Compliance with directly-observed therapy short course regimen and recovery from pulmonary tuberculosis among clients of an infectious disease hospital
1Ekpeyong AU, PhD, 1Peters GE, PhD*, 2Nabuk NM, BNSC, 3Peters EJ, MD, FRCP (Edin)
Abstract
Background: The aim of this study was to assess the compliance with directly-observed therapy short course (DOTS)-regimen and recovery from pulmonary tuberculosis among clients of infectious Diseases Hospital, Ikot Ekpene, Nigeria.
Methods: A descriptive design was used for the study and a total of 100 pulmonary tuberculosis patients who came for medical checkup between August and September 2021 were studied using convenience sampling technique. The instrument used for data collection was a researcher constructed questionnaire with 20 items grouped into sections A and B. Section A, elicited information on the demographic data of the respondents while section B focused on the level of compliance and recovery rate of the patients. Data was analyzed using descriptive statistics of percentages on frequency tables and chart while Pearson product Moment Correlation formula was used to analyse the results at 0.05 level of significance.
Results: Findings from the study revealed that majority (72.2%) of the patients had knowledge, 70.6% complied with DOTS regimen and 68.2% recovered from pulmonary tuberculosis. There was no significant relationship between patient’s knowledge of the disease and compliance with DOTS.
Conclusion: It is therefore recommended that adequate information should be given to all pulmonary tuberculosis patients on the need for strict compliance with DOTS in order to recover completely from the infection after treatment.
Keywords: Compliance, Directly-observed therapy short course (DOTS), Recovery status, Pulmonary tuberculosis clients.
Introduction
Pulmonary tuberculosis is an infectious disease caused by Mycobacterium tuberculosis which is characterized by chronic cough, chest pain, haemoptysis amongst other symptoms. It is one of the leading causes of morbidly and mortality worldwide and remains a major public health burden1. The danger of this infection is an ever present one especially when it occurs as a co-infection in HIV/AIDS patients. Pulmonary tuberculosis is however cured by taking several antibiotics for at least six months but many patients fail to complete this treatment because of some social, cultural, medical and demographic barriers such as anti- tuberculosis drugs adverse reactions and lack of adequate knowledge about the disease and its treatment.
However, the world Health Organization (WHO) recommends a treatment strategy named “Directly observed Therapy short course” (DOTS) regimen to help people complete their treatments.1 DOTS is mainly responsible for ensuring that medications are made available on daily basis and also involves close monitoring to ensure that medications are taken as prescribed by keeping appointments with health workers. At the same time, DOTS is a medical regimen that needs strict compliance with its norms once it has been adapted to suit the lifestyle of the patients and their specific illness behavior. Ultimately, DOTS ensures that a health care worker or other individual watches the patient swallow every dose of the prescribed drugs.2 Non-compliance to DOTS could however arise due to many reasons such as some patients preferring to take their drugs at home without supervision in contrast to DOTS policy which recommends that the patient should be treated under observation. Also stigmatization could be a cause of non-compliance in which people are given negative social label and stigmatized because of the disease condition. Non-compliance could also occur due to the adverse reactions of anti-tuberculosis drugs. Considering the recovery status of pulmonary tuberculosis patients under DOTS, it is the best biomedical weapon in the fight against tuberculosis epidemics. At the same time, it allows identification of vulnerabilities and needs that can be dealt with during the process so as to overcome them. The WHO global tuberculosis report in 2012 stated that between the period 1995-2011, 51 million people were successfully treated for TB in countries that had adopted the DOTS and stop tuberculosis strategy.1
It is from the above premises that the researchers noted that compliance with DOTS is vital for the recovery of tuberculosis patients hence, the decision to assess the compliance with DOTS and recovery from Pulmonary tuberculosis among clients in Infections Diseases Hospital, Ikot Ekpene. Moreover, non-compliance by some patients with the regimen results in some patients developing drug resistant strains, thus making recovery from tuberculosis very difficult. Also, these patients become more infectious thereby increasing the chances of spreading the disease in contrast to the Government goal of reducing the spread of tuberculosis.
Methodology
Research design and population of study: Descriptive research design was used for the study. This design was chosen since it will provide an accurate quantitative description and also established the relationship between the dependent and independent variables. The sample population consisted of all 100 pulmonary tuberculosis patients who came for medical checkup after treatment in infectious disease hospital (IDH), Ikot Ekpene between August and September 2021 being one of the treatment centres for tuberculosis in Akwa Ibom state of Nigeria
Instrument for data collection: The main instrument for data collection was a researcher made questionnaire titled “Assessment of patients compliance with directly observed therapy short course (DOTS) regimen and recovery from tuberculosis among clients of infectious disease hospital” administered with the assistance of a trained nursing personnel. The questionnaire elicited information on demographic data, Assessment of knowledge of DOTS, Compliance and Recovery status.
Method of data collection: Data was collected using a structured questionnaire administered by the researcher and one trained assistant to the respondents in the hospital after obtaining necessary permission from the Medical Superintendent in-charge of the Hospital and written consent from the respondents. Completed questionnaire were retrieved by the researcher after administration each day with a return rate of hundred percent.
Method of data analysis: The data was analyzed using descriptive statistics. These include simple percentages, Frequency tables, and chart. Pearson product moment correlation formula was used to test the results obtained.
Results
Demographic data
Table 1: Demographic data of pulmonary tuberculosis patients who attended medical checkup in IDH, Ikot Ekpene
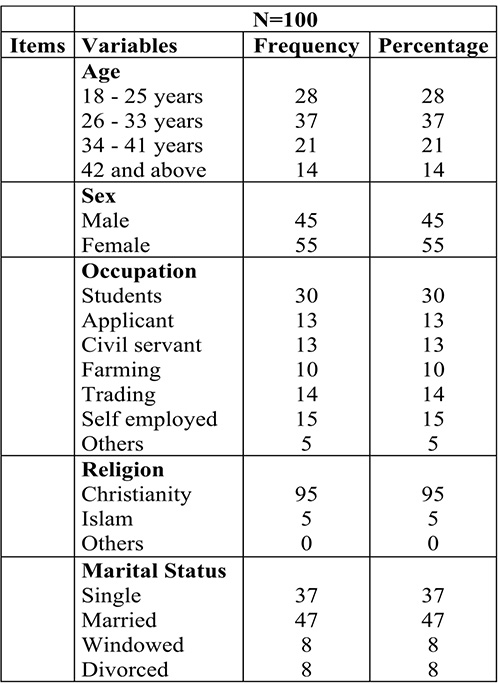
Table 1 indicates that, majority of the respondents 37 (37%) were within the age group of 34- 41, 55(55%) were female,while males were 45(45%). Thirty (30%) were students, 95 (95%) were Christians, while 47(47%) were married.
Table 2: Patient’s knowledge of DOTS
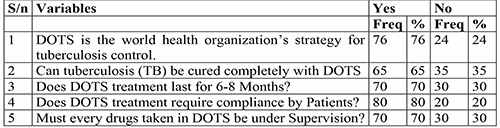
In table 2, the results showed that 76 (76%) respondents accepted DOTS as the world health organization’s strategy for tuberculosis control, 65 (65%) respondents accepted that TB can be cured completely with DOTS, 70 (70%) respondents acknowledged that DOTS treatment last for 6-8 months, while 80 (80%) respondents agreed that DOTS requires compliance by patients, and 70 (70%) respondents agreed that every drug taken in DOTS should be under supervision.
Table 3: Patient’s compliance to DOTS
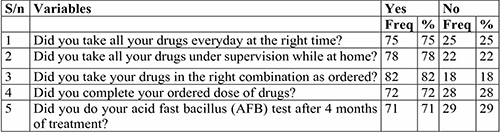
In table 3, the results showed patient’s compliance to DOTS. Seventy-five (75%) respondents agreed that they took their drugs everyday at the right time, 78 (78%) respondents accepted taking all their drugs under supervision, while 82(82%) respondents confirmed that they took their drugs in the right combination, 72 (72%) respondents accepted that they completed their ordered dose of drugs and 71 (71%) did their acid fast bacillus (AFB) test after 4 months of treatment.
Figure I: A multi-bar chart showing the recovery status of tuberculosis patients under DOTS
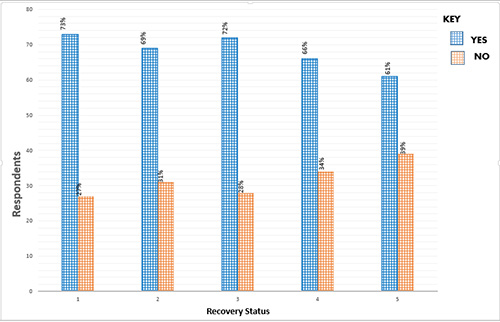
Figure I shows the recovery status of tuberculosis patients under DOTS in infectious disease hospital, Ikot Ekpene. The results revealed that 73(73%) respondents were relieved of their symptoms, while 27 (27%) were not relieved. Sixty-nine (69%) had their test result confirmed cured of TB after treatment, while 31 (31%) rejected. Seventy-two (72%) respondents had total relief of the signs and symptoms of tuberculosis (TB) after treatment while 28(28%) respondents did not. Sixty-six (66%) respondents suffered multiple drug resistant TB while 34 (34%) did not suffer. Lastly, 61 (61%) respondents gained weight after recovery from TB while 39 (39%) respondents did not.
Table 4: Pearson product Moment Correlation of relationship between knowledge and compliance of DOTS among clients of infectious Disease Hospital, Ikot Ekpene
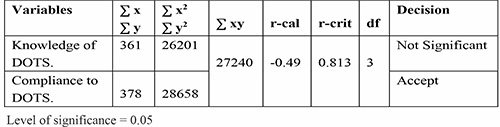
Findings in table 4 showed calculated value -0.49 at a degree of freedom 3. Since the calculated value -0.49 is less than the tabulated or critical value of 0.878, the hypothesis is accepted indicating that there is no significant relationship between knowledge and compliance with DOTS among clients of IDH, Ikot Ekpene. This means that although majority of the patients had knowledge of DOTS, they did not relatively comply to it in order to improve their recovery status.
Discussion
The findings from the study revealed that majority of the tuberculosis patients in Infectious Disease Hospital Ikot Ekpene had a good knowledge of DOTS treatment strategy. These findings are in contrast with the study conducted in India by Kaur et al,3 which showed that out of 100 clients, majority (66%) of the tuberculosis clients had inadequate knowledge, 31% had moderately adequate and only 3% of them had adequate knowledge on DOTS therapy. Similarly, the findings showed that majority of the pulmonary tuberculosis patients complied with DOTS regimen in infectious disease hospital, Ikot Ekpene. This finding is in consonance with the study conducted in Bombay, India by Nepali et al4 which showed that the overall compliance rate of patients to DOTS therapy was 86.8%. However, it is in contrast to Nepal’s view, who stated that despite the introduction of DOTS strategy to make tuberculosis services accessible at community level, there was still a high defaulting rate every year as about 5% of patients had defaulted from the treatment and the death rate due to tuberculosis was around 60%.5 The study also revealed that most patients were completely cured of tuberculosis while some of the patients recovered after suffering multiple drug resistant TB and a few others did not recover. This finding is in line with the study conducted by other workers6,7 which revealed that DOTS yielded more cure rate in the treatment outcome of pulmonary TB.
With regards to the hypothesis concerning patients level of education and compliance, it was tested with information on table 4 which showed that calculated value r = -0.49 was less than the tabulated value r = 0.878 at 0.05 level of significance. This indicated a lack of significance and acceptance of the hypothesis meaning that majority of the clients had knowledge of DOTS and still did not comply with it. The finding is in line with the study conducted by Mweemba et al8 which showed that there is no relationship between knowledge and compliance which suggested that knowledge is not a direct determinant of compliance. However, it is in contrast with the study conducted by Nepal et al5 which reported that patients compliance with TB treatment is associated with their knowledge and perception on the therapy.
Patient’s knowledge of DOTs.
Knowledge about a disease condition is seen to be the protective factor of defaulting to therapy. Some patients may not have necessary information or knowledge about DOTS therapy, as such might not comply with the regimen. Those who are already on treatment can be educated regarding treatment compliance so that treatment relapse can be reduced.3
In practice, lack of knowledge of DOTS regimen has been linked to ineffective physician- patient communication and in particular, physicians failure to assess, recall and comprehend the new concept with their patients.9 Consequently, language barriers contributes somewhat to this limitation. Healthcare providers need to explain the specific steps of the DOTS regimen, review most important details, use written instruction and encourage TB patients to ask questions about the regimen to enhance compliance.3
Therefore a patient centered individualized approach to treatment support is a core element to all TB control effort. More efforts should be made to enlighten people that TB is 100% curable and DOTS is a sure way of achieving the cure of TB.
Patients Compliance with DOTS
Patient’s choice in taking treatment is framed by the physiological, psychological and social/ cultural structures in which the person is immersed.10 Drug therapy for tuberculosis is very effective provided strict patient compliance can be ensured. Lack of knowledge about various aspects of TB and its treatment, toxicities of medication, and feeling better during treatment are also the contributing factors to non-compliance. Compliance to therapy is one of the important factors that affect the outcome of therapy. Improving patient’s compliance is of particular interest to all health care providers, and this is enhanced by several approaches and strategies taken to tackle the problem such as educating and counseling patients on their treatments regimen, good Nurse-Doctor-patient relationship, supply of free drugs, follow-up and monitoring of patients.11 According to the study conducted by Nepali et al4 on compliance to DOTS chemotherapy among the patients with pulmonary TB in Banke District of Nepal, patients were categorized into compliant or non-compliant categories by reviewing treatment carols. On the whole, it was discovered that alcohol drinking and negative/non–supportive family behaviours were significant factors affecting treatment compliance. The highest non-compliance was observed at the fourth month of treatment of TB and promoting supportive behaviours increased the compliance with DOTS therapy.
Recovery Status of Patients under DOTS
Regarding the importance of undertaking DOTS, evidence suggests that it is possible to achieve up to 90% cure rate when anti-tuberculosis drugs are correctly used. Supervised treatment is therefore an important strategy to not only ensure drug ingestion by the patients but also to promote adherence to treatment, increase chances of cure care and decrease the odds of probable drug resistance which seems to be major consequence in contexts of non-compliance by the patient.12 Since the adoption of the DOTS strategy and the stop TB partnership plan, many countries have seen a notable reduction in the number of TB cases and deaths related to TB. The WHO global TB report stated that 51 million people were successfully cured of TB in countries that had adopted the DOTS and stop TB strategy (out of a total of 60 million treatment.13 Tuberculosis mortality rate has decreased by 41% since 1990 and the world seems to be in the right path to achieve the global target of 50% anticipated reduction. However, TB incidence still remains high in some continents, such as Africa where the TB incidence rate increased from 245/100,000 inhabitants to 262/100,000.14 However according to Davidson et al,15 following successful completion of chemotherapy, cure should be anticipated in majority of patients. There is a small (<5%) and unavoidable risk of relapse which usually occurs within 5 Months after treatment and has the same drug susceptibility. HIV positive patients have higher mortality rates and a modestly increased risk of a relapse. Another study conducted by Eikomy, et al6 on the assessment of efficacy of DOTS for pulmonary tuberculosis, concluded that DOTS yielded more cure rate in the treatment outcome of pulmonary TB and decreases the rate of failure and defaulting. Also defaulting and non-adherence of the patients could be considered as important factors for increased incidence of failure in the treatment outcome of TB under DOTS.
Conclusion
Based on the above findings, it is obvious that patient’s compliance with DOTS improves their recovery status of tuberculosis but knowledge of DOTS does not necessarily increase their compliance. Thus, apart from creating awareness on DOTS, the need for strict compliance to DOTS should also be stressed when health educating the public on DOTS. It is therefore recommended that adequate information should be given to all tuberculosis patients on the need for strict compliance with DOTS in order to recover completely from tuberculosis infection after treatment.
References
- WHO. The Global tuberculosis control; surveillance. Global TB report. Geneva; WHO:1S-20
- Meulemans, H. The limits of patients’ compliance with DOTS for TB: A sociological perspective. Trop Pediatr 2009; 46:183- 954.
- Kaur B, Samuel P, Manpreet KG. A study to assess the knowledge regarding DOTS therapy among tuberculosis clients at TB Sanatorium in Amritsar; India: Mai Bhagi College of Nursing Journal Punjab. 2014; 4: 2249-4944.
- Nepali S. Tuberculosis in Bombay. New insights from urban poor patients. Health policy and planning.2009; 12 (1): 77- 85.
- Nepal AK, Siyalap K, Sermsri S, Keiwkamka B. Compliance with DOTS among tuberculosis patients under community based DOTS strategy in Palpa District, Thailand: Int J Infect Microbiol 2012;1 (1)14-19.
- Elkomy H, Awad M, El-shora A, Elshobeni B. Assessment of the efficacy of Directly observed treatment with shortcourse (DOTS) for pulmonary tuberculosis. Egyptian journal of chest disease and tuberculosis 2013; (8): 189-193.
- Inom AS Abebe F. (2014). Assesssment of defaulting from directly observed treatment short course (DOTS) and its determinate in Benin City, Nigeria. Journal of tuberculosis Research 2014;2: 30-39.
- Mweemba P, Haruzivishe C, Siziya S, Chipimo P, Christenson K. Knowledge, attitude and compliance with tuberculosis treatment, Lusaka Zambia. Medical journal of Zambia; 2008:35(4) 1-9.
- Hopewell. Advances in the diagnosis and treatment of tuberculosis. PROC AM thorax SOC 2009;3: 1-8.
- Buru J. Knowledge of tuberculosis and its management practice about tuberculosis and choice of communication channels in a rural community in Vietnam. Health policy 2008; 90 (1): 8-12.
- Hussein A. Factors influencing non compliance patients in some selected health institutions in Osun State, Nigeria (M.Sc thesis, OAU 2013, unpublished).
- Edmunds W, Jokes DJ. Who mixes with whom? A method to determine the contact patterns of adults that may lead to the spread of airborne infections PROC R SOC Lond 2010;264: 964-957.
- Volmink J. Systematic review of randomised controlled trials. Med J 2013;315:1403-1406.
- Cuneo A, Snide D. Effect to TB educating program on compliance to shortcourse chemotherapy among TB patients in sibuco Zambuanya, Phillipines: Medical School Foundation.2011;3: 5-9.
- Davidson J, Pandit N. Study of treatment compliance in DOTS for tuberculosis Indian Journal of community medicine.2015;2:(4)1-7.