Pattern of Haematological Indices Among Pregnant Women at Booking in Murtala Muhammad Specialist Hospital, Kano
Murtala Yusuf1, Badriyya Aliyu Darma2
Abstract
Background: Haematological changes are some of the physiological events that occur in pregnancy. A proportion of women die each year as a result of pregnancy complications related to hematological profile alterations. This study observed the haemoglobin level, white blood cell and platelets counts of pregnant women and their association with sociodemographic factors.
Objectives: To determine the pattern of haematological indices of pregnant women at booking in Murtala Muhammad Specialist Hospital and to determine the sociodemographic characteristics that affect haematological indices among the women.
Methodology: The study was a cross sectional study of 256 pregnant women who booked for antenatal care at Murtala Muhammad Specialist Hospital Kano. The sociodemographic information of the women was obtained using an interviewer administered questionnaire. About 3mls of venous blood was collected from each of the clients and put into an ethylenediaminetetraacetic acid (EDTA) bottle; a full blood count analysis was then run on the samples.
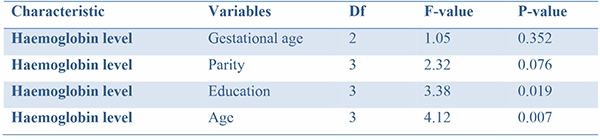
Results: The mean values for the different indices were: WBC 5.31 ± 2.68 x109/L, Haemoglobin level was 10.59 ± 1.13 g/dl and Platelet count was 208.4 ± 6.07 x109/ L. Majority of the clients were anaemic (68.35%), thrombocytopenia was found in 27.3%, and 40.63% had leucocytopenia. Statistical test of association using one –way ANOVA found no association between haemoglobin level and gestational age and no association between haemoglobin level and parity. However there were associations between haemoglobin level and age of the clients, and haemoglobin level and educational status.
Conclusion: Significant proportion of women in this study were anaemic at booking and had no formal education; this demonstrates the need for awareness of the general public for the girl child education and women empowerment.
Keywords: Anaemia, leucocytopenia, pregnancy, booking, Kano
Introduction
Haematological indices reflect to a large extent the overall health status of an individual, however those indices are affected by pregnancy in order to meet up the demand of the developing foetus and placenta.1,2 Haematological changes are also some of the major factors affecting pregnancy and its outcome.3 Anaemia, thrombocytopenia and leukocytosis are some of the observed changes in pregnant women from various parts of the world.4
Pregnancy is associated with a lot of physiological changes in the circulatory system which otherwise will be considered pathological; for this reason it is of utmost importance to have reference values for each locality as factors such as genetics, socio economic and cultural factors may play a role in causing variations.5,6
The major concern about the adverse effects of anaemia and other haematological changes on pregnant women is the greater risk of perinatal morbidity and mortality.7 World wide an estimate of 58.27 million women are anaemic during pregnancy, and the major burden lies in developing countries including Nigeria; this has significantly been associated directly or indirectly with the maternal mortality in these regions.8 Anaemia in pregnancy is defined by WHO as a haemaglobin concentration below 11g/dl, and it remains a major problem in developing countries. It is associated with increased rates of maternal and perinatal complications such as preterm delivery, low birth weight, and sepsis.9-12
Red blood cells increase in pregnancy to approximately 30% between 12-26th week of gestation to complement the plasma increase of 25-80% between 6-24th week of gestation. This discrepancy is responsible for the physiological anaemia seen in pregnancy. However, in late pregnancy the plasma volume increases at a slower rate inducing a slight rise in haematocrit.2,3
Platelet aggregation is increased and a decrease in the number of circulating platelets with gestation has been observed in normal pregnancies. Increased consumption of platelets in the uteroplacental circulation has been suggested to be the explanation of the reduction in the number of circulating platelets.3,14
White blood cell count is increased in pregnancy as a result of physiologic stress induced by pregnant state.15 Lymphocyte count decreases during the first and second trimesters and increases during the third trimester. Monocytosis occur in 7th to 20th week of gestation and this increase help prevent fetal allograft rejection by infiltrating the decidual tissue. Values of basophils and eosinophils do not change significantly in pregnancy.1,3,15
Objectives:
1. To determine the pattern of haematological indices of pregnant women at booking in Murtala Muhammad Specialist Hospital.
2. To determine the sociodemographic characteristics that affect haematological indices among pregnant women in Murtala Muhammad Specialist Hospital.
Materials and methods
Study population: The study was carried out in the Department of Obstetrics and Gynaecology of Murtala Muhammad Specialist Hospital, Kano. It is a general hospital located in the ancient city of Kano; it has about a thousand hospital beds with 17 departments and 14 clinics. It has the busiest Obstetrics and Gynaecology department in Kano State with about 14000 deliveries recorded in 2018. The hospital receives client not just from Kano State but also from nearby states such as Jigawa, Kaduna and Katsina State.
Study design: The study was a cross sectional study of 270 pregnant women who attended Murtala Muhammad Specialist Hospital for antenatal care booking between November and January 2018. Approximately 300 women meet the inclusion criteria. The women were recruited using simple random sampling. Pregnant women not willing to give consent, those with medical conditions, those on medications that could affect blood counts such as antibiotics, anticoagulants or steroids were excluded from the study. Clients who consented to participate in the study were interviewed with interviewer administered questionnaire to obtain their sociodemographic information such age, parity, education level, occupation, and gestational age at booking. Blood samples were then collected from each of the participants.
Sample collection: A medical laboratory technician served as a research assistant in the study and assist the researchers in sample collection. Using a 5mls syringe, a blood sample of 3mls was collected from the antecubital vein of each client after sterile swab was used to clean the site. The sample was then put into an EDTA bottle. A dry swab was used to apply pressure to the vein after collection and the bottle was labeled. After each day’s collection, the samples were transported to the laboratory often within 2 hours. The samples were analysed in the laboratory on the day of collection by laboratory scientists.
Analysis of samples: An automated Sysmex Haematology Analyser XP 300 was used to auto-analyse the samples. It runs 12 parameters per sample. The standard calibration of the machine was set and each processing was done according to the manufacturer’s instruction and guidelines. Approximately 0.2ml of sample was aspirated by the sample probe into the machine which analysed the sample and the results were displayed on the monitor. Results were printed immediately on a thermal printing paper.
Data analysis: The data obtained was analysed using MINI TAB 18 statistical software. Both quantitative and qualitative variables were summarised. Mean and standard deviations were calculated for the qualitative variables while percentages and frequencies were used for the quantitative variables. Statistical test of association was calculated for haemoglobin against age, parity, educational level and gestational age. A statistical level of significance was P<0.05 using a one –way Anova.
Using WHO “haemoglobin concentration for the diagnosis of anaemia and assessment of severity” anaemia was graded as follows; mild 10 - 10.9g/dl, moderate 7.0 - 9.9g/dl,13 and severe less than 7g/dl. Normal range for Platelet count was 150 – 450 x 109/L,14 and for Leucocytes it was 4 -11 x 109/L.15
Results
Table 1: Sociodemographic characteristics
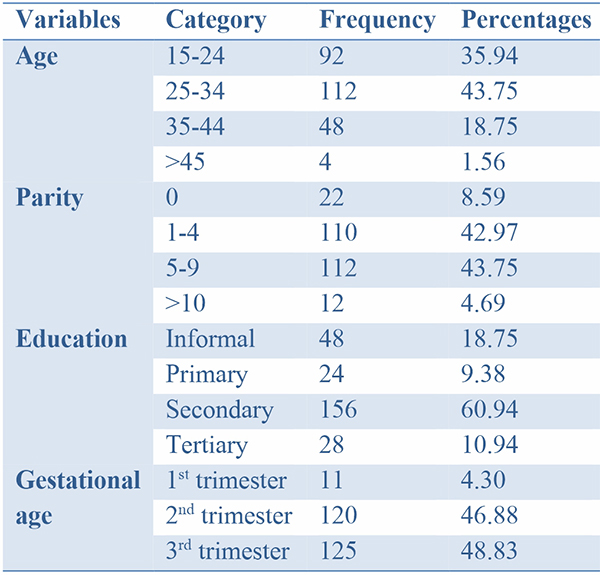
Table 2: Descriptive Statistics of white blood cells, haemoglobin and platelets
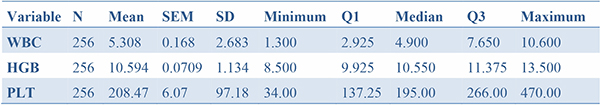
Where N is sample size, SEM: standard error of the mean, SD: standard deviation, Q1 and Q3: quartile ranges
The mean Haemoglobin was 10.95 ± 1.13g/dl, while the mean of WBC was 5.30 ± 2.68x109/L. the mean for platelet count was 208.47 ± 97.18x109/L. The minimum haemoglobin level was 8.5g/dl and the maximum was 13.5g/dl.
Table 3: Haemoglobin level across trimesters
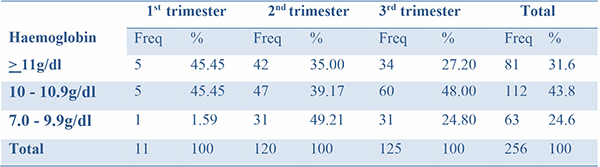
Out of the 256 women, only 31.64% had normal haemoglobin level, 43.75% had mild anaemia while 24.61% had moderate anaemia. There was no patient with severe anaemia in this study.
Table 4: Thrombocyte count
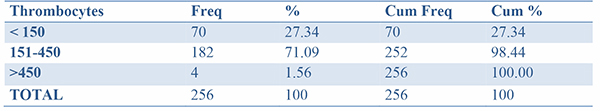
Cum freq: cumulative frequency, cum %: cumulative percentage
Thrombocytes count was found to be within normal range in 182 (71.09%) clients, while 70 (27.34%) had thrombocytopenia and 4 (1.56%) had thombocytosis.
Table 5: Leucocyte count
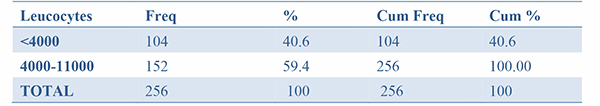
The result of leucocytes count was found to be normal in almost 60% of the clients while leucopenia was found in 40.6%. There was no case of leucocytosis.
Table 6: Association between anaemia and gestational age
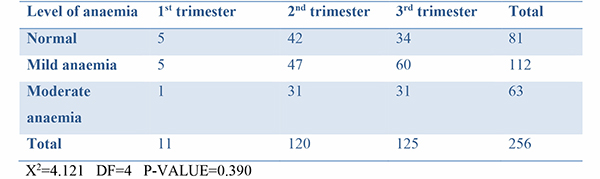
Table 7: Association between anaemia and parity
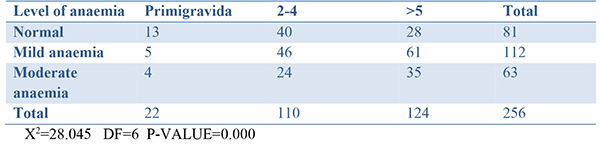
Table 8: Association between anaemia and educational status
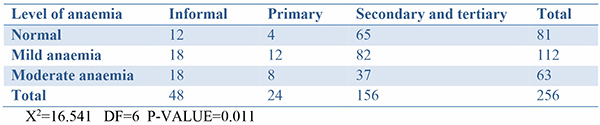
Secondary and tertiary columns were merged because a cell was empty (moderate anaemia and tertiary level of education). The statistical test of association using degree of anaemia and gestational age showed no association, but education and parity were found to be significantly associated with haemoglobin levels.
Table 9: Summary of one-way ANOVA for haemoglobin against gestational age, parity, age and educational level
Analysis of Variance
Null hypothesis: All means are equal
Alternative hypothesis: Not all means are equal
Significance level: α = 0.05
Equal variances were assumed for the analysis.
Blood samples of 270 women were collected but only that of 256 clients were analysed; this was because 6 samples coagulated before arrival in the laboratory and 8 results obtained from the automated machine were incomplete. The mean age of the booked women was found to be 28.19 ±7.32. the age range was 16-47 years. Majority of the women were parous 234 (91.4%) while only 22 were primigravidas (8.59%). The women were mostly formally educated up to secondary school certificate(60.94%) and 10.94% had tertiary level of education; however only 4.30% presented for booking at first trimester, 46.88% and 48.83% presented for booking at second and third trimester respectively.
Discussion
This study found that women attending antenatal clinic in Murtala Muhammad specialist Hospital booked late with 46.8% and 48.8% booking in 2nd and 3rd trimester, only 4.3% booked in the first trimester. It was also found that only 10% of the women in this study were educated up to tertiary level. This was found to be lower than the study done in 2009 at Aminu Kano Teaching Hospital were the study found women booking in 2nd trimester to be 65%, and about 41% were educated to tertiary level.8 The difference might be due to the fact that Murtala Hospital was a general Hospital while Aminu Kano Hospital was a tertiary centre, and is usually attended by those of higher socioeconomic status. This finding of early booking was also found in another study at a tertiary hospital by Akinkabi et al in Lagos where majority of the women booked in 2nd trimester and were educated up to tertiary level of education.3
The mean haemoglobin level was found to be 10.59g/dl ± 1.13, mean WBC count was 5.3x109 ± 2.6/L and mean platelets count was 208.4x109 ± 6.01/L, this was similar to the findings of Akinkambi et al except that, the mean WBC was higher in their study. In this study, 68.36% of the patients were anaemic at booking. This contrasts with 32% of patients who had anaemia at booking in a similar study in Gombe.16
In this study, there was an increase in WBC at booking, this is comparable to the findings in Delta State where pregnant women when compared to controls showed an increase in WBC.2 The leucocytosis seen in pregnancy is likely due to consequences of selective immune tolerance, immunosuppression and immunomodulation of foetus.17
This study also showed a slight reduction in platelet count which was similar to most other studies, in Libya the mean platelet of control group was higher than that of pregnant women, and this decrease progressed with increase in trimester.18 Some women have statistically abnormal platelets count while having no demonstrable abnormality, but thombocytopenia or thombocytosis is an indication of abnormality, hence the need for further screening in such patients.19 Large cross sectional studies done in pregnancy of healthy women in India have shown platelets count does decrease during pregnancy especially in 3rd trimester (gestational thrombocytopenia), partly due to haemodilution and partly due to increase platelet activation and accelerated clearance.15
There appears to be a statistically significant association between level of anaemia with parity, educational level and gestational age (p-value <0.005) but no statistically significant association with patients age; this finding is similar to the study carried out in Aminu Kano Teaching Hospital and at Dawakin Kudu general hospital.8,20
The limitations of this study was the fact that it was a facility based study and might not be a true reflection of the population, a large proportion of the women who do not attend ANC would have been missed.
Conclusion:
Anaemia at booking was found in a significant number of clients in this study, leucocytopenia was also observed in a portion of the women, so also thrombocytopenia. High proportion of women booked for antenatal care during second and third trimester of the pregnancy. Also majority of the clients had no formal education. Therefore, there is need for community enlightenment about the importance of early booking for antenatal care. There is also a strong need for girl child education and women empowerment.
References
- Gebreweld A, Bekele D, Tsegaye A. Haematological Profile of Pregnant Women at St. Paul’s Hospital Millennium Medical Collage. Addis Ababa Ethiopia. BMC Hematol.2018;5: 121-129
- Ichipi-ifukor PC, Jacobs J, Ichipi-ifukor RN, Ewrhe OL; Changes in Haematological Indices in Normal Pregnancy. Physiol J 2013. http://dx.doi.org/10.1155/2013/283814
- Akinbanmi A, Ajobola SO, Rabiu KA, Adewunmi A, Dosunmu AO, Adediran A, et al. Haematological Profile of Normal Pregnant Women in Lagos, Nigeria. Int J Women Health. 2013;(5):227-232.
- Micheal OA, Theresa OA, Tyodoo MM. Haematological Indices of Nigerian Pregnant Women. J Blood Lymph. 2017(7):159
- Akingbola TS, Adewale IF, Adesina OA, Afolabi KA, Fehintola FA, Bamboye FA, et al. Haematological Profile of Healthy Pregnant Women in Ibadan, South Western Nigeria. J Obstet Gynaecol. 2006;26(8): 763-769.
- Chaudhari SJ, Bodat RK. Are there any Difference in Haematological Parameters in Pregnant and Non-Pregnant Women? Ntl J Comm Med 2015; 6(3):429-432.
- Allen LH. Anaemia and Iron Deficiency: Effects on Pregnancy Outcome. Amer J Clin Nutr. 2000;71(5):1280-1284
- Nwizu N, Ilyasu Z, Ibrahim SA, Galadanci HS. Socio-Demographic and Maternal Factors in Anaemia in Pregnancy at Booking in Kano, Northern Nigeria: Afri J Repro Health 2011;15(4):33-41.
- Shridevi. Study of Prevalence of Anaemia Among Pregnant Women Attending Antenatal Check-up in Rural Teaching Hospital in Telangana, India. Int J Reprod Contracept Obstet Gynaecol. 2018;7:2612-2616.
- World Health Organisation (WHO) The prevalence of Anaemia in women: a tabulation of available information. Geneva, Switzerland: WHO;1992.WHO/MCH/MSM/92.2.
- El Guindi W, Pronost J, Carles G, Largeaud M, El Gareh N, Montoya Y, et al. Severe Maternal Anaemia and Pregnancy Outcome. J Gynecol Obstet Biol Reprod, 2004;33(6):506-509.
- Allen LH. Anaemia and Iron Deficiency: Effect on Pregnancy Outcome. Am J Clin Nutr 2000:71(5)128-132.
- WHO. Haemoglobin Concentration for Diagnosis of Anaemia and Assessment of Severity, Vitamin and Mineral Nutrition Information System, Geneva, World Health Organisation 2011 (WHO/NHH/NHD/MNM/II)
- Juan P, Stefano G, Antonella S, Albana C. Platelets in Pregnancy. J Prenat Med. 2011:5(4):90-92.
- Chandra S, Tripathi A, Mishra S, Amzarul M, Vaish AK. Physiological Changes in Haematological Parameters During Pregnancy. Indian J Haematol Blood Transf. 2012; 28(3) :144-146.
- Vander jagt DJ. Nutritional Factors Associated with Anaemia in Pregnant Women in Northern Nigeria, J Health Popl Nutr.2007;25(1):75-81.
- Li A, Yang S, Zhang J, Qiao R. Establishment of Reference Intervals for Complete Blood Count Parameters During Normal Pregnancy in Beijing. J Clin Lab Anal.2017;31(6)
- Azab AE, Albasha MO, Elhemady SY. Haematological Parameters in Pregnant Women Attended Antenatal Care at Sabratha Teaching Hospital In Northwest, Libya. Amer J Lab Med.2017;2(4):60-68.
- Juan P, Stefano G, Antonella S, Albana C. Platelets in pregnancy. J Prenat Med. 2011;5(4):90-92.
- Imam TS, Yahaya A. Packed Cell Volume of Pregnant Women Attending Dawaki Kudu General Hospital, Kano State, Nigeria. Int J Pure App Scs.2008;2(2):46-50.