Sociodemographic factors associated with depression in people living with epilepsy in Kano, Nigeria
Owolabi S D
Abstract
Background: A high level of co-morbidity exist between epilepsy and depressive disorder, and in fact it has been found to be the commonest psychiatric disorder in people with epilepsy, with consequence of huge psychosocial burden and poor quality of life. Sociodemographic factors that have been implicated in the association between depression and epilepsy include age, female gender, unemployment, low level of education amongst others.
Objective: To determine the sociodemographic factors associated with depression in people living with epilepsy (PWE) in Kano, Nigeria
Materials and Methods: In this cross- sectional study, two hundred and fifty- five consecutive patients with epilepsy attending the outpatient epilepsy clinics of Kumbotso Health Centre and Neurology/Psychiatry clinics of Aminu Kano Teaching Hospital, Kano were recruited.
Inclusion criteria were age above 18years and being seizure free for two weeks. Patients with severe neurological and cognitive deficits were excluded. Sociodemographic characteristics were obtained using a structured proforma. Diagnosis of depression was made using the M.I.N.I. International Neuropsychiatric Interview.
Results: The age range of participants was 18-76 years with a mean of 32 years (SD=1.31). Majority of participants (57.6%) were males. Prevalence of depression was 20.4%. There was no difference in the mean age of depressed and non-depressed participants. Females had a higher frequency of depression (32%) and association between gender and depression was statistically significant (p ˂ 0.001). Being divorced/widowed and having tertiary level of education were more associated with depression.
Conclusion: Depression is common in PWE with being female a significantly associated factor.
Keywords: Sociodemographic factors, depression, epilepsy.
Introduction
Epilepsy is defined as recurrent seizures due to a chronic underlying process whereas seizure is described as an “excessive discharge of nerve tissue and muscle”. It is a paroxysmal event due to abnormal excessive hyper synchronous discharge from an aggregate of neurons in the central nervous system.1
Over 50 million people world-wide suffer from epilepsy, and according to World Health Organization it is 4-5 times commoner in developing compared to developed countries, hence constitutes a grave problem in middle- and low-income countries.2
Several studies have noted the high occurrence of psychiatric disorders among patients with epilepsy,3-5 in particular depression has been found to be the most common psychiatric disorder in people with epilepsy,6 as up to 50-80% of people living with epilepsy (PWE) are said to develop depression.7-9 Despite this huge burden depression in people with epilepsy remains underdiagnosed and undertreated.10
Major depression is present if a person has either depressed mood or anhedonia, that has lasted for at least two weeks, in addition to minimum of four other symptoms such as changes in appetite and weight, changes in sleep and activity, lack of energy, feelings of guilt, problems thinking and making decisions, and recurrent thoughts of death or suicide and symptom severity to limit occupational and social functioning.11
This co-morbid relationship between epilepsy and depression constitutes a significant public health problem, as each disorder is independently associated with huge psychosocial burden and poor quality of life, let alone co-occurring.
Social sequalae of epilepsy such as stigma, ostracism and social isolation, as a result of misconceptions about its etiology; such as belief that it is as a result of possession, witchcraft or punishment for wrongdoing, makes continuing education and maintaining employment difficult for sufferers, further worsening the cycle of depression.12,13
The association of sociodemographic characteristics with depression in PWE cannot be overemphasized. Studies have shown that PWE with co morbid depression are less likely to be educated, married or employed,14 and are likely to be females.15 Other psychosocial factors that have been associated with depression in epilepsy include seizure worry, change in lifestyle and perceived stigma.15,16
Prior identification of such sociodemographic risk factors will improve the treatment outcome in people with epilepsy, as preventive measures will be applied to forestall occurrence of major depression.
It is based on this background, that this study was conducted. Thus, the aim of this study was to determine the sociodemographic factors associated with depression in PWE in Kano, Nigeria.
Materials and methods
The study is a cross sectional study among consecutive patients with epilepsy attending Health Centre Kumbotso outpatient epilepsy clinic and outpatient Psychiatry and Neurology clinics of Aminu Kano Teaching Hospital, Kano, Nigeria.
Sample size was calculated using Fisher’s formula for calculating sample size;
N=Z2PQ/d2
Inclusion criteria were epileptic patients, age 18 years and above and being seizure free for at least two weeks. Participants with severe neurologic and cognitive deficits were excluded by carrying out complete physical and neurological examination and excluding those with a score of ≤ 15 on modified mini mental state examination respectively. Sociodemographic characteristics such as age, gender, marital status, employment and highest level of education were obtained using a structured proforma and the data collection took four months.
The diagnosis of depression was made using the major depressive module of Mini International Neuropsychiatric Interview (M.I.N.I) version 5 (M.I.N.I 5.0.0) which was developed as a short and efficient diagnostic interview to be used in clinical and research settings17
Major depression was diagnosed if five or more answers from a list of symptoms A1-A3(total of nine symptoms) were coded yes in the major depressive module.
The M.I.N.I has been validated for use among Psychiatric populations and its total administration time is 15-30 minutes.
All data were collated and analyzed using statistical package for Social Sciences (SPSS) version 16.0. Quantitative variables were described using mean and standard deviation (SD) while independent sample t test was used to compare means. Qualitative variables were presented as percentages and bar charts. Chi square was used to compare proportions where appropriate. Confidence interval was 95% and P value ≤ 0.05 was considered significant. Binary logistic regression was done on significant variables to eliminate confounders.
Ethical clearance was obtained from ethical board of AKTH and each participant signed an informed consent form.
Results
Two hundred and fifty-five participants met the inclusion criteria, out of whom 147(57.6%) were males while 108(42.4%) were females. The M:F ratio was 4:3. The age range of participants was 18-76 years with a mean of 32 years (SD=1.31). There was a male preponderance across all age groups at presentation except at the 7th decade where the male female ratio was equal. The age and sex distribution is as shown in figure 1.
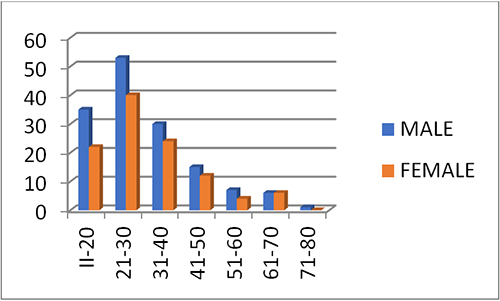
Fig 1. Distribution of age by sex of the participants
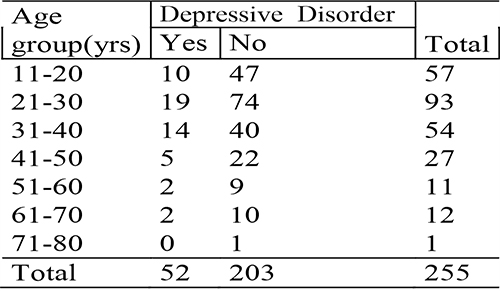
Table 1: Age group at first seizure
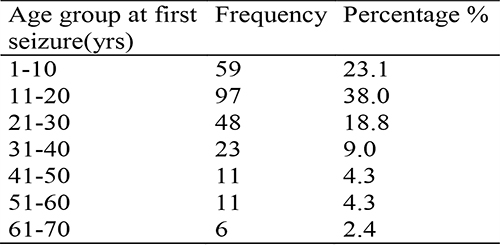
Their age at onset of epilepsy ranged between 1 and 69 years with a mean of 21 (SD=1.46). The peak age frequency at onset of epilepsy was in the second decade (table 1).
Table 2: Socio-demographic characteristics of participants
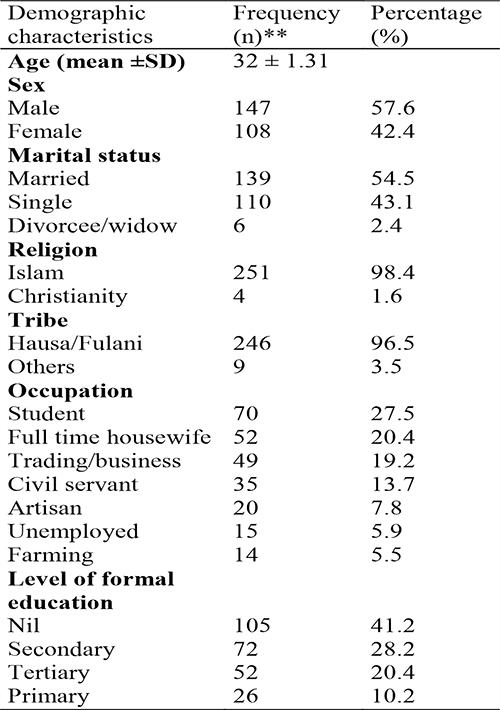
Majority (54.5%) of the participants were married and only a minute (5.9%) percentage were unemployed (table 2).
Table 3: Distribution of the participants by depressive disorder
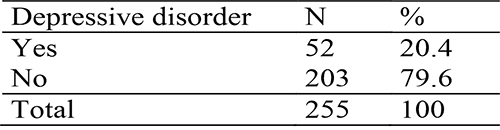
Overall, depressive disorder was present in 52 (20.4%) participants (table 3).
Table 4: Frequency distribution of depression across age group of participants
The frequency of depression was highest (36%) among the age group 21-30years (table 4)
There was no significant difference in the mean age of depressed and non-depressed participants, no statistically significant association was found between age and depressive disorder P=0.941.
Depression was commoner in females compared to males, and a statistically significant association was found between gender and depression. Depression was more frequent in single women (21%) when compared with married women (18.7%)
Table 5: Sociodemographic factors associated with depression in epilepsy
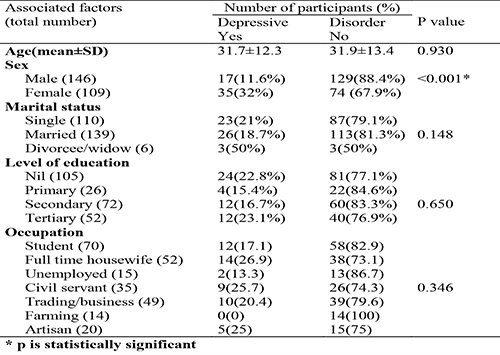
The frequency of depression was highest among participants who had tertiary education (23.1%) compared with those with no formal (22.8%), secondary (16.7%) and primary (15.4%) education. However, this association was not statistically significant. In the occupation category, full time housewives had the highest frequency of depression (26.9%). (table 5)
Discussion
Depression has long been identified as a common co morbid psychiatric disorder among people with epilepsy. Result from the index study revealed a prevalence of depression to be 20.4% in PWE. This is in keeping with prevalence of between 20-55% obtained from previous studies.18 Some Nigerian studies have also reported prevalence of 21.6%-28% using various diagnostic instruments.19,20 This is still in keeping with findings in the current study.
However other local studies have found higher prevalence rates of depression (42%-85.5%) in people with epilepsy.21,22 The high prevalence rates obtained from these latter studies could be attributed to the use of screening tools which have the tendency to overestimate symptoms, when compared with diagnostic instruments. A cross sectional study done in Northern Nigeria found a low prevalence of 8.8%, this study included only patients with epilepsy who had been stable for at least six months.15 Generally prevalence of depression in PWE is said to be as low as 3%, with a range of 3-9% in patients who are stable and seizure free.18
This study found no age difference between depressed and non-depressed patients with epilepsy. This is in conformity with findings from other studies.14 The mean age of participants with comorbid depression and epilepsy was about 31 years, this is similar to findings by Madandola et al.15 Also in this index study, the participants with age range 21-30years had the highest frequency of depression. This is not unexpected as this age range is when many people strive for career development, financial independence and finding a life partner. The realization that all these may not be achievable due to epilepsy may precipitate a depressive illness. This study revealed that females were more likely to be depressed compared to males, and this relationship was statistically significant. This is in keeping with the work of Awoke et al who found that being female, amongst other factors was significantly associated with depression.23 Madandola et al in a study in Northern Nigeria found that 11.9% of females were depressed compared to 7.1% males. A study evaluating the prevalence of depression and associated factors among epileptic patients in Ethiopia also found a higher prevalence of depression in women compared to male participants.24
These findings may be a reflection of the fact that depression is commoner among women in the general population as a result of hormonal factors and internalizing behaviors, amongst other reasons, which are common with women. Some studies have however not found any gender difference between depressed and non-depressed patients with epilepsy.14
This study found that married participants were less likely to be depressed compared to those who are single, divorced or widowed. This has been replicated by various studies.14,15 This can be explained by the social support apparent in being married as it has been found that depression is 2.04 times more likely in epileptic patients with poor social support compared to those with high social support.24 Furthermore, being married might be a protective factor as fear of stigmatization or discrimination, which may make it difficult to get a life partner, may precipitate a depressive illness, and this fear is not applicable in someone who is already married. Although the frequency of depression among participants who had tertiary education in our study is only slightly higher (23.1% vs 22.8%) than for those with no education. It is not unexpected because of the understanding about the illness which an educated person has and its consequent limitations on their achievements. Many studies have found that having no education at all or having lower levels of education is associated with increased frequency of depression.14,15
For instance, Nigus et al found that the odds of developing depression were four times more among participants who had no education whatsoever, whereas it was three to two times more among those who had Primary and Secondary levels of education respectively.24
Depression was more prevalent among full time house wives in our study. In Northern Nigeria, it is not unexpected to find a significant number of women being housewives; this is a cultural concept. This finding may be in support of the work of Brown and Harris, who sought to find how social and cultural factors may influence the onset of depression in women. Part of the vulnerability factors proposed by Brown and Harris include having more than three children under the age of 14 years and not being employed outside the home, these have been found to increase the risk of depression in women.25 Several studies have found that depression is more likely in unemployed patients with epilepsy than those employed.14,26 This further leads to a vicious cycle of unemployment, depression, poverty and poor quality of life.
In its entirety, this study conforms to findings from other studies that being a female with epilepsy is strongly associated with development of depression, while unemployment and being single pose increased risk.
The limitation of our study; though female gender was associated with depression in our study, a controlled study is needed to separate this association from the increased risk of depression in women among the general population.
Conclusion
This study found no age difference between depressed and non-depressed participants with epilepsy, however depression was commoner among females. Participants who were divorced/widowed or single were more likely to be depressed compared to the married ones. Depression was least common among participants with primary level of education, while being a full time housewife was more associated with depression in the occupation category.
References
- Jackson JH. A study of convulsions. Transactions of the Saint Andrew Graduate Association; 1870; 3:162-204.
- The Global Campaign Against Epilepsy, Geneva, World Health Organization, 2000 (Information Pack for the launch of the Global Campaign’s Second Phase,12-13 February 2001).
- Makanjuola RO. Psychiatric and social complications of epilepsy in Nigerians. Trop Geogr Med 1983; 35:299-304
- Gureje O. Interictal psychopathology in epilepsy: prevalence and pattern in a Nigerian clinic. Br J Psychiatry 1991; 158:700-5
- American Association For The Advancement Of Science. Epilepsy A nd Depression-A Two-way street? Science Daily,2005. Retrieved June 6,2011, from http://www.science daily.com.),
- Gilliam FG, Barry JJ, Hermann BP, Meador KJ, Vahle V, Kanner AM. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol 2006;5(5):399–405)
- Albena Grabowska Grzyb, Joanna Jedrzejczak, Ewa Naganska, Urszula Fiszer. Risk factors for depression in patients with epilepsy. Epilepsy and Behavior 2006; 8:411-417
- Mendez MF, Cummings J, Benson D, et al. Depression in epilepsy. Significance and phenomenology. Arch Neurol 1986; 43:766-770
- Standage K, Fenton G. Psychiatric symptoms profile of patients with epilepsy: a controlled investigation. Psychol Med 1975; 5:152-160
- Andres M Kanner. Should Neurologists be trained to recognize and treat comorbid depression of neurologic disorders? Yes. Epilepsy and Behavior 2005; 6:303-311
- Mula M. American Psychiatric Association, Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC 2013: American Psychiatric Association.
- Hermann BP, Whitman S, Wyler AR, Anton MT, Vanderzwagg R. Psychosocial predictors of psychopathology in epilepsy. Br J Psychiatry 1990; 156:98–105.
- Dada T.O and Odeku E.L. Epilepsy in the Nigerian patient. West African Medical Journal 1966; 15:153-163)
- Alexander W. Thompson, John W Miller, Wayne Katon, Naomi Chaytor, Paul Ciechanowski. Sociodemographic and Clinical Factors associated with Depression in Epilepsy. Epilepsy&Behaviour 2009; 14:655-660
- Madandola N, Sale S, Adebayo A, Obembe A, Salihu A, Bakare A, Danjuma I. Sociodemographic and Clinical Variables of Depression among Patients with Epilepsy in a Neuropsychiatric Hospital in Nigeria. Depression Research and Treatment 2020;(3):1-7
- Dabilgou A., Nanema D., Dravé A., Sawadogo S., Kyelem J., Napon C.et al. Symptoms of Depression and Associated Risk Factors in Patients with Epilepsy in Burkina Faso. Open Journal of Depression 2019; 8: 29-40. doi: 10.4236/ojd.2019.81004.
- Sheehan DV., Lecrubier Y., Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview ( M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin Psychiatry 1998;59(Suppl 20): 22-23
- Kanner AM. Depression in Epilepsy: Prevalence, clinical semiology, pathogenic mechanisms and treatment. Biol Psychiatry 2003; 54:388-98.
- Adewuya AO, Ola BA. Prevalence of and risk factors for anxiety and depressive disorders in Nigerian adolescents with epilepsy. Epilepsy Behav 2005; 6:342–7.
- Kazeem A, Dauda S. Predictors of psychiatric disorders among people living with epilepsy as seen in a Nigerian tertiary health institution. Niger Med J 2016; 57:24–30.
- Ogunrin OA, Obiabo YO. Depressive symptoms in patients with epilepsy: Analysis of self-rating and physician's assessment. Neurol India 2010; 58:565–70.
- Onwuekwe I, Ekenze O, Bzeala-Adikaibe, Ejekwu J. Depression in patients with epilepsy: A study from Enugu, South East Nigeria. Ann Med Health Sci Res 2012; 2:10–3.
- Chaka A., Awoke T., Yohannis Z. et al. Determinants of depression among people with epilepsy in Central Ethiopia. Ann Gen Psychiatry 2018; 17:27. https://doi.org/10.1186/s12991-018-0197-z
- Nigus A.E., Lemi B. and Adamu K. Prevalence of depression and associated factors among epileptic patients at Ilu Ababore zone hospitals, South west Ethiopia 2017: a cross-sectional study. Annals of General Psychiatry 2020; 19:19
- Patten, S. B. Are the Brown and Harris "vulnerability factors" risk factors for depression? Journal of Psychiatry & Neuroscience 1991; 16(5):267–271.
- Chaka, A., Awoke, T., Yohannis, Z. et al. Determinants of depression among people with epilepsy in Central Ethiopia. Ann Gen Psychiatry 2018; 17:27. https://doi.org/10.1186/s12991-018-0197