Prevalence and determinants of medical errors among early career doctors in Nigeria
Kehinde Kanmodi1,2, Abdulmajid Yahya3, Shehu Umar4, Ugo Enebeli5, Oladimeji Adebayo6, Olayinka Ilesanmi7,
Ugochukwu Eze8, Mumeen Salihu9, Shuaibu Ibrahim10, Kabir Durowade11, Taiwo Alatishe12,
Dabota Yvonne Buowari13, Oluwatobi Osasona14, Godiya Dare Ishaya15
Abstract
Objectives: This study aimed at investigating the prevalence and determinants of medical error involvement among early career doctors (ECDs) in Nigeria.
Material and methods: This study was a post-hoc analysis of a descriptive cross-sectional questionnaire-based survey of 460 ECDs in 14 hospitals spreading across Nigeria.
Results: The mean (±SD) age of the surveyed respondents was 32.6 (±5.7) years and 312 were males. Seventy-six respondents (16.5%) had been involved in medical error before, of which 38.1% of them indicated that they were involved in such error about 0 to 1 year ago. Bivariate analysis showed a statistically significant relationship between the place (Nigeria versus foreign) of respondents’ undergraduate medical/dental training and their status regarding involvement in medical error only (p = 0.048). However, multivariate analysis showed no statistically significant (p-values>0.05) relationship between the relevant characteristics of the respondents and their involvement in medical errors.
Conclusion: This study affirms that medical error involvement is not an uncommon event among ECDs in Nigeria. Importantly, serious efforts need to be committed towards reducing the rate of medical errors among ECDs.
Key words: medical error; early career; resident; medical doctor; dentist; Nigeria
Introduction
Medical errors are preventable human errors resulting from medical care, whether or not it is evident or harmful to the patient.1,2 Medical error is defined as a failure to achieve planned actions (errors of execution) or using wrong plans to attain an objective (errors that result due to planning).3 Medical errors are a significant cause of mortality and morbidity. The World Health Organization (WHO) estimates that medical errors are one of the top ten causes of death and disability worldwide, particularly in low and middle income countries (LMICs) where 134 million healthcare associated adverse events occur contributing to 2.6 million deaths annually.4 Consequently, the World Health Assembly in May 2019 adopted the resolution to ensure patients’ safety from medical errors and established September 17 as the World Patient Safety Day.4
Among healthcare professionals, medical errors are found to be common among doctors.5 Early career doctors (ECDs) are medical or dental practitioners who are resident doctors, medical/dental interns, or medical officers below the rank of principal medical officers and dental equivalents.6 ECDs are a vulnerable population of doctors whose early experience shapes their future behaviour and responses to medical error.7 Thus there is need to focus on this group for effective prevention and mitigation of medical errors. Though it has been argued that medical errors are inevitable in almost all healthcare settings and that virtually all doctors have made mistakes but generally under-report them (the concept of “to err is human”).5,8 However, the Hippocratic dictum states “above all, do no harm”;9 and patient safety is a basic right that should always be ensured during patients contacts with health care settings.10
In the United States (US), it is recently estimated that medical errors may account for 251,000 deaths annually, making it the third leading cause of death.11 A population-based study of 6,586 US physicians showed that 691(10.5%) reported a major medical error in the prior 3 months.12 These medical error rates are significantly higher in the US than in other developed countries such as Canada, Australia, New Zealand, Germany and the United Kingdom, even though less than 10 percent of medical errors are reported.13 Among developing countries, Pakistan reported that among 130 postgraduate resident doctors, 128(98.5%) had encountered a medical error among whom 103(86%) had disclosed their errors.5
In Africa, many countries do not properly report the data on medical errors and minimal risk for physicians to lose their licenses due to poor controls.14 However, some studies on the subject have been conducted. In a study of 77 health workers in Uganda, 41(53.2%) reported that medical errors occurred.15 A systematic review of 51 studies from nine African countries reported 8.4% prevalence of adverse drug events from medication errors.16
In Nigeria, a national survey of 2,386 health professionals reported a prevalence of self-reported medication errors of 47%.17 In Ondo State, a study of 95 health professionals reported that medication errors were found more commonly among junior doctors and nonmedical doctors; and only 1.6% of the errors were detected and corrected during the process of dispensing.18 Another study in Abia State reported a medical error rate of 42.8% among 145 medical doctors and committal of medical errors was significantly associated with less than ten (10) years of practice.1
In all, medical errors can be fatal, debilitating and economically draining to all parties; and need to be urgently addressed. An investigation into the prevalence and determinants of medical errors will help in policy making and implementation geared towards curbing the menace of medical errors in Nigeria. This study therefore aimed to investigate the prevalence and determinants of medical error involvements among the ECDs in Nigeria – a group of doctors who historically have been more prone to medical errors.
Materials and methods
Study Type
This was a descriptive cross-sectional study conducted to investigate the prevalence and determinants of medical error involvements among ECDs in Nigeria. This study forms a part of the Phase II projects of the CHARTING (Challenges of Residency Training and Early Career Doctors in Nigeria) Study.6,19,20 At large, the CHARTING Study is a multi-centre, and hospital-based major research project which studies the medical, economic and psychosocial issues affecting ECDs across Nigeria.6,19,20 Furthermore, this study was a post-hoc analysis.
Study Protocol
The protocol of the CHARTING Study – Phase II, of which this current study forms a part of it, had been earlier described in literature.20
Study Instrument
The study instrument for this current study was a seven-section paper questionnaire which forms a part of the piloted CHARTING Study – Phase II questionnaire.20 The questionnaire has 39 items which obtained the following information from the participating ECDs: socio-demographic characteristics (Section 1; 9 items); history of engagement in medical errors (Section 2; 2 items), personal health issues using the Patient Health Questionnaire – 9 [PHQ9] (Section 3; 9 items), and anxiety-related issues using the Generalized Anxiety Disorder Questionnaire – 7 [GAD7] (Section 4; 7 items), clinical performance self-rating (Section 5; 5 items), self-rating on current job (Section 6; 5 items), and working hours (Section 7; 2 items).
Study Sites
The study sites were some selected hospitals across five, out of six (north-west, north-east, north-central, south-west, south-south, and south-east), geopolitical zones in Nigeria (Table 1). Participating hospitals were selected using multistage sampling technique.
Sampling
The sampling (sample size determination and sample selection) processes adopted in this study has been well-described in “Niger J Med. 2019;28(2):198–205”.20
Data Collection
The data collection process was carried out between July 2020 and May 2021. A total of 460 ECDs, selected using multistage sampling technique, participated in this study.
Data Analysis
The data obtained from the 460 ECDs were computed and analyzed using the Statistical Package for Social Sciences (SPSS) Version 23 software. The frequencies and proportions of all variables (discrete and continuous), and means and standard deviations (SD) of all continuous variables were determined. Chi-square (χ2) test, Man-Whitney U test, and student T (t) test were used in determining bivariate associations between variables of interest. Multivariate regression analysis was also done on various factors as seen in Table 5A, 5B, and 5C.
Ethical Considerations
This study was conducted with strict compliance with the provisions obtained in the Helsinki Declaration regarding health-related studies on human participants. Prior to the study, we obtained ethical approval from the National Health Research Ethics Committee (NHREC). Prior to participation, all the recruited ECDs were informed about the aims and objectives of the study; they were also informed that their participation in the study is strictly voluntary and confidential, and that they have the freedom to opt out of the study if peradventure they are unwilling to continue participation in the study. Before they were issued a questionnaire to fill, written informed consent was obtained from each of the consenting participant. Data collected were anonymous and analysis was done with strict adherence to confidentiality.
Result
The completeness rate for the study was >70%, i.e. all the respondents responded to at least 27 (≥70%) items in the 39-item questionnaire.
Table 1: Distribution of respondents based on geopolitical zones and centres
[caption id="" align="alignnone" width="600"]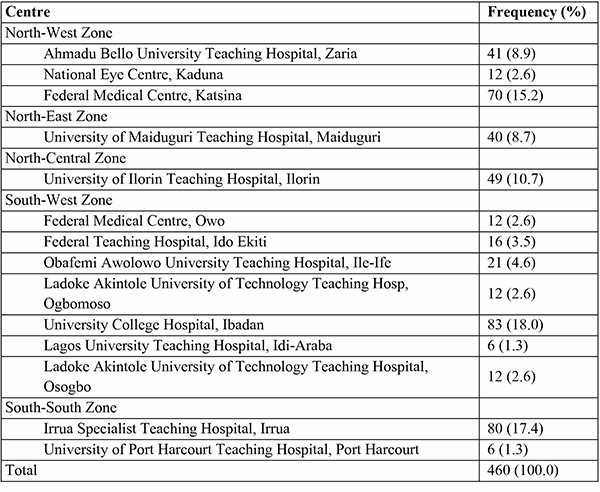 Table 1 depicts the distribution of the respondents based on affiliated centre (i.e. hospital) and geopolitical zone in Nigeria.[/caption]
Table 1 depicts the distribution of the respondents based on affiliated centre (i.e. hospital) and geopolitical zone in Nigeria.[/caption]
Table 2: Characteristics of the respondents
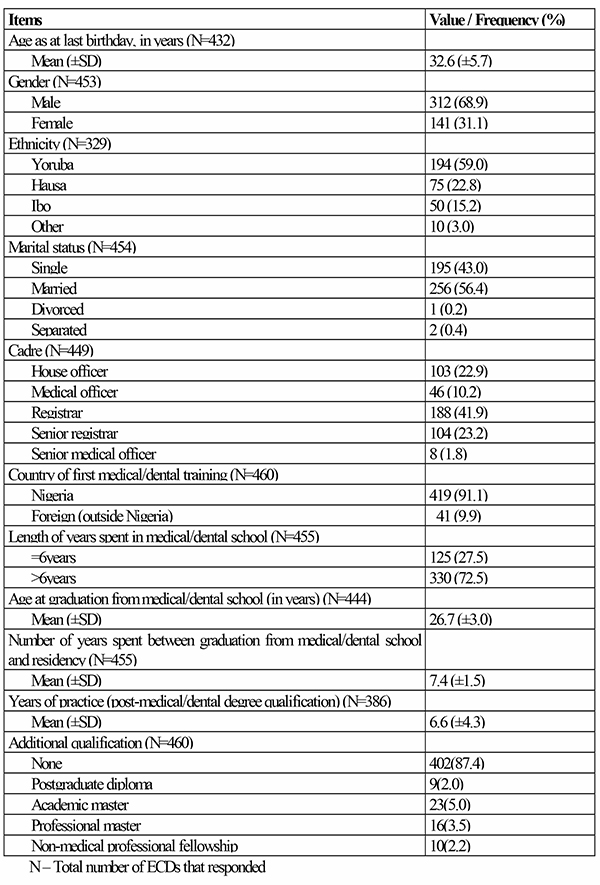
Table 2 depicts the characteristics of the 460 respondents (with “N” designating the total number of respondents that responded to an item in the table). Three hundred and twelve respondents (N=453; 68.9%) were males, 194 (N=329; 59.0%) were from the Yoruba ethnicity, 256 were married (N=454; 56.4%), 188 (N=449; 41.9%) were registrars, 419 (N=460; 91.1%) were Nigeria-trained, 330 (N=455; 72.5%) spent >6 years in medical/dental school, and only 23 (N=460; 5.0%) had an academic master degree. The mean (±SD) age of the respondents as their last birthday was 32.6 (±5.7). The mean (±SD) age of graduation from medical/dental school was 26.7 (±3.0). Other information are also available in the table.
Table 3: Prevalence of medical error involvement among the respondents
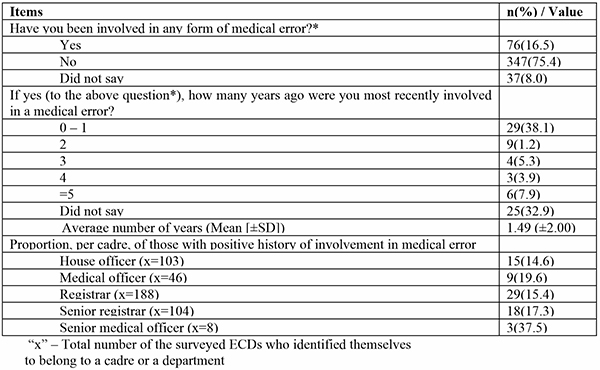
Table 3 provides information regarding the prevalence of medical error involvement among the respondents. Seventy-six (76/460; 16.5%) respondents reported that they had been involved in medical error before, of which 38.1% (29/76) of them indicated that they were involved in such error about 0 to 1 year ago. The senior medical officers (37.5%; 3/8), medical officers (19.6%; 9/46), and senior registrars (17.3%; 18/104) were the top three cadres of the respondents that had a positive history of involvement in a medical error.
Table 4: Cross – tabulations for bivariate analysis
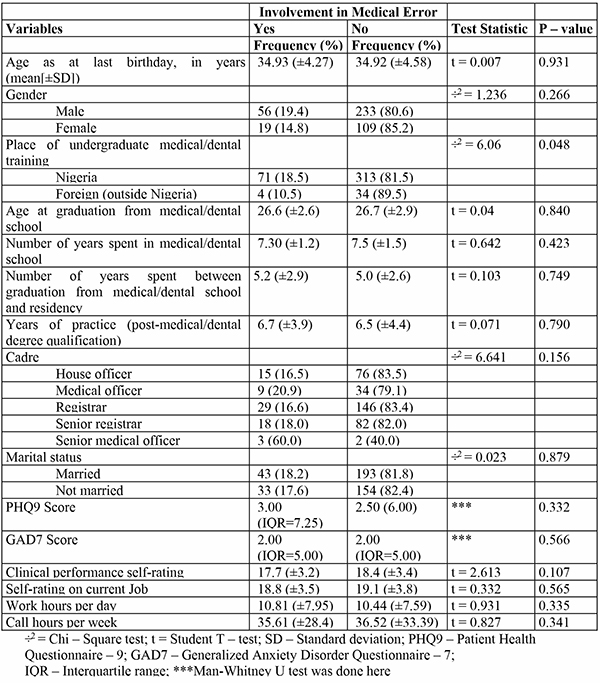
Table 4 presents noteworthy comparisons among the respondents with respect to their status regarding involvement in medical error, socio-demographic characteristics, personal health issues, and anxiety-related issues. Respondents’ age as at last birthday, gender, age at graduation from medical/dental degree, number of years spent in medical/dental school, number of years spent between graduation from medical/dental school and residency, years of practice after medical/dental degree qualification, and all other characteristics were found to have no statistically significant relationship (p>0.05) with the their status on medical error involvement except for the place (Nigeria versus foreign) of respondents’ undergraduate medical/dental training, which was found to be statistically significant (p = 0.048).
Table 5a: Multivariate regression analysis (model A)
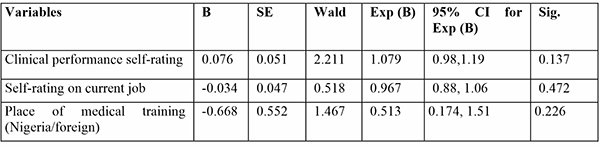
Table 5b: Multivariate regression analysis (model B)
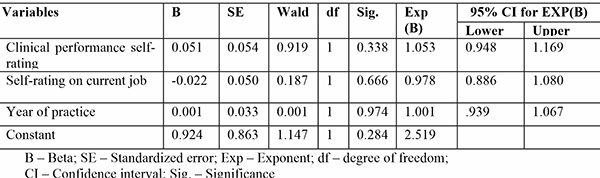
Table 5c: Multivariate regression analysis (model C)
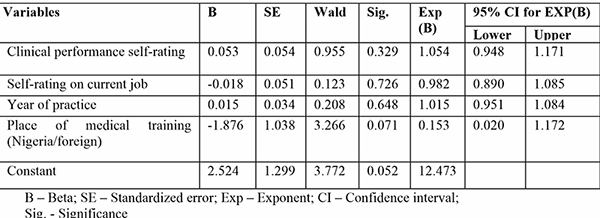
Tables 5a, 5b, and 5c depict regression models A, B, and C respectively. In the regression models, no statistically significant (p-values>0.05) relationship was obtained between the characteristics of the respondents and their involvement in medical errors.
Discussion
Medical error is a global phenomenon and it is an umbrella term for errors committed in relation to medical care.11,21-23 According to literature, medical errors exist in different kinds. They include “surgical error”, “diagnostic error”, “medication error”, “tubing misconnection”, “device and equipment error”, “iatrogenic infection”, “fall”, “information technology-related error”, “communication error”, and others.24
Medical error is one of the major causes of deaths among patients.11 Pertinently, medical errors are preventable errors; the avoidance of such error can salvage the life of a patient and improve the quality/outcome of patient care. The need for the prevention and control of medical errors in patient care cannot be over-emphasized, as this will help reduce the incidence rate of disability and deaths in the society. In a developing African nation like Nigeria, there is a dearth of credible literature exploring “medical error” as a thematic research area. This observation birthed the idea of conducting this present study to explore the prevalence and determinants of medical error involvement among ECDs in Nigeria.
The findings obtained in this study are noteworthy. The prevalence of medical error involvement in this study was low (16.5%); this prevalence is lower than that reported among a population of adults (18.8%) in Iowa, USA, but far lower than that reported among staffers and medical students of Nemazee Hospital (Shiraz, Islamic Republic of Iran) (95.8%) and residents of Massachusetts, USA (23%).21-23 Based on these comparisons, it can be affirmed that medical error involvement/experience is a differing phenomenon among diverse population groups.
About four out of every ten respondents indicated that they were involved in a medical error within the past 0 to 1 year, whereas the frequencies of involvement in such event was lower in older years (i.e. >1 year). This observation can be attributed to recall bias, as some respondents might not be able to completely recall events of such in past years.
It is also important to note that some respondents decided not to respond to items that enquired about their involvement in medical errors. Based on the study scope, it is difficult to ascertain why this category of respondents refused to respond to such items. However, can this refusal to respond be due to fear of reporting such, lack of trust in the investigators or some other reasons best known to them? To the best of authors’ capacity, all participating ECDs were assured that their participation and data will be kept with strict confidentiality; hence, this rules out the issue of lack of investigator-subject trust. Nonetheless, this observation calls for the need to deeply investigate, using mixed research methods, why ECDs may be unwilling to report confidential information pertaining to medical errors. Due to the non-response rate observed, it is difficult to rule out that all the surveyed ECDs had comprehensive knowledge of what medical error entails. Hence, all ECDs in Nigeria need to be comprehensively educated about medical error as a medical phenomenon.
It was observed that the respondents categorized under the lowest cadre – house officer cadre – had the lowest proportion of persons with positive history of medical error involvement while those categorized under the senior medical officer cadre (one of the highest cadres) had the highest proportion. However, this is not too surprising; the more the years spent in medical practice, the more the expected possibility of involving in medical errors and possibly being more relaxed to acknowledge an error. This is most probably the reasons for this variance. More so, house officers are under strict supervision, they always seek guidance of their seniors (trainers) before carrying out any task, so risk of medical error may be low among them. While some senior medical officers may or may not be under any supervision, most especially in general hospitals and some may feel they are well grounded to take decisions without seeking any second opinion or liaising with senior colleagues thus putting them at risk of medical errors. Nonetheless, this shows the need for meticulous mentorship with more dedication to training by trainers as improved skill will benefit ECDs, their trainers and patients. Minimizing medical errors will also reduce the litigation burden ECDs and their superiors will be exposed to.
It is noteworthy that the place of medical/dental degree training is significantly associated (at the level of bivariate analysis) with respondents’ status on medical error involvement. The category of those respondents who acquired their medical/dental degree overseas reported relatively lower rate of medical error involvement when compared to those that acquired such degree domestically. However, after subjecting this interesting finding into multivariate analysis, it was found that the place of the respondents’ training is not an independent predictor of involvement in medical error; nonetheless, this finding does not completely rule out the need to investigate why a significant relationship of such exists at bivariate analysis level in a higher powered study.
This study has its limitations. First, this study did not explore the types of medical errors which the respondents were involved in; hence, this study did not ascertain the medical error patterns which the surveyed ECDs were involved in. Second, this study did not explore all cadres of medical doctors and dentists (such as consultants and principal medical officers). Also, other health professionals (such as nurses, dieticians, physiotherapists, pharmacists, laboratory scientists, etc.) were excluded from this study; hence, this study fails to provide relevant data on these categories of persons. This second limitation is due to the limited scope of the study. Third, this study reported past experience of its respondents; hence, the possibility of recall bias cannot be ruled out. Hence, the data presented in this study is an estimated data which may not be an absolute representation of the respondents’ experience.
Notwithstanding these limitations, this study has its strength. This study is believed to be the first study to explore the associations between medical error involvement, mental health, and occupational health of ECDs in Nigeria at a closely nationally representative scale. This study reported the first scientific attempt to generate a more representative data on the Nigeria as ECDs in 5 out of the 6 geopolitical zones in Nigeria were captured. Even though it may appear that ECDs working in the South-eastern zone of Nigeria did not participate in the study, 15% of the respondents who volunteered their ethnicity were of South-eastern extraction though working in other zones of the country which still gave the zone some amount of representation. This study was also largest multicentre study on issues unique to ECDs.
Conclusion
This study affirms that medical error involvement is not an uncommon event among ECDs in Nigeria. Also, ECDs that received their first medical/dental degree training domestically are more prone to medical error involvements. There is a need for further investigative studies to explore the pattern of medical errors among ECDs. Importantly, more serious efforts need to be committed towards reducing the rate of medical errors among ECDs; if more efforts are committed towards this, the incidence rate of disability and deaths in Nigeria will reduce and the quality and outcome of medical care services in Nigeria will improve to a significant extent.
Funding
This study was funded by the Nigerian Association of Resident Doctors (NARD), Nigeria formerly called National Association of Resident Doctors (NARD), Nigeria.
Conflicts of interest
None of the authors have any competing interest to declare except all are ECDs except OI, UE, and KD. GDI is a national officer of NARD.
References
-
Iloh G, Chuku A, Amadi A. Medical errors in Nigeria: A cross-sectional study of medical practitioners in Abia State. Arch Med Heal Sci. 2017;5(1):44–9.
-
Ahmed Z, Saada M, Jones AM, Al-Hamid AM. Medical errors: Healthcare professionals’ perspective at a tertiary hospital in Kuwait. PLoS One. 2019;14(5):e0217023.
-
Reason J. Human error. Cambridge: Cambridge University Press; 1990. 90 p.
-
World Health Assembly. Global action on patient safety. Seventy-Second World Heal Assem [Internet]. 2019;22(10):809–15. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA72/A72_R6-en.pdf
-
Bari A, Khan RA, Rathore AW. Medical errors; causes, consequences, emotional response and resulting behavioral change. Pakistan J Med Sci. 2016;32(3):523–8.
-
Adebayo O, Ogunsuji O, Olaopa O, Kpuduwei S, Efuntoye O, Fagbule O, et al. Trainees collaboratively investigating Early Career Doctors: A NARD initiative in Nigeria. Niger J Med. 2019;28(1):93–7.
-
Mankaka CO, Waeber G, Gachoud D. Female residents experiencing medical errors in general internal medicine: a qualitative study. BMC Med Educ. 2014;14:140.
-
Brownlie K, Schneider C, Culliford R, Fox C, Boukouvalas A, Willan C, et al. Medication reconciliation by a pharmacy technician in a mental health assessment unit. Int J Clin Pharm. 2014;36(2):303–9.
-
Smith CM. Origin and uses of primum non nocere--above all, do no harm! J Clin Pharmacol. 2005;45(4):371–7.
-
Kim I-S, Park M, Park M-Y, Yoo H, Choi J. Factors Affecting the Perception of Importance and Practice of Patient Safety Management among Hospital Employees in Korea. Asian Nurs Res (Korean Soc Nurs Sci). 2013;7(1):26–32.
-
Makary MA, Daniel M. Medical error - the third leading cause of death in the US. Brit Med J. 2016;353:i2139.
-
Tawfik DS, Profit J, Morgenthaler TI, Satele D V, Sinsky CA, Dyrbye LN, et al. Physician Burnout, Well-being, and Work Unit Safety Grades in Relationship to Reported Medical Errors. Mayo Clin Proc. 2018;93(11):1571–80.
-
Anderson JG, Abrahamson K. Your Health Care May Kill You: Medical Errors. Stud Health Technol Inform. 2017;234:13–7.
-
Camara ME, Camara N, Camara AY, Traore F. Healthcare settings: the best ways to mitigate errors. Int J Community Med Public Health2016;3(1):380-384.
-
Mauti G, Githae M. Medical error reporting among physicians and nurses in Uganda. Afr Health Sci. 2019;19(4):3107–17.
-
Mekonnen AB, Alhawassi TM, McLachlan AJ, Brien J-AE. Adverse Drug Events and Medication Errors in African Hospitals: A Systematic Review. Drugs - real world outcomes. 2018;5(1):1–24.
-
Ogunleye OO, Oreagba IA, Falade C, Isah A, Enwere O, Olayemi S, et al. Medication errors among health professionals in Nigeria: A national survey. Int J Risk Saf Med. 2016;28(2):77–91.
-
Babatunde KM, Akinbodewa AA, Akinboye AO, Adejumo AO. Prevalence and pattern of prescription errors in a Nigerian kidney hospital. Ghana Med J. 2016;50(4):233–7.
-
Kanmodi K, Ekundayo O, Adebayo O, Efuntoye O, Ogunsuji O, Ibiyo M, et al. Challenges of residency training and early career doctors in Nigeria study (charting study): A protocol paper. Niger J Med [Internet]. 2019;28(2):198–205.
-
Eze UA, Tolani MA, Adeniyi MA, Ogbonna VI, Isokariari O, Igbokwe MC, et al. Challenges of residency training and early career doctors in Nigeria Phase II: Update on objectives, design, and rationale of study. Niger J Med 2020;29(4):714-719.
-
Lind DP, Andresen DR, Williams A. Medical Errors in Iowa: Prevalence and Patients' Perspectives. J Patient Saf. 2020 Sep;16(3):e199-e204.
-
Askarian M, Sherafat SM, Ghodsi M, Shayan Z, Palenik C, Hatam N, Enchev Y. Prevalence of non-reporting of hospital medical errors in the Islamic Republic of Iran. East Mediterr Health J. 2020;26(11):1339-1346.
-
Hibbard JH, Peters E, Slovic P, Tusler M. Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Rev. 2005;62(5):601-16.
-
Rodziewicz TL, Houseman B, Hipskind JE. Medical Error Reduction and Prevention. [Updated 2021 Aug 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499956/