Biochemical analysis and management of phaeochromocytoma: A case report
Familoni O.M, Uwanuruochi V.N, Uwanuruochi K, Elendu K.C.
Abstract
Phaeochromocytoma is a tumour from chromaffin cells in adrenal medulla or extra-adrenal autonomic ganglia, usually releasing catecholamines and metanephrines. It is an unusual cause of severe hypertension in the young. This is the first report from our hospital, the Federal Medical Centre, Umuahia. There are important steps in management which if unattended to results in high peri-operative mortality. This article highlight these issues in its management.
Keywords: Biochemical, management, analysis, Phaeochromocytoma
Introduction
There have been few reports of phaeochromoctoma from various centres in Nigeria.1-4 It is a rare cause of hypertension and diagnosis is often delayed. Our case report highlights the need for higher index of suspicion, understanding of current guidelines for diagnosis and modalities of management that enhance early diagnosis and reduce morbidities and mortality in patients.
Case report
A 27 year old male complained of recurrent abdominal pain, headache and palpitations for 4 years. The headache was severe, frontal and associated with light headedness and diaphoresis He also had nausea, vomiting, recurrent constipation and generalised body weakness and occasional shortness of breath. He was not hypertensive, and did not abuse drugs. For the past one year, he had increased urination, thirst, appetite and progressive unintentional weight loss and undue fatigue. He was not known to be diabetic.
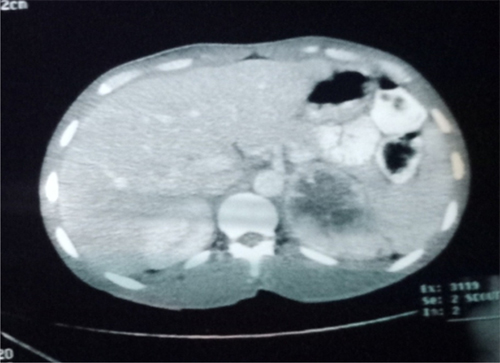
Figure 1: A left 7 cm pheochromocytoma seen on a CT scan
He sought care at a private hospital where abdomino-pelvic ultrasound scan showed left hypoechoic mass suspected to be splenic. He was given some medications for splenic enlargement. At the Babcock University teaching hospital a computer tomography of the abdomen was done, localised a tumour in the adrenal gland (Figure 1). There was a rim enhancing isodense mass in the left suprarenal region. The mass has a Hounsfield unit value ranging from 10 to 65 and measures 76 x 71 x 57mm in its widest longitudinal, anterior-posterior and transverse dimensions. No area of macroscopic fat is seen. The mass is seen to compress the left kidney but no definite invasion of adjacent structures is seen, revealing features of left large adrenal mass likely adrenal carcinoma with no evidence of metastasis to any intra-abdominal organs.
He could not follow up his treatment in the hospital due to financial constraints and came to our hospital, which is near his home and family. He was first seem at general out-patient, and sent to the Endocrine clinic. He was acute on chronically ill-looking, wasted and lethargic.
His random blood sugar record was above 33.3 mmol/L on the Accu-chek glucometer. His pulse was 87beats per minute, blood pressure was 130/90mmHg, respiration 23per minute, and oxygen saturation 97% at room air. He had left flank pain, radiating to the epigastrum. He was lethargic, but well oriented with no muscle weakness.
We entertained phaeochromocytoma with secondary diabetes in hyperosmolar, hyperglyceamic state. The following investigations were requested: serum cortisol (9am), plasma free metanephrine, 24 hour urine creatinine, total cathecholamine, vanillylmandelic acid and metanephrine, serum testosterone, dihydrotestosterone, dehydroepiandrosterone, Hemoglobin A1C, Brain magnetic resonance imaging.
Table 1: Biochemistry results of patient
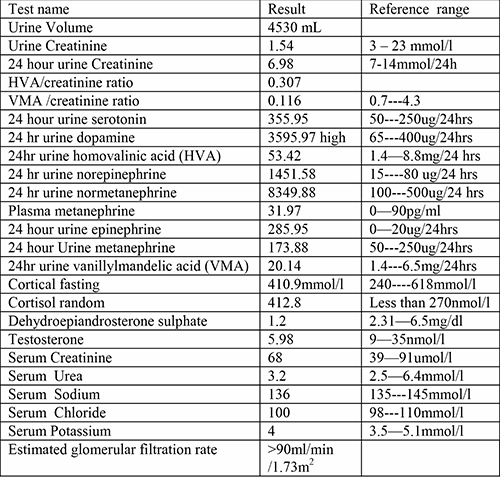
He was rehydrated with normal saline and hyperglycaemia was controlled with regular insulin. He was placed on phenoxybenzamine 10mg daily and doxazosin 2 mg daily. Laboratory results obtained are shown in Table 1. It showed biochemical evidence of phaeochromocytoma.
Brain magnetic resonance imaging and C-peptides were not done due to financial constraints. By the following day, he was better, with good glycaemic control (random blood sugar 198 mg/dl (11 mmol/L). His pulse was 128 beats/minute, so propranolol 40mg daily was added. He was discharged to the clinic on the fourth day. He is being prepared for adrenalectomy, with continued alpha and beta adrenergic blockade.
Discussion
Pheochromocytoma is a rare cause of secondary hypertension, with a prevalence of about 0.2–0.6%.5 This is the first documented case in our centre. Management is demanding as it may precipitate life-threatening hypertension or cardiac arrhythmias because of excessive catecholamine secretion.6
Headaches, palpitations, and sweating which were all present in our patient are the classic triad of symptoms seen in pheochromocytoma6. The triad has a specificity of 93.8%, a sensitivity of 90.9% and an exclusion value of 99.9% for the diagnosis of phaeochromocytoma.7 Their presence in hypertensive patients justifies assays of blood or urinary catecholamines. Their absence virtually excludes phaeochromocytoma.
Proper interpretation of biochemical analysis is important. Initial biochemical tests of paragangliomas (PPGLs) should include measurements of plasma free metanephrines.8 Metanephrines are normetanephrine and metanephrine, the degradation products of noradrenaline and adrenaline respectively.
Elevated plasma free metanephrines is considered the gold standard for diagnosis, with a sensitivity of 99% and specificity of 89%.9 Positive results is greater than > 2-3 folds elevation, 24h Urine catecholamines above 2-fold elevation, 24h Urine total metanephrines above 1.2 ug/d (6.5 umol/d), 24h Urine VMA > 3-fold elevation. Sensitivity approaches 90% and specificity 98% when urinary catecholamine is combined with urinary total metanephrines. Urinary fractionated metanephrines have equivalent sensitivity, but much lower specificity (about 45%). They are useful for initial screening.9
24hr urine normetanephrine, dopamine, epinephrine and norepinephrine were markedly elevated in our patient, but 24 hour urine metanephrine and plasma metanephrine were normal. Separate measurement of metanephrine and normetanephrine is required (fractionating) and an elevation in either is considered positive.10 Normal plasma metanephrine in the presence of markedly elevated urine catecholamines suggest a dopamine secreting paraganglioma, a very rare occurrence.10
VMA is a metabolites of the norepinephrine and HVA is a metabolites of the dopamine. They were elevated in our patient. Elevated HVA supports a diagnosis of neuroblastoma and malignant pheochromocytoma. Measurements of urinary dopamine and plasma 3-methoxytyramine are useful for the biochemical diagnosis of PPGLs with predominantly dopamine secretion and/or high risk for metastases.11 Low levels of HVA in presence of high levels of dopamine suggest poor conversion of dopamine.
After biochemical confirmation, the tumour is localized using either computed tomography or magnetic resonance imaging.12 The location in the suprarenal region, variable display and enhancement with contrast are features helpful for its identification.
Preparation for surgery is multidisciplinary, involving endocrinologists, anaesthesiologists, surgeons and cardiologists. Most commonly, phenoxybenzamine is used for pre-operative blockade of catecholamines. It should be started at least 10-14d preoperatively, at starting dose of 10 mg twice a day, with stepwise increases of 10 to 20 mg every 2-3 days until until blood pressure and paroxysms are controlled. The final dose of 1mg/kg of body weight is reached. The Maintenance is usually 40-80 mg/day.9 To reduce tachycardic reflex responses while patients are on alpha-blockers, a low dose beta-blockade is started only after effective a-blockade. It also prevents arrhythmia during surgery. Propanolol is usually started at 10 mg twice a day, and increased to control the heart rate.
References
- Ugwumba FO, Okafor OC, Okoh AD, Ajuzieogu OV. Phaeochromocytoma in a 20-year-old Nigerian, resolving the dilemma of benignity or malignancy. Clin Pract. 2012 Jan 18;2(1):e15. doi: 10.4081/cp.2012.e15. PMID: 24765414; PMCID: PMC3981342.
- Adenekan A, Faponle A, Badmus T, Sanusi A. Anaesthetic management of giant phaeochromocytoma in a patient with chronic renal disease. J West Afr Coll Surg. 2011;1(2):112-122.
- Atim T, Aiyekomogbon JO. Retroperitoneal paraganglioma causing proximal ureteric obstruction in a child: diagnostic conundrum and immunohistochemistry characteristics (case report). Pan Afr Med J. 2022;43:79. Published 2022 Oct 13. doi:10.11604/pamj.2022.43.79.29159
- Afuwape O, Ladipo JK, Ogun O, Adeleye J, Irabor D. Pheochromocytoma in an accessory adrenal gland: a case report. Cases J. 2009 Aug 3;2:6271. doi: 10.4076/1757-1626-2-6271. PMID: 19918568; PMCID: PMC2769278.
- Ariton M, Juan CS, AvRuskin TW. Pheochromocytoma: Clinical observations from a Brooklyn tertiary hospital. Endocr Pract 2000; 6: 249–252
- Zuber SM, Kantorovich V, Pacak K. Hypertension in pheochromocytoma: characteristics and treatment. Endocrinol Metab Clin North Am. 2011 Jun;40(2):295-311, vii. doi: 10.1016/j.ecl.2011.02.002. PMID: 21565668; PMCID: PMC3094542.
- Plouin PF, Degoulet P, Tugayé A, Ducrocq MB, Ménard J. Screening for phaeochromocytoma : in which hypertensive patients? A semiological study of 2585 patients, including 11 with phaeochromocytoma. Nouv Presse Med. 1981 Mar 7;10(11):869-72. French. PMID: 7208288.
- Ku EJ, Kim KJ, Kim JH, Kim MK, Ahn CH, Lee KA, Lee SH, Lee YB, Park KH, Choi YM, Hong N, Hong AR, Kang SW, Park BK, Seong MW, Kim M, Jung KC, Jung CK, Cho YS, Paeng JC, Kim JH, Ryu OH, Rhee Y, Kim CH, Lee EJ. Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force. Endocrinol Metab (Seoul). 2021 Apr;36(2):322-338. doi: 10.3803/EnM.2020.908. Epub 2021 Apr 6. PMID: 33820394; PMCID: PMC8090459.
- Hannah-Shmouni F, Pacak K, Stratakis CA. Metanephrines for Evaluating Palpitations and Flushing. JAMA. 2017 Jul 25;318(4):385-386. doi: 10.1001/jama.2017.5926. PMID: 28742886; PMCID: PMC7457564.
- Bozin M, Lamb A, Putra LJ. Pheochromocytoma with Negative Metanephrines: A Rarity and the Significance of Dopamine Secreting Tumors. Urol Case Rep. 2017 Mar 21;12:51-53. doi: 10.1016/j.eucr.2017.02.002. PMID: 28337414; PMCID: PMC5362136.
- Därr R, Lenders JW, Hofbauer LC, Naumann B, Bornstein SR, Eisenhofer G. Pheochromocytoma - update on disease management. Ther Adv Endocrinol Metab. 2012 Feb;3(1):11-26. doi: 10.1177/2042018812437356. PMID: 23148191; PMCID: PMC3474647.
- Francis I.R., Korobkin M. (1996) Pheochromocytoma. Radiol Clin North Am 34: 1101–1112.