Assisted Reproduction in Kano, North- Western Nigeria: A Four-year retrospective study
Abdullahi HM1, Egwuda K2, Suleiman M3, Warshu IH4, Ladan ZF5, Dayyabu AL1, Miko M6, Yusuf A7, Sheriff A8, Jibril A9
Abstract
Background: Infertility is a global problem and it poses severe physical and mental discomfort to the victims. Although considered a breakthrough, the assisted reproductive treatment of infertility such as in-vitro fertilization has been marred by a high failure rate even in technologically advanced societies.
Objective: This research was conducted to understand some of the factors that influence the outcome of in-vitro fertilization and embryo transfer (IVF & ET) and Intra-cytoplasmic sperm injection (ICSI)
Material and method: It is a 4-year retrospective study (April, 2017 to March 2021) which explored information from case notes of patients who underwent IVF& ET treatment at Getwell Fertility center. Information was collected and summarized using a specially designed proforma.
Results: It was discovered in this study that of the 109 IVF treatment offered, the 2 weeks pregnancy rate was 24 (22.9%), the Live birth rate was 19 (18.29%) and miscarriage was 5 (4.5%). The remaining 77.06% had failed procedures.
Conclusion: This study showed that advanced age above 32 years, and obese level of body mass index BMI, were the independent negative predictors of IVF success.
Introduction
Infertility is a global problem, and the absolute number of couples affected by infertility increased from 42.0 million 1990 to 48.5 million in 2010.1 It has been reported that up to 30% of the infertile couples are from the developing world.2 Infertility is a public health concern and associated with social, economic, and psychological effects. In some societies, the effects of infertility surpass childlessness alone, but a reason for stigma to the victims especially the women who suffer various negative behaviors towards them.3 In many of these communities, women are stigmatized, isolated, and become targets of psychological abuse or domestic violence.4 This negative behaviours are commoner in low resource countries, particularly in sub-Saharan Africa.4,5
The etiology of infertility is diverse with 40% coming from either of the couple while 20% emanate from both at the same time.5 Male factor infertility constitute 40% of all cases and mostly is due to moderate to severe abnormal sperm parameters. Female factor infertility on the other hand may be due to anatomical anomalies of the uterus, hormonal imbalance, and genetic anomalies.6,7
Assisted reproductive technology (ART) refers to any treatment or procedure that involves in vitro handling of human oocytes and sperm or embryos to establish a pregnancy.8,9 Since the first successful IVF procedure in 1978, the use of ART has expanded to become a routine around the globe.10 The procedures of assisted reproduction include; In-vitro fertilization and embryo transfer (IVF and ET), Intra-cytoplasmic sperm injection, Sperm/Oocyte/ Embryo donation, Zygote intra-fallopian transfer (ZIFT), Gamete intra-fallopian transfer (GIFT) and Surrogacy. Unfortunately, ART services remains out of reach to many infertile couples in the developing society not only due to the cost but the high failure rate that will require multiple treatment cycles.11,12 It has become imperative to improve selection process for ART treatment by clinicians, in order to improve the pre-procedure preparation of patients.
This study aims to determine the factors that affect outcome of assisted reproduction treatment of infertile couples in in Kano, northwest Nigeria.
Materials and method
It was a 4-year retrospective study (April 2017 to March 2021) of Assisted reproductive procedures carried out in Getwell Women and Children Hospital, which is a private hospital located in Ungoggo local government, Kano. The hospital operates for 24hours and attends to the health needs of women and children only. It is the only hospital that offers assisted conception in Kano presently. A total of 627 new cases of infertility were recorded during the period. Out of which 295 couples were qualified for assisted reproductive procedure, and only 109 (36.95%) were able to afford the procedure. Proper evaluation, adequate information, and informed consent were obtained from each couple. The protection of personal data and confidentiality were ensured.
Stimulation protocol
Down regulation was achieved using the long– GnRH agonist protocol for all patients. Ovarian reserve was assessed using serum anti-mullerian hormone (AMH), Antral follicular count (AFH). The synthetic Human Menopausal Gonadotropin was used to commence patients stimulation as a group with dosing tailored according to the perceived ovarian reserve at the dosage range of 150- 600iu daily. Serial trans-vaginal ultrasound scan was done to rule out early respondents and those with ovarian hyper-stimulation and the follicular size was used to determine the time of trigger using the Human chorionic gonadotropin. Oocyte retrieval was done approximately 24-36 hours after the trigger.
Embryology
Routine embryology protocols were observed, sperm preparations was achieved by the gradient method using the sperm grad and G-IVF-Plus media. Oocyte collection, equilibration and IVF were achieved using the G-Mops, and G-IVF-Plus media all media were purchased from Vitrolife (Sweden).
Day 3 embryo transfer was done for all patients and luteal support was achieved using synthetic progesterone analogue (cyclogest). A pregnancy test was carried out after two weeks.
Case notes of the patients that underwent assisted reproduction were retrieved from the medical records department of the hospital. Records of maternal age, type of infertility, duration, causes, body mass index, type of procedure, and pregnancy outcome were collected for analysis. Data collected were entered into statistical software (SPSS version 21.0) and analyzed. A test of association between Age and BMI with conception was conducted. Results were presented in tables and figures. Statistical significance was set at P ≤ 0.05.
Results and Discussion
Table 1: Socio-demographic characteristics of the participants
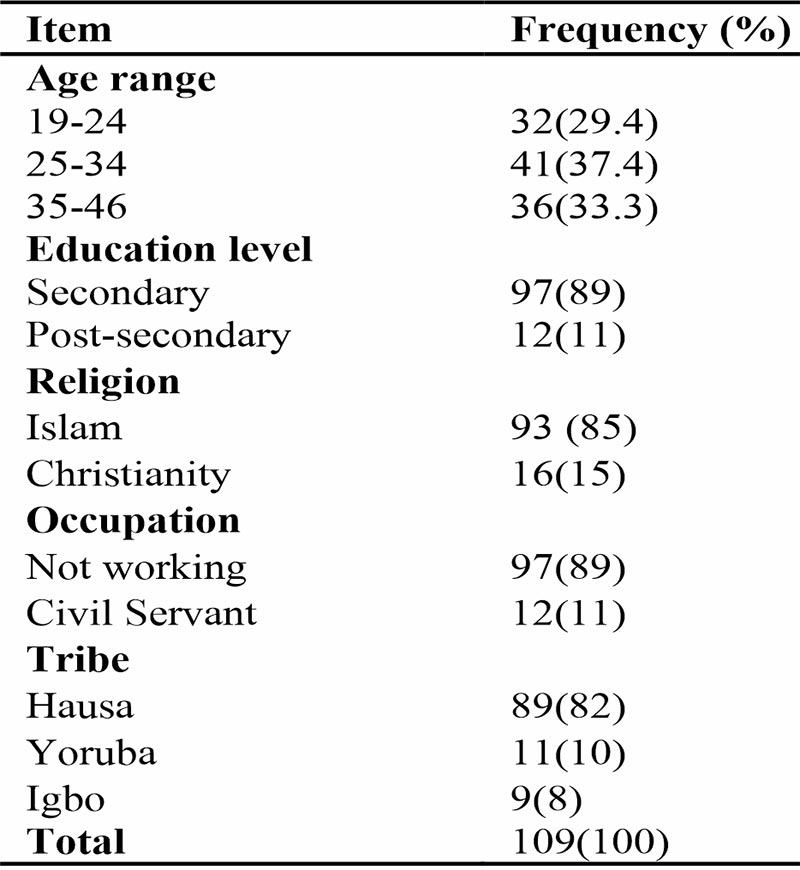
Table 2: Distribution of respondents according to the cause of infertility
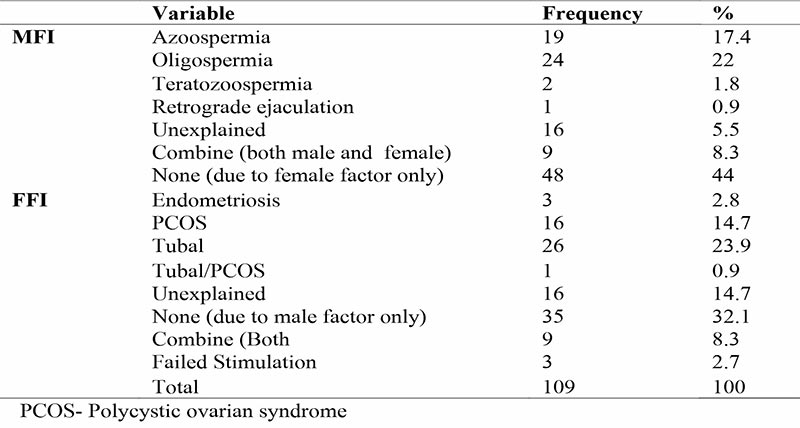
Table 3: Distribution of outcome of ART according to the Type of procedure

Table 4: Relationship between age, BMI and duration of on fertility and 2 weeks β-hCG positivity
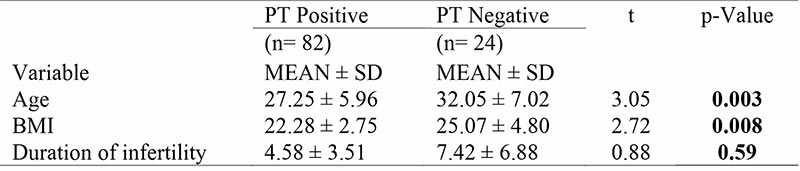
The age of the female partners ranges between 19 to 46years with a mean age of 30.12 ± 6.95years. Most of them (89%) had secondary education, were full-term housewives, Hausa by tribe, and predominantly Muslims (96%). The majority (74%) presented with primary infertility (table 1). The minimum duration of infertility among patients was between 2-20years with a mean duration of 7.5years (figure 1). Male factor contributed 40%, female factor 38%, combine factors 18%, and unexplained contributed only 4%. Severe Oligospermia is the leading cause of male infertility (72%) and tubal factor as the leading cause of female infertility (63%). Also 49% have a healthy weight. About 35% were overweight, and 16% were obese. A successful procedure was reported in 19 patients (17.43%). There is also a significant association between Age and conception (p< 0.00), and even Body Mass Index (BMI) and conception (p< 0.02).
A total of 162 couples were evaluated for ART, but only 109 (67.28%) were able to afford the procedure. Financial constraint is a major challenge surrounding ART.13-15 High costs of ARTs compared to the average local income, Lack of state support, and health insurance covering these expenses. Assisted reproductive technologies have become unaffordable and inaccessible for the average sub-Saharan African citizen.16-19 the age range of the female partners ranges between 19 to 46years with a mean age of 30.12 ± 6.95 years and a duration of between 2-20years with a mean duration of 7.5years (table 1). Research carried out in the United Kingdom in 2014 shows that the largest cohort receiving IVF treatments were women between 18 and 34, accounting for 43.4% of all cycles compared with 37% of those between 35 and 40.20 This finding is lower than that of women in southern part of Nigeria as reported by Sule et al, (2008) where the mean age of infertility was found to be 36.1 ± 6.6 years and mean duration of infertility of 7.3 ± 5.8 years. The lower mean age of in our study may be attributed to the sociocultural differences and health seeking behavior between the two regions. The mean age was also relatively advanced and this may be related to the well-documented reality that both women and men are less eager to seek for fertility treatment while they are young.18 Majority of subjects (74%) presented with primary infertility. This may be attributed to the cause of infertility. A study from Northeastern Nigeria also identifies primary infertility (58.7%) as the main type of infertility among couples that presented for assisted reproduction.18
Male factor contributed for 40%, female factor 38%, combine factors 18%, and unexplained contributed for only 4%. This finding is similar to the documented literature where Male factor infertility is shown to be responsible for about 40-50% of all infertility cases globally [19]. Severe Oligospermia is the leading cause of male infertility (72%) (table 2), while the tubal factor is the leading cause of female infertility (63%), followed by polycystic ovarian syndrome PCOS (32%).
Of the 109 ART procedures, 19 persons had ICSI, and 90 had IVF + ET. The overall live birth rate was 22.9% with and almost half of all those with ICSI had a successful pregnancy compared to those with IVF+ET. The overall miscarriage was 4.5%. Women who had ICSI had higher ODD of positive pregnancy rate, and live birth rate (table 3). This is lower than 41/104 (39.4%) reported in Ilorin.18 180/600 (30%), and 31/115 (27%) reported in Nnewi and Benin southwestern and eastern Nigeria, respectively.19,20 Studies from tropical countries reported a success rate of 28.3%, reduced to13.9% in patients with poor ovarian reserve.21 Studies from developed countries showed a success rate of between 42-54%.21-23 Our finding is however higher than the 16.2% and 18.3% reported in Nnewi and Benin city.19,20 The odds of having a successful pregnancy was almost 6 times when ICSI is used compared to when IVF+ET is done (OR 6.73 95% CI 2.13-12.46).
Also, 50% were single pregnancies, and 50% were multiple gestations from our study with twins accounting for 40% and triplets for 10%. Day three transfer and transfer of multiple embryos in a single cycle increase the rates of multiple births.23 A rate of 11.8% was reported from Ilorin18 6.6%, and 8.7% obtained in Benin and Nnewi, Nigeria, respectively.19,20 Elective single embryo transfer (eSET) was found to reduce the incidence of multiple gestations.24 Studies from Nigeria showed that over 94% of infertile couples preferred the transfer of multiple embryos because they see multiple pregnancies as compensation for their infertility.25 Ectopic pregnancy was reported in one (2.17%) patient with tubal factor infertility in our study. Other studies reported an incidence of ectopic pregnancy to be 1.6% when one embryo was transferred among fresh, non-donor cycles, 2.2% – 2.5% with two or more embryos.26 Risk factors for ectopic pregnancy were zygote intrafallopian transfer (ZIFT), tubal factor infertility, and endometriosis, rather than male factor infertility.27
There is a significant association between Body Mass Index (BMI) and conception (p< 0.02). Advanced maternal age, Obesity, and longer duration were associated with lower chances of live birth rate following IVF/ICSI in this study (table 4). This was similar to the previous studies [28,29] where it was shown that women with a BMI of more than 25kg/m2 have a lower chance of conception following ART procedures, require a high dose of gonadotropins that have a high risk of Abortion.30,31 Likewise, advanced maternal age types of infertility and duration of infertility were shown to affect the live birthrate in ART.18,32
Conclusion
This study showed a slightly higher prevalence of male factor infertility when compared to female factor and a high failure rate of IVF in Northern Nigeria. Also, advanced maternal age, BMI, and long history of infertility were negative confounders of ART treatment. We recommend more in-depth research to understand the reasons for the high failure rate of ART in our environment.
References
- Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12): e1001356. doi: 10.1371/journal.pmed.1001356
- Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14(6):605–621. doi:10.1093/humupd/dmn042
- Tabong PT, Adongo PB. Infertility and childlessness: a qualitative study of the experiences of infertile couples in Northern Ghana. BMC Pregnancy Childbirth. 2013;13:72. Published 2013 Mar 21. doi:10.1186/1471-2393-13-72
- Araoye MO. Epidemiology of infertility: Social problems of the infertile couples. West Afr J Med 2003;22:190-6.
- Cong J, Li P, Zheng L, Tan J. Prevalence and Risk Factors of Infertility at a Rural Site of Northern China. PLoS One. 2016;11(5):e0155563. Published 2016 May 13. doi:10.1371/journal.pone.0155563
- Ombelet W, Cooke I, Dyer S, Serour G, Devroey P. Infertility and the provision of infertility medical services in developing countries. Hum Reprod Update. 2008;14(6):605–621. doi:10.1093/humupd/dmn042
- Giwa-Osagie OF. The need for infertility services in the developing world: the WHO point of view. GynecolObstet Invest. 2004;57(1):58.
- Zegers Hochschild F, Adamson GD, Mouzon J, Ishihara O, Mansour R, Nygren K, et al. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) Revised Glossary on ART Terminology. Human Reproduction 2009;24:2683 7
- Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, Barfield WD; Centers for Disease Control and Prevention (CDC). Assisted Reproductive Technology Surveillance — United States, 2012. MMWR SurveillSumm. 2015 Aug 14;64(6):1-29.
- Adamson GD, Tabangin M, Macaluso M, De Mouzon J. The numbers of babies born globally after treatment with the assisted reproductive technologies (ART). FertilSteril 2013;100:S42.\
- Luke B. Pregnancy and birth outcomes in couples with infertility with and without assisted reproductive technology: with an emphasis on US population-based studies. Am J Obstet Gynecol. 2017 Sep;217(3):270-281. doi: 10.1016/j.ajog.2017.03.012. Epub 2017 Mar 18
- Chambers G. M.,. Sullivan E. A, Ishihara O., Chapman M. G., and. Adamson G. D`, “The economic impact of assisted reproductive technology: a review of selected developed countries,” Fertility and Sterility, 91;(6). 2281–2294, 2009.
- Omurtag K R K. R. Omurtag, A. K. Styer, D. Session, and T. L. Toth, “Economic implications of insurance coverage for in vitro fertilization in the United States: a review,” J Reprod Med, 2009;.11(12); 661–668,
- Griffiths A, Dyer SM, Lord SJ, et al. A Cost effectiveness analysis of in-vitro fertilization by maternal age and number of treatment attempts. Hum Reprod. 2010; 25:924–31.
- Ombelet W and Campo R. (2007). Affordable Invitrofertilization for developing countries, Reprod Biomed Online, , vol. 15; 257 - 265.
- Sule JO, Erigbali P, Eruonom L (2008). Prevalence of infertility in women in a Southwestern Nigerian community. Afr Biomed Res;11:225-7.
- Pierce, Nicolea; Mocanu, Edgar. Female age and assisted reproductive technology. Global Reproductive Health: June 2018 – 3(2) e9doi:
- Lukman O O, Abdulwaheed O O, Kabir A D, Sekinat T R, Sikiru A B and Ganiyu A S. Assisted reproduction technology: Perceptions among infertile couples in Ilorin, Nigeria. Saudi Journal of Health Sci. 2017. 6 (1); 14-18.
- Orhue AA, Aziken ME, Osemwenkha AP, Ibadin KO, OdomaG.In vitro fertilization at a public hospital in Nigeria. Int J GynaecolObstet 2012;118:56-60.
- Ikechebelu JI, Eleje GU, Ibadin K, Joe-Ikecheelu NN. Outcome of in vitro fertilization procedure at a private fertility center in Nnewi, South-East Nigeria. Afr J Infertil Assist Concepts 2016;1:2-5.
- Wang AY1, Safi N2, Ali F3, Lui K3, Li Z2, Umstad MP4, Sullivan EA2. BMC Pregnancy Childbirth. Neonatal outcomes among twins following assisted reproductive technology: an Australian population-based retrospective cohort study. 2018 Aug 8;18(1):320.
- Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, Barfield WD; Assisted Reproductive Technology Surveillance — United States, 2012. Centers for Disease Control and Prevention (CDC). MMWR SurveillSumm. 2015 Aug 14;64(6):1-29.
- Maheshwari A, McLernon D. Bhattacharya S. Cumulative live birth rate: time for a consensus? Hum Reprod. 2015 ; 30 : 2703 – 2707.
- Oloyede OA, Iketubosin F, Bamgbopa K. Spontaneous fetal reduction and early pregnancy complications in multiple pregnancies following in vitro fertilization. Int J Gynaecol Obstet. 2012 ; 119 : 57 – 60.
- McLernon, K. Harrild, C. Bergh “Clinical effectiveness of elective single versus double embryo transfer: meta-analysis of individual patient data from randomized trials,” BMJ, 341 c6945, 2010.
- Okohue JE, Onuh SO, Ikimalo JI, Wada I. Patients’ preference for number of embryos transferred during IVF/ICSI: a Nigerian experience. Niger J ClinPract. 2010. 6(13):294–297.
- Okohue JE, Ikimalo JI, Omoregie OB. Ectopic pregnancy following in vitro fertilisation and embryo transfer. West Afr J Med. 2010a; 29 : 349 – 351.
- Chang HJ. Ectopic pregnancy after assisted reproductive technology; what are the risk factors? CurrOpinObstetGynaecol. 2010;22(3);202-207.
- Brugh, V. M and Lipshultz, L. I. Male factor infertility: Evaluation and management. Medical Clinics of North America 2004; 88, 367-385.
- Cooper TG, Noonan E, Von Eckardstein S, Auger J, Baker HW, Behre HM, Haugen TB, Kruger T and Wang C (2009). "World Health Organization reference values for human semen characteristics". Hum Reprod Update. 16 (3): 231–45.
- Antonio M, Juan ES, Javier AC, FernandoZH. Outcome of assisted reproductive technology in overweight and obese women. JBRA Assist Reprod. 2017 Apr-Jun; 21(2): 79–83.
- Bellver J, Ayllón Y, Ferrando M, Melo M, Goyri E, Pellicer A, Remohí J, Meseguer M. Female obesity impairs in vitro fertilization outcome without affecting embryo quality. FertilSteril. 2010; 93:447–454.
- Chavarro JE, Ehrlich S, Colaci DS, Wright DL, Toth TL, Petrozza JC, Hauser R. Body mass index and short-term weight change in relation to treatment outcomes in women undergoing assisted reproduction. FertilSteril. 2012; 98:109–116.]
- Omokanye LO, Olatinwo AW, Biliaminu SA, Durowade KA. Successful pregnancy outcome after in vitro fertilization at a public health facility in Nigeria. J Med InvestigPract 2014; 9:157-9.