Complications following cardiac pacemaker insertions
Uwanuruochi K1, Shah R A2
Abstract
Context: Permanent pacemaker insertion is a recognised mode of therapy for cardiac arrhythmias. The procedure is carried our regularly at the Cardiac Catheterization laboratory of Madras Medical Mission India.
Aims: This study reviewed the associated morbidity and complications of cardiac pacemaker insertions carried out over fifteen years.
Settings and Design: This study was carried out in the Cardiac Electrophysiology department, of the Institute of Cardiovascular diseases, Madras Medical Mission, India. The study was retrospective.
Material and methods: Data was collected when previously paced patients presented for cardiac interrogation between January to July of 2013. The patients had undergone implantation over the preceding fifteen years. 501 consecutive cases were chosen for analysis.The data obtained was analysed using SPSS statistical software version 15.
Results: The 501 patients had been on pacemaker for variable durations. They comprised 321 males and 180 females. A variety of complications were observed in 33 (6.58%) patients but there was no procedure-related mortality.
Conclusions: Pacemakers were generally well tolerated. Majority of patients were asymptomatic and the rate of complications is 6.58%.
Key-words: Complications, cardiac pacemaker insertions
Introduction
The first permanent pacemaker was inserted in 1958 by AkeSenning, a thoracic surgeon at the Karolinska Hospital in Stockholm.1 Over the years, the indications, techniques, affordability as well as type of cardiac pacemakers have evolved.2 It is currently estimated that, worldwide, about 3 million persons are on cardiac pacemakers.3
Changing epidemiographic profile in the developing countries with increase in cardiovascular risk factors is also well documented.4 Lifestyle change has been especially rapid in many developing countries over the past two decades. The result is an upsurge in cardiovascular diseases.5,6 This supports ongoing research in cardiovascular disease pattern. Appreciation of current trends in cardiac diseases is of public health concern. It is expected that public policy makers as well as individuals adopt the benefit of such research into making choices that lead to better cardiac health outcomes.
This study analysed the clinical morbidity of patients on pacemakers, and the immediate outcome of the cardiac pacemaker insertions at one of the largest tertiary care centres in South-east Asia.
Materials and methods
We studied records of consecutive cardiac pacemaker insertions carried out between January to October 2009, and the follow up record over the years. In our study, we described the demographic characteristics of the patients and the prevalence of associated cardiovascular morbidity in the patients. We documented the frequency of various complications of pacemaker insertions as well as electrophysiologic abnormalities detected. The study was carried out at the Cardiac Electrophysiology department of the Institute of Cardiovascular Diseases, Madras Medical Mission, India. The data was obtained from the records of patients.
The data obtained was analysed using SPSS statistical software version 15. Categorical data was compared using the Chi-square-test while continuous data was compared using T-test. Probability levels of less than 0.05 was considered significant.
Results
Table 1: Spectrum of clinical symptoms present at interrogation
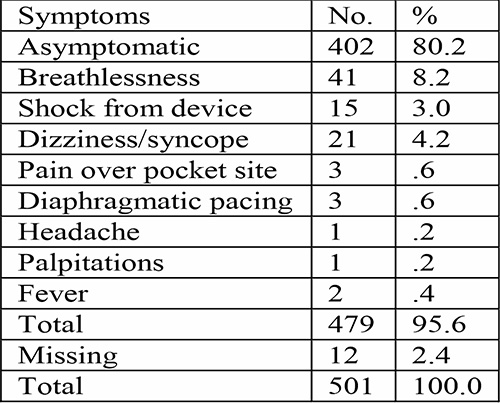
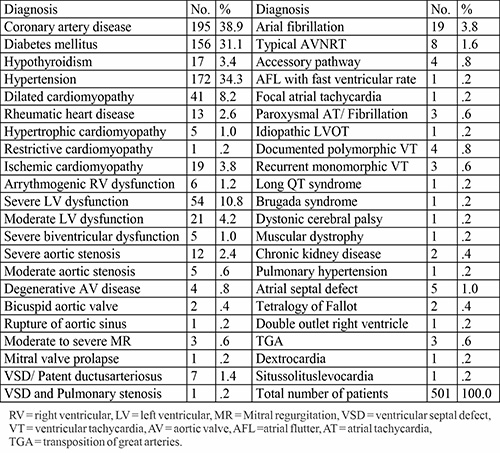
Table 2: Associated medical conditions in paced patients
A total of 501 patients were interrogated with age range of 4-91 years (61.69 ±16.60). Of these, 321 (64.1 %) were males. 370 (73.9%) had their implantation done at MMM.
The duration following implantation varied from one week to 22.25 years, with a mean duration of 3.24 years (±3.28).
The spectrum of clinical symptoms present at interrogation are shown in table 1 while associated medical conditions in the patients were shown in table 2. The indications for pacemaker implantation has been earlier published.7 Only 8 (1.6%) patients had received epicardial leads. Five patients had initial epicardial leads, with endocardial implantation following expiration or elective replacement interval (ERI) of epicardial pacemaker. Two patients had dual epicardial leads, while one had a left ventricular epicardial lead. Three patients were on remote monitoring.
Pacing complications were noted in 33(6.58%). The list includes pacemaker pocket hematoma 4 (0.8%), lead dislodgement 9 (1.8%), endocardial lead displacement 4(0.8%), pocket infection 4 (0.8%), lead fracture 4 (0.8%), lead screw retraction 1 (0.2%) and pocket erosion 3 (0.6%). Abnormal electrophysiologic observations include high lead impedance 7 (1.4%), inappropriate therapy for supraventricular tachycardia 6 (1.2%), ineffective anti-tachycardia pacing and shock from wavelet mismatch 1 (0.2%), T wave over-sensing 2 (0.4%), fusion complexes 2 (0.4%), high lead threshold 20 (4.0%), loss of capture 4 (0.8%), chronotropic incompetence 1 (0.2%), and exit block 1 (0.2%). Complications were managed accordingly, for example explantation and re-implantation for pocket erosion. Electrophysiologic failure were also addressed, supraventricular tachycardia criteria reprogramming for ineffective anti-tachycardia pacing and shock from wavelet mismatch, mode switch was put on for T wave over-sensing, sensed and paced A-V delay was increased in presence of fusion complexes, leads were revised for high impedance and repositioned for loss of capture.
Discussion
Complication rates vary with the definition of complications utilized in various studies. There are no generally accepted norms of complication rates in pacemaker surgery.8 The rate of complications in our study was 6.58%. This compares favourably to the rate of 13.6% reported by Unapkoya et al9 in sub-Saharan Africa. Monib et al10 from a centre in the same subcontinent reported a complication rate of 9.25%. Ozcan et al from Turkey reported 7.6% complication rate in the elderly but 15.1% in young patients11 while Haug and colleagues from Norway had 12.0% complication rate.8 Parsonnet et al12 however identify a complication rate of less than 5% as acceptable.
There was no procedure related mortality. Good procedure related outcome and minimal mortality has also been reported by other workers.13
Conclusion
This study shows that pacemakers were generally well tolerated with majority of patients remaining asymptomatic and a low rate of complications. The study creates more awareness for interventional cardiology in developing countries and encourages continued development of manpower.
Limitations: The retrospective nature that made it difficult to fill up missing data and all indications for pacing do not fit neatly into current complex classifications.
References
- Kirk Jeffrey, Victor Parsonnet. Cardiac Pacing, 1960–1985 A Quarter Century of Medical and Industrial Innovation. Circulation. 1998;97:1978–1991.
- Valentin Tsibulko, Ivo Iliev, Irena Jekova, A Review on Pacemakers: Device Types, Operating Modes and Pacing Pulses. Problems Related to the Pacing Pulses Detection. Int. J. Bioautomation, 2014, 18(2), 89-100
- Mark A. Wood, Kenneth A. Ellenbogen. Cardiac Pacemakers: From the Patient’s Perspective. Circulation. 2002;105:2136–2138 (doi: 10.1161/01.CIR.0000016183.07898.90)
- Omran, A.R. The epidemiological transition: A theory of the epidemiology of population change. Available @ http://www.milbank.org/quarterly/830418omran.pdf.
- Srinath Reddy K. Salim Yusuf. Emerging Epidemic of Cardiovascular Disease in Developing Countries. Circulation. 1998; 97: 596-601 doi: 10.1161/01.CIR.97.6.596.
- Celermajer DS1, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol. 2012 Oct 2;60(14):1207-16. doi: 10.1016/j.jacc.2012.03.074.
- Uwanuruochi K, Shah R A. Review of indications in 501 Cardiac Paced Patients. tjhs 2023, 30(2),33-36.
- Haug B, Kjelsberg K, Lappegård KT. Pacemaker implantation in small hospitals: complication rates comparable to larger centres, EP Europace2011 Nov, 13, (11), , 1580–1586, https://doi.org/10.1093/europace/eur162
- Onakpoya UU, Ojo OO, Eyekpegha OJ, Oguns AE, Akintomide AO. Early experience with permanent pacemaker implantation at a tertiary hospital in Nigeria. Pan Afr Med J. 2020 Jul 13;36:177. doi: 10.11604/pamj.2020.36.177.24425.
- Monib AK, Nepal R, Dhungana S, Bista M, Ghimire R. Early outcome of permanent pacemaker implantation. J Nobel Med Coll 2018 Dec. 7(2):35-8. 11.
- Ozcan KS, Osmonov D, Altay S, Dönmez C, Yıldırım E, Türkkan C, et al. Pacemaker implantation complication rates in elderly and young patients. Clin Interv Aging. 2013;8:1051-4. doi: 10.2147/CIA.S47121.
- Parsonnet V, Bernstein AD, Lindsay B. Pacemaker-implantation complication rates: an analysis of some contributing factors. J Am Coll Cardiol. 1989 Mar 15;13(4):917-21. doi: 10.1016/0735-1097(89)90236-2.
- Villalba S, Roda J, Quesada A, Palanca V, Zaragoza C, Bataller E, et al. Retrospective study of patients who undergo pacemaker implantation in short-stay ambulatory surgery. Long-term follow-up and cost analysis]. Rev Esp Cardiol. 2004 Mar;57(3):234-40. Spanish. PMID: 15056427.