Diabetic foot amputations in Nigeria; raising awareness to the burden of diabetic foot syndrome
Ebojele FO*, Iyawe VI
Abstract
Background: In recent times, our community has been inundated with an increasing number of amputees and of course an increasing number of people requiring lower limb prosthesis. We have also witnessed a surge in the prevalence of Diabetes, Diabetic Foot Syndrome and Diabetic foot gangrene.
Aim: The aim of this study is to highlight the increasing contribution of Diabetic Foot Gangrene to our teaming population of Amputees and to emphasize that this can be ameliorated with definite, multidisciplinary Public Health Strategies aimed at increasing awareness to this ailment as well as early diagnosis and control of Diabetes.
Methods: This was a descriptive, quantitative and prospective study of all amputations done at the University of Uyo Teaching Hospital and selected Private Hospitals in Uyo, Niger Delta region of Nigeria which is ongoing.
Results: A total of 49 unilateral amputations of either the upper or lower limb were done. They were 21 Males and 28 Females. Patients in the 4th to 6th decades of life who had Diabetic foot gangrene, majority of whom were females were the highest number who underwent amputation 30 (61.2%). Most of the patients 27, out of 30 (90%) were diagnosed as Diabetic for the first time with foot gangrene. There is therefore a strong need to increase the awareness of our society to Diabetes and the negative effects of its complications particularly diabetic foot syndrome and gangrene.
Conclusion: Diabetic foot gangrene was the commonest indication for amputation in this series and was responsible for 30 out of 49 (61.2%) amputations.
Keywords: Diabetes, Diabetic Foot Gangrene, Amputations, Awareness.
Introduction
Diabetic Foot Syndrome (DFS) is a spectrum of clinical entities that affect the feet of Diabetics as a complication of Diabetes. Amputation is the removal of a whole or part of a limb.1 Cutting through the joint will be more specifically referred to as disarticulation. It is one of the oldest surgical procedures with a history of over 2500 years dating back to the Hippocratic times.2,3 It however, retained its relevance in modern times to safe life or remove a dead or useless limb.1
In our society, amputation is viewed as a failure of orthodox Orthopaedic practice, particularly due to the fact that the procedure of amputation is done mainly in the hospital. The other reason amputation is viewed as a failure of orthodox Orthopaedic practice is that our society feels everything was not done to rescue the limb irrespective of the reason behind the amputation; be it severe crush limb injury, ascending limb gangrene, a useless limb from congenital deformities or a dangerous limb due to a mitotic lesion.
This position is compounded by our religious and cultural belief that ailments have a spiritual origin or cultural myths associated with them. Against the foregoing, the decision to have amputation in our society is a very difficult one. This has become a family or community decision. In the midst of all these, the health seeking behaviour of our people is such that the hospital is the last port of call after severally seeking treatment from traditional medical practitioners and spiritual houses for any kind of medical ailment.
The poor health seeking behaviour of our people, poverty, dearth of health insurance, low availability and access to proper medical services are some of the factors militating against early diagnosis and management of diabetes in our community. Additionally, with the aging global population and with the increased prevalence of diabetes, the magnitude of this problem will increase.2,4-8 It is said that diabetes has become an epidemic health problem with a 32% increase globally over the past decade.2,8,9 In most developed countries, the incidence of diabetic foot syndrome (DFS) is about 2%.4,8,10-12 In Nigeria, the prevalence of diabetes is said to be 11–32% amongst hospitalized patients8,13 and in the last two decades, Nigeria has witnessed more than 100% increase in the prevalence of diabetes from 2.2% in 1997 to nearly 6% in 2015.8,13,14 Therefore, as the most populous country in Africa, Nigeria has the greatest burden of Diabetes within the Sub-Saharan Sub-continent.8,13,15 It is therefore not surprising that there is increasing incidence and prevalence of diabetic foot syndrome and diabetic foot gangrene in our community. These pose a serious threat to our local and national economy and put enormous pressure on our healthcare services.
In this series, 61.2% (30/49) of amputations were indicated by Diabetic Foot Gangrene (DFG) as a leading indication with trauma coming a distant second 14 (28.6%)1,8 as against and much higher than reports by many Nigerian authors16-20 who reported 14.1% - 29.3% amputations indicated by diabetic foot gangrene between 2001 and 2015 when trauma was a leading indication for amputation. It also varies with reports from other African authors who reported trauma as the leading indication for amputation.2,22 The lamentations of Ejiofor et al therefore, hold strong that the burden of Diabetic Foot Ulcer and DFG in Nigeria is very high.13 He emphasized the major gaps in the control and management of diabetes to include low foot care knowledge amongst diabetic patients, over-dependence on self-medication and unorthodox medication and treatment following development of foot ulceration, late hospital presentation and high amputation and mortality rates.8,13 These problems have added to increase the burden of diabetic foot syndrome, diabetic foot gangrene and amputations amongst diabetics in our community to the extent that diabetics are now first time hospital presenters with foot gangrene (27 of 30 Amputees).8 The adverse social implications and the effects on life and self-image are therefore devastating.4,8 It is said that major limb amputation is associated with profound economic, social and psychological effect on the patient and family especially in developing countries where the knowledge and acceptance of prosthetic use is poor.3
Family, Community and National income and economy are negatively affected even more, as we now have an increasing number of amputees in the 4th to 6th decades of life in our community courtesy of diabetes. The contributions from these family breadwinners and experienced workforce to national economy is stunted or lost completely. It is important therefore, that we bring this to the notice of government, healthcare providers, our community and other stakeholders that the increasing burden of diabetes, diabetic foot syndrome and diabetic foot gangrene is breeding poverty in our society with careful note that these diabetic amputees will also be on medications and treatment of diabetes for life.
Patients and Methods
It is an ongoing prospective and descriptive study which commenced in January 2018 at the University of Uyo Teaching Hospital, Uyo and other selected private hospitals in Akwa Ibom State, Niger Delta region of Nigeria. All patients who had any form of amputation of the upper or lower extremity were included in the study. Data was collected based on age, sex, indication for amputation, level of amputation and period between diagnosis of diabetes and development of gangrene. It was analysed using Microsoft Excel into averages, frequencies, charts and histograms.
Results
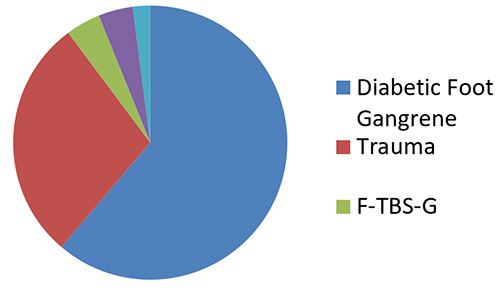
A total of 49 unilateral amputations were recorded in the study. The age range was 19 to 71 years, 28 females were amputated compared to 21 males giving a male to female ratio of 1:1.3. There was bimodal distribution pattern of amputation with the early peak in the 2nd to 4th decades of life contributed mainly by trauma 14(28.6%), while the second peak in the 4th to 6th decades of life was contributed mainly by Diabetes 30(61.2%) due to diabetic foot gangrene (DFG) (Fig.1). Most patients amputated due to diabetic foot gangrene (DFG) were females 19 who contributed majority of the amputations 30 (61.2%) and many of them were diagnosed diabetic for the first time with foot gangrene 27 (90%) (Fig.3). Below-knee amputation was the commonest amputation that was done 36 (73.5%) and it was amongst DFG patients 29 (59.2%).
Figure 1: Indications for amputation
Discussion
With the rising incidence and prevalence of Diabetes in our society, Diabetic Amputations (or amputations) have become a common term in our society. It is an albatross that tends to pitch the patient and relatives against the attending Physician and Surgeon as it is now a family or community decision to undergo amputation. In this series, the highest indication for amputation was Diabetic foot gangrene (DFG) 30(61.2%) (Fig.1).
The peak age group for amputations in our series was the 4th to 6th decades of life which contributed 34 (69.4%) amputations. These amputations in this age category were mainly due to Diabetic foot gangrene 29(59.2%). Females had more amputations in this series 28(57.1%) than males 21(42.9%), giving a male to female ratio of 1: 1.3. This varies widely with findings from other authors in Nigeria,1,17-21,24 Africa 2(3.6:1),22 and the rest of the world9,11,25-27 who found more males than females undergoing amputations. Most of these females had amputations indicated by diabetic foot gangrene 19 of 30 as against 9 who had amputations indicated by other reasons. Solagberu et al19 in his study in 2001 also found DFG dominate in females over 30 years who had amputation. Females are more religious, are likely to have a lower income in our society and are less likely to be involved in the decision making process that favours Health seeking behaviours to the hospital. These factors ensure that Diabetic females (and other females with limb ailments) indulge in self and unorthodox medication, traditional treatment and spiritual treatment and healing. The result is poor control of Diabetes, late hospital presentation, early development of foot ulcers from poor foot care knowledge and high rate of gangrene and amputation amongst female Diabetics. It must be emphasized here that, amputations in this cases are usually carried out as a last resort when limb salvage is impossible, when the limb is dead or viable but non- functional or when the limb endangers the patients’ life.3 This is due to the fact that our patients seek traditional therapy, spiritual therapy and other unorthodox treatment as a first line for almost every kind of ailment. This is reported by other Nigerian authors.3,8,15-18 There is also a raging propaganda amongst our locals generated by TBS that seeking orthodox Orthopaedic care will ultimately result in amputation (in any case, amputations are only carried out in our hospitals by orthodox Orthopaedic practitioners). Ndukwu et al3 argued that the circulation of this kind of propaganda with the actual reality of poor health seeking to hospitals may ultimately result in a vicious cycle of continued late presentations to orthodox Orthopaedic care and subsequent high prevalence of amputation.3
It is therefore not surprising that in this series of amputation, diabetic foot gangrene (DFG) 30(61.2%) (Fig. 1) towers above all other indications for amputation including trauma 14(28.6%), 2(4.1%) each for peripheral arterial disease (PAD) and fracture – traditional bone setter-gangrene (F-TBS-G) while tumour was 1(2.0%). This finding differs from that of other authors in Nigeria1,16-21 and Africa2,22 where trauma is the leading indication for amputation. It however agrees with a recent finding by other Nigerian authors that DFG is the leading indication for amputation in their series in 2015(71.4%) and 2020 (56.8%).3,8 Ndukwu et al suggest a changing trend as in the past trauma and TBS-G were the leading indications for amputation in Nigeria (Onuminya 2000, Solagberu 2001, Kidmas 2004, Akiode 2005, Thanni 2007, Ekere 2013, Ajibade 2013).1,16-21 Ndukwu et al added that the high evolving incidence of diabetic complications may be as a result of increasing urbanization with adverse change in life style and diet, complicated by a low awareness of the disease and its complications with inappropriate patient education on foot care and poor health seeking attitude.3 Reports from South Korea,28 Jordan4 and other developing countries like India,29 Tanzania,22 Pakistan30 and Singapore31 also present diabetic foot gangrene (DFG) as the leading indication for amputation in their countries. These have to do with the 32% global increase in incidence4,9 and prevalence4-7 of diabetes as it has now become an epidemic health problem. These countries have also made significant progress in the control and treatment of extremity injuries.
In countries of Europe and America, peripheral arterial disease (PAD) is said to be the leading indication for amputation.4,27,32-34 The ageing population of the developed countries tends to ensure prevalence of hypertension, vasculitis, atheromatous plagues and heart diseases. The temperate weather in these countries encourages frostbite and vascular occlusion possibly of already compromised blood vessels.
In our series, trauma comes a distant second 14(28.6%) while F-TBS-G and PAD each contributed 2(4.1%) and tumour 1(2.1%). These findings vary widely with that of other Nigerian authors.1,16-21 but agree with that of Ndukwu et al3 in 2015. Ndukwu et al opined that the lower percentage of amputations due to trauma in their study may be due to a more efficient public enlightenment campaign on road safety measures together with prompt management of cases of trauma in their facility. This is also the situation in our study. Additionally, since the ban on the use of motorcycles for commercial transportation in the Uyo metropolis in Akwa Ibom State in 2012, we have witnessed a sharp reduction in grostegue extremity wounds and crush limb injuries requiring amputation in our hospital. These factors, added to proper management of limb ailments and injuries, a better outcome of the cases of trauma in our facility and the increasing ability to salvage limbs for patients with severe limb trauma or those mismanaged by TBS has also contributed to lower indication for amputation by F-TBS-G (4.1%) in our series. I dare say that contributions of TBS to management and mismanagement of limb injuries and ailments in our community can be reduced by producing superior results or better outcome in orthodox orthopaedic care apart from concerted efforts to reduce trauma on the one hand and the cost of medical care by Health Insurance on the other.
Conclusion
This study has identified DFG as the leading indication for amputation in our community and has also showed that there is a changing trend from trauma and TBSG as the leading indication for amputation in Nigeria.
We must therefore put our acts together, apply concerted, multidisciplinary and public health strategies to raise awareness to diabetes, control diabetes and its attendant complications. Some of these strategies may include; increasing public health campaigns through the media and otherwise, to increase awareness of diabetes and its complications, routine testing by every health facility of all patients 30 years and above for blood and urine sugar, establishment of multidisciplinary and super specialty diabetic clinics in our tertiary hospitals and improved training of specialist physicians and surgeons in diagnosis and management of diabetes and its complications particularly diabetic foot syndrome.
References
- Ajibade A, Akinniyi O.T, Okoye C.S, Indications and Complication of Lower Limb amputations in Kano, Nigeria. Ghana Medical Journal 47: 185 – 188.
- Berhe G, Kibrom G, Reiye E, (2018). Patterns and causes of amputations in Ayder referral Hospital, Mekelle, Ethiopian: A three year experience. Ethiop J. Health Sci 28:31 – 36.
- Ndukwu C, Muoneme C. (2015). Prevalence and Pattern of Major extremity amputation in a tertiary hospital in Nnewi, South-east Nigeria. Trop. J. Med. Res.18: 104-114.
- Qusai Aljarrah, Mohammed Z.A, Sohail B, Abdelwahab A, Hasan O. et al (2019). Major lower extremity amputation; a contemporary analysis from an academic tertiary referral centre in a developing community. BMC surgery 19:170.
- Shaw J.E, Sicree R.A, Zimwet for 2010 and 2030. Diabetes Res Clinical Pract. 87: 4 – 4.
- Ziegler-Graham K, Mackenzie E.J, Ephraim P.L, Travison T.G, Brookmeyer R. (2008). Estimating the prevalence of limb loss in the United States; 2005 to 2050. Arch Phys Med Rehabil 89:422 – 429.
- Narres M, Kritkina T, Classen A, Droste S, Shuster B, et al. (2017). Incidence of lower extremity amputations in the Diabetic compared to the nondiabetic population; a systematic review. PLOS ore 12:e0182081.
- Inyang U.C, Benson S, Nottidge T.E, Amanari C.O, Ettah O.E, Ekpenyong C.E (2020). Current trends in Indications and epidermiological characteristics of amputations in Nigeria. Journal of Orthopaedic Research and Therapeutics 2:
- de Jesus-Silva S.G, de Oliveira J.P, Brianezi M.H.C, Silva M.A.M, Krupa A.E, et al (2017). Analysis of risk factors related to minor and major lower limb amputations of a tertiary hospital J. Vasc Bras 16:16 – 22.
- Boulton A.J, Vileikyte L, Ragnarson-Tennvall G, Apelgrist J. (2015). The global burden of diabetic foot disease. Lancet 366:1719 – 1724.
- Tabor S, Enen M.A, Celik Y, Dag O.F, Sabuncu T, et al. (2015). The major predictors of amputation and length of stay in diabetic patients with acute foot ulceration. Wien Klin Wochenschr 127: 45 – 50.
- Rogers L.C, Andros G, Caporusso J, Harkless L.B, Mills J.L. Sr, et al. (2010). Toe and flow; essential components and structure of the amputation prevention team. J. Vasc Surg 52: 235 – 275 of the amputation prevention team. J. Vasc Surg 52: 235 – 275.
- Ejiofor U, Olufunmilayo A, Ibrahim G, Innocent O. Marcelina E, et al (2019). Burden of diabetic foot ulcer in Nigeria: Current evidence from the multicenter evaluation of diabetic foot ulcer in Nigeria. World Journal of Diabetes 10:200 – 211.
- Adeloye D, Ige J.O, Aderemi A.V, Adeleye N, Amoo E.O, et al. (2017). Estimating the prevalence, hospitalization and mortality from type 2 diabetes mellitus in Nigeria: a systematic review and meta-analysis. BMJ open 7:e015424.
- Mbanya J.C, Motala A.A, Sobngwi E, Assah F.K, Enoni S.T, (2010). Diabetes in Sub-Saharan Africa. Lancet 375:2254 – 2266.
- Kidmas A.T, Nwadiaro C.H, Igun G.O. (2004). Lower limb amputation in Jos, Nigeria. East Afr. Med. J. 81: 427 – 427.
- Onuminya J.E, Obekpa P.O, Ihezue H.C, Ukegbu N.D, Onabowale B.O. (2000). Major amputations in Nigeria; a plea to educate Traditional bone setters. Trop. Doct. 30: 133 – 135.
- Ekere A.U. (2013). The Scope of extremity amputations in a private hospital in the South-south region of Nigeria. Niger J. Med. 12: 225 – 228.
- Solagberu B.A. (2001). The Scope of amputations in a Nigerian teaching hospital. Afr. J. Med. Sci. 30: 225 – 227.
- Akiode O.A, Shonubi O.S, Musa A, Sule G. (2005). Major limb amputations: An audit of indications in a sub urban surgical practice. J. Nat’l Med. Assoc. 97. 74 – 78.
- Thanni L.O, Tade A.O. (2007). Extremity amputation in Nigeria – a review of indications and mortality surgeons 5: 213 – 217.
- Chalya P.L, Mabula J.B, Dass R.M, Ngayamela I.A, Chandika A.B, et al. (2012). Major limb amputations: a tertiary hospital experience in North-western Tanzania. J. Orthop. Surg. Rest. 7: 18.
- Umaru R.A, Gali B.M, Ali N. (2004). Role of inappropriate splintage in limb amputation in Maiduguri, Nigeria. Ann Afr. Med. 3: 138 – 140.
- Abbas A.D, Musa A.M, (2007). Changing pattern of extremity amputations in University of Maiduguri Teaching Hospital, Nigeria. Niger J. Med.16: 330 – 333.
- Aulivola B, Hile C.N, Hamdam A.O, Sheadan M.G, Veraldi J.R, et al. (2004). Major lower extremity amputation: outcome of a modern series. Arch. Surg. 139: 395 – 399.
- Cruz C.P, Eidt J.F, Capps C, Kirtley L, Moursi M.M. (2003). Major lower extremity amputations at a veterans affairs hospital. AMJ. Surg. 186: 449 – 454.
- Limb T.S, Finlayson A, Thorpe J.M, Sieunarine K, Mwipatayi B.P, et al. (2006). Outcomes of a contemporary amputation series. ANZJ. Surg. 76: 300 – 305.
- Se-Young K, Tae H.K, Jun-Young C, Yu-Jim K, Dong H.C, et al (2018). Predictors for amputation in patients with Diabetic Foot wound. Vasc Specialist International 34: 109 – 116.
- Unnikrishran E.P, Rollands R, Parambil S. (2017). Epidermiology of major limb amputations: a cross sectional study from a South Indian tertiary care hospital. Int Surg. J4: 1642 – 1646.
- Ubayawansa D.H, Abeysekera W.Y, Kumana M.M. (2016). Amputations in a tertiary care hospital J. Coll Physicians Surg. Pak 26: 620 – 622.
- Khalid K.A, Sulong A.F, Nazri Mohd Yusof, Jamalludin Ab. Rahman, Ahmad Hafiz Zulkifly, et al. Predictors of Major lower limb amputation among type II diabetic patients admitted for diabetic foot problems. Singapore Med. J. 56: 626 – 631.
- Ahmad N, Thomas G.N, Gill P, Torella F. (2016). The prevalence of Major lower limb amputation in the diabetic and non-diabetic population of England 2003 – 2013. Diab. Vasc Dis. Res. B: 348 – 353.
- Kelly D.A, Pedersen S, Tosenovsky P, Sieunarines K. (2017). Major lower limb amputation: Outcomes are improving. Ann Vasc Surg. 45: 29 – 34.
- Ploeg A.J, Lardenoye J.W, Vrancken Pieters M.P, Breslau P.J. (2005). Contemporary series of morbidity and mortality after lower limb amputation. Eur. J. Vasc Endovasc Surg. 29: 633 – 637.