psychological evaluation at offices to identify workers most at risk in order to boost productivity by employers is advocated. The use of humidifiers by offices using air conditioning to improve relative humidity, screen glare filters and other ergonomic practices is also advocated.
References
- Craig, J.P., Nichols, K.K., Akpek EK, Caffery B, Dua ,H.S., Joo, C.K., Lui,Z., Nelson, J.D., Nichols J.J., Tsubota, K.and Stapleton F.TFOS DEWS II Definition and classification report. Ocular Surface (`2017); 15(3):267-283.`
- Willcox, M.D.P., Argüeso, P., Georgiev, G.A., Holopainen, J.M., Laurie, G.W., Millar, T.J., et al. TFOS DEWS II Tear Film Report. Ocular Surface (2017);15(3):366-403. doi: 10.1016/j.jtos.2017.03.006. Epub 2017 Jul 20.PMID: 28736338.
- Zhang, X., Zhao, L., Deng, S., Sun, X. and Wang N. Dry eye syndrome in patients with diabetes mellitus: Prevalence, etiology, and clinical characteristics. Journal Ophthalmol .(2016); 2016:8201053. doi: 10.1155/2016/8201053.
- 2007 Report of the International Dry Eye WorkShop (DEWS). The Ocular Surface; April :5(2) 67-202
- Rouse M. VDT (video display terminal, visual display terminal). techtarget. 2011 [Accessed 20th August 2019]. Available from: https://whatis.techtarget.com
- Nakamura, S., Kinoshita, S., Yokoi, N., Ogawa, Y., Shibuya, M., Nakashima, H., et al. (2010). Lacrimal hypofunction as a new mechanism of dry eye in visual display terminal users. PloS one, 5(6), e11119. https://doi.org/10.1371/journal.pone.0011119
- Stapleton, F., Alves, M., Bunya, V.Y., Jalbert, I., Lekhanont, K., Malet F, et al. (2017). TFOS DEWS II Epidemiology report. Ocul Surf;15(3):334-365.
- Asiedu, K., Kyei, S., Boampong, F, Ocansey, S. Symptomatic dry eye and its associated factors: A study of university undergraduate students in Ghana. Eye Contact Lens(2017); 43(4):262–266.
- Onua, A.A, Chukwuka, I.O. Prevalence of dry eye disease in a rural Niger delta community, Southern Nigeria. Open J Ophthalmol(2017);7(2):95–102.
- Abraham, E.G. and Megbelayin, E.O. Pattern of eye diseases among participants of free eye screening program in Uyo, Akwa Ibom State, Nigeria. Int J Community Med Public Health (2017); 4(3):657-661.
- Courtin,R., Pereira, B., Naughton,G., Chamoux, A., Chiambaretta, F. Lanhers, C et al. Prevalence of dry eye disease in visual display terminal workers: a systematic review and meta-analysis BMJ Open (2016) ;6:e009675. doi: 10.1136/bmjopen-2015-009675
- Khanal, S., Tomlinson, A., McFadyen, A., Diaper, C. and Ramaesh, K Dry eye diagnosis. Investig Ophthalmol Vis Sci.(2008);49(4):1407–1414.
- Olaniyan, S.I., Fasina, O., Bekibele, C.O. and Ogundipe, A.O.(2016). Dry eye disease in an adult population in South-West Nigeria. Contact Lens Anterior Eye;39(5):359–364.
- Willcox, M.D., Argüeso, P., Georgiev, G.A., Holopainen, J.M., Laurie, G.W., Millar, T.J., et al. TFOS DEWS II Tear film report. Ocul Surf (2017);15(3):366–403.
- National Population Commission. Data for National planning and development. 2018 [Accessed 19th February 2021]. Available from: www.nationalpopulation.gov.ng
- Eric B Papas. The global prevalence of dry eye disease: A Bayesian view. Ophthalmic and Physiological optics (2021) ;41(6) :1254-1266
- Onwubiko SN, Eze BI, Udeh NN, Arinze OC, Onwasigwe EN, Umeh RE. Dry eye disease. Prevalence, distribution and determinants in a hospital-based population. Lens Anterior Eye (2014);37(3):175–161.
- Mostafa E. Prevalence of dry eye disease in southern Egypt: a hospital-based outpatient clinic study. J Egypt Ophthalmol Soc(2016) ;109:32–40.
- Castelyn, B., Majola, S., Motilal, R., Naidu, M.T., Ndebele, S.A., Vally T.A, et al. Prevalence of dry eye amongst black and Indian university students aged 18–30 years. African Vis Eye Heal(2015);74(1):1–6.
- de Kluizenaar Y, Roda C, Dijkstra NE, Fossati S, Mandin C, Mihucz VG, et al.Office characteristics and dry eye complaints in European workers-The OFFICAIR study. Build Environ (2016) ;102:54–63. doi.org/10.1016/buildnev.2016.03.013.
- Hikichi, T., Yoshida, A, Fukui, Y., Hamano, T., Ri, M., Araki, K., et al.Prevalence of dry eye in Japanese eye centers. Graefe’s Arch Clin Exp Ophthalmol(1995); 233(9):555–558.
- Kojima, T., Ibrahim, O. ànd Wakamatsu T. The impact of contact lens wear and visual display terminal work on ocular surface and tear functions in office workers. Am J Ophthalmo(2011)l;152(6):933–940.
- Kawashima, M., Yamatsuji, M., Yokoi, N., Fukui, M., Ichihashi, Y., Kato, H. et al. Screening of dry eye disease in visual display terminal workers during occupational health examinations: The Moriguchi study. J Occup Health (2015);57(3):253–258.
- Uchino, M., Schaumberg, D.A., Dogru, M., Uchino, Y., Fukagawa, K., Shimmura, S. et al. Prevalence of dry eye disease among Japanese visual display terminal users. Ophthalmology (2008);115(11):1982–1988.
- Uchino, M., Uchino, Y., Dogru, M., Kawashima, M., Yokoi, N., Komuro A. et al. Dry eye disease and work productivity loss in visual display users: The Osaka study. Am J Ophthalmo(2014)l;157(2):294–300.
- Wolffsohn,, J.S., Arita, R., Chalmers, R., Djalilian, A., Dogru, M., Dumbleton. K., et al. TFOS DEWS II Diagnostic methodology report. Ocul Surf(2017); 15(3):539-574.
- Kolawole, O.U, Iyanda, R.A, Isawumi, M.A. Computer-related vision problems in Osogbo , south-western Nigeria. Afr J Biomed Res 2017 ;20(3):267–272.
- Hashemi, H., Khabazkhoob, M., Kheirkhah, A., Emamian, M.H., Mehravaran, S, Shariat, M, et al. Prevalence of dry eye syndrome in an adult population. Clin Exp Ophthalmol(2014);42(3):242–248.
- Bukhari, A., Ajlan, R, Alsaggaf, H. Prevalence of dry eye in the normal population in Jeddah, Saudi Arabia. Orbit (2009);28(6):392–397.
- Moss, S.E., Klein, R., Klein, B.E. Long-term incidence of dry eye in an older population. Optom Vis Sci(2008);85(8):668–674.
- Lee, A.J., Lee, J., Saw, S.M., Gazzard, G., Koh, D., Widjaja, D. et al. Prevalence and risk factors associated with dry eye symptoms: A population based study in Indonesia. Br J Ophthalmol (2002);86(12):1347–1351.
- Kojima, T. Ibrahim, O. and Wakamatsu, T. The impact of contact lens wear and visual display terminal work on ocular surface and tear functions in office workers. Am J Ophthalmol(2011);152(6):933–940.
- Patil, S, Trivedi, H., Parekh, N. and Jethva J. Evaluation of dry eye in computer users. Int J Community Med Public Heal(2016);3(12):3403–3407.
- Akkaya, S., Atakan, T., Acikalin, B., Aksoy, S. and Ozkurt Y. Effects of long term computer use on eye dryness. North Clin Istanb(2017);5(4):319–322.
- Adesoji A. Mobile technology, social media and 180 million people. JBAMSR (2017);6(5):82–85.